Abstract
Intracranial involvement in multiple myeloma patients takes up around 1%, and is usually known to be present in the parietal bone or skull base in cases of skull vault involvement, while it presents in the dura and parenchyma in cases of intracranial involvement. Primary pachymeningeal invasion is even rarer with extremely rapid progression and very poor prognosis. It is our intent to report a case in which we had to differentiate multiple myeloma with other metastatic tumors, lymphoma, and leukemia with intracranial involvement. Our patient showed an osteolytic lesion of the skull with dural involvement and subdural mass formations.
While involvement of the pachymeninges by various malignancies is well known, intracranial involvement of multiple myeloma (MM) is very rare, taking up only 1% of all MM patients. Intracranial mass formation is much rarer (1). Pachymeningeal MM is known to have a very poor prognosis with rapid progression (2). We experienced a rare case of direct intracranial involvement, rather than involvement through the cerebrospinal fluid (CSF), which formed a subdural mass with osteolytic lesions of the skull and required differential diagnosis from lymphoma, leukemia, and other metastatic diseases. It is our intent to present a case report of the imaging findings and literature review.
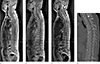
A 53-year-old female was admitted with lower back pain which started a month ago. On admission, a blood laboratory test revealed decreased WBC (3970/uL), RBC (1.95 × 106/uL), Hb (5.8 g/dL) and hematocrit (18.4%). Spine MRI was taken to assess the intractable lower back pain. The patient's spine MRI (Fig. 1) revealed diffuse heterogeneous signal intensity of vertebral bodies on T1 weighted images (T1WI) and T2 weighted images (T2WI), and homogeneously enhancing posterior epidural masses at the level of T4-5 and T10-12 on the contrast enhanced T1WI, resulting in the patient's hospitalization with an impression of multiple metastases or multiple myeloma. There was no evidence of bony destructive changes on the spine CT images.
Surgery was planned to treat the nerve compression symptoms due to the epidural vertebral masses. During the preoperative additional tests to evaluate the cause of low Hb, a sudden change in mental status occurred. Non-contrast enhanced brain CT and gadolinium enhanced brain MRI were performed.
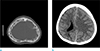
Non-enhanced brain CT showed multifocal osteolytic lesions of the skull bones (Fig. 2a).
Also, a diffuse and high attenuated subdural lesion at left fronto-parietal convexity was noted, simulating acute subdural hematoma (Fig. 2b). On the brain MRI of the patient, the hyperdense subdural lesion in the left frontoparietal convexity of the brain CT, reveals iso signal intensity as the cerebral cortex on T1WI (Fig. 3a) and T2WI (Fig. 3b) and fluid-attenuated inversion recovery (FLAIR) images (Fig. 3c), as well as diffuse heterogeneous enhancement along the thickened dura mater on enhanced T1WI (Fig. 3d, e). The patient underwent emergency craniectomy. There was a gross jelly-like tissue covering the subdural space and tumor bleeding occurred during the operation. The epidural mass in the thoracic level was removed to decompress the spinal cord. Post-operative pathologic report confirmed a diagnosis of λ-chain plasma cell myeloma.
The patient showed drowsy mentality during conservative management and the follow-up brain CT revealed a large hematoma in the operation bed. Consecutive emergency hematoma evacuation was conducted without evidence of active bleeding. Because of her poor general condition and drowsy mental status, radiotherapy and chemotherapy were put on hold. At the 30th day of admission when her C-reactive protein (CRP) level was elevated (28.55 mg/dL) by combined Clostridium difficile colitis, aspiration pneumonia, influenza B infection. On the 36th day of admission, the patient expired.
MM represents a neoplastic proliferation of plasma cells from a single clone. The tumor and its products result in multi-organ failures and symptoms, including bone pain and fracture (70%), recurrent infections (~25%), renal failure (25%), anemia (80%), hypercalcemia, blood coagulation abnormalities, and neurologic symptoms (3). When MM invades the skull or cranium, it usually involves the skull bone, skull base, nose, and paranasal sinus while direct intracranial involvement is rare and primary dural or pachymeningeal involvement is even rarer (4). The location of the MM may be inside or outside the bone marrow, and depending on the stage of disease progression, may be a single or multiple lesions. Primary extramedullary plasmacytoma is rare and takes up about 4% of all plasmacytomas, and as the periosteum is avascular structure, it is generally the case that the disease spreads through the adjacent bone lesion first (2). On the other hand, dural invasion of MM shows a prevalence of about 1-5% (456), and Roddie et al. (7) explains how the myeloma cells pass through the veins of the arachnoid membrane, destroy the arachnoid trabeculae, and mix into the CSF, and that infiltration into the central nervous system (CNS) occurs around a few months to 2 years after diagnosis (2). Recently, as the survival time of MM patients increases, the incidence of pachymeningeal or dural involvement also increases (8), while the radiologic or disease-specific clinical findings have rarely been reported. Dural or pachymeningeal involvement may be local, multiple, or diffuse and needs to be differentiated from infectious meningitis or metastasis of other tumors. In MM with dural or pachymeningeal involvement, the disease progression is known to be very rapid with an unfavorable prognosis, as in this case, in which the time interval from the symptom onset to patient's death was about 2 months. The patient eventually died of a compromised immune system with complicated infections, including aspiration pneumonia probably due to deteriorated mental status, as a result of MM complications.
MM with dural involvement shows high attenuation on unenhanced CT, similar to meningioma or subdural hematoma, and is known to present as a lesion distributed around the periphery (6). However, the tumor tissue shows iso to high signal intensity on the T1WI, and iso to low signal intensity on the T2WI, thus with clinical information, these findings may help differential diagnosis from meningioma or subdural hematoma.
According to the previous reports, MM shows strong enhancement of the involved dura or pachymeninges on both brain and spine CT and MRI (5), high signal intensity on diffusion weighted images (DWI), and low value on the apparent diffusion coefficient (ADC) map (2). Nevertheless, there aren't any clearly defined radiologic findings of MM with high diagnostic specificity, and the diagnosis is usually established through past diagnosis of MM, clinical findings and CSF studies, and confirming myelomatosis in the dura through surgical pathology (2). In this study, there were no abnormal findings in the skull base and paranasal sinus, which are known to be commonly involved in cases of intracranial involvement. The subdural mass showed iso signal intensity similar to that of the cerebral cortex on T1WI, T2WI, and FLAIR images, with homogeneous enhancement. Additionally, there were multiple typical osteolytic lesions of skull and soft tissue mass formation around the spine, which increased the possibility of MM but wasn't specific enough to completely rule out metastasis from other tumors. Also, the osteolytic lesion of the left parietal bone formed a soft tissue mass that engulfed small osseous fragments thought to be a sequestrum (Fig. 2a). Therefore, although rare, the possibility of intracranial involvement of a lymphoma or osteosarcoma, and chloroma seen in myelogenous leukemia could not be ruled out.
In conclusion, diagnosis of MM involving multiple organ is still a challenging subject to radiologists. As the survival time of the patients increases, the incidence of pachymeningeal involvement, which is known to be rare in current literature, also increases. Therefore, when faced with a case suspicious for MM but with atypical features, it would be exemplary to consider the possibility of MM and advise the clinician for further work-up on MM.
Figures and Tables
Fig. 1
Whole spine MR and CT images of a 53-year-old female patient. The spine MR images (a-c) show diffuse heterogeneous signal intensity of vertebral bodies on both T1WI and T2WI. Homogeneously enhancing posterior epidural masses at the level of T4-5 and T10-12 also noted on the contrast enhanced T1WI (c). The whole spine CT image shows no evidence of bony destructive changes (d).
References
1. Terada T. Multiple myeloma presenting as an intracranial plasmacytoma: a case report. Cases J. 2009; 2:9110.
2. Cerase A, Tarantino A, Gozzetti A, et al. Intracranial involvement in plasmacytomas and multiple myeloma: a pictorial essay. Neuroradiology. 2008; 50:665–674.
3. Munshi NC, Longo DL, Anderson KC. Plasma cell disorders. In : Longo DL, Fauci AS, Kasper DL, editors. Harrison's principles of internal medicine. 18th ed. New York: The McGraw-Hill Education;2011. p. 936–944.
4. Schluterman KO, Fassas AB, Van Hemert RL, Harik SI. Multiple myeloma invasion of the central nervous system. Arch Neurol. 2004; 61:1423–1429.
5. Pizzuti P, Pertuiset E, Chaumonnot F, et al. Neuromeningeal sites of multiple myeloma: 3 cases and review of the literature. Rev Med Interne. 1997; 18:646–651.
6. De Blay V, Misson N, Dardenne G, Dupuis MJ. Leptomeningeal myelomatosis mimicking a subdural haematoma. Neuroradiology. 2000; 42:735–737.
7. Roddie P, Collie D, Johnson P. Myelomatous involvement of the dura mater: a rare complication of multiple myeloma. J Clin Pathol. 2000; 53:398–399.
8. Moran CC, Anderson CC, Caldemeyer KS, Smith RR. Meningeal myelomatosis: CT and MR appearances. AJNR Am J Neuroradiol. 1995; 16:1501–1503.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download