Abstract
Gastric teratoma is an extremely rare tumor that accounts for less than 1% of all teratomas. Gastric teratoma is mostly presented as a palpable abdominal mass, and is rarely accompanied with gastrointestinal bleeding such as melena or hematemesis. A 5-month-old male infant was brought with a history of pale facial color and dark-colored stool. The hemoglobin level was at 6.1 g/dL, with melena having begun 1 month previous. Upper gastrointestinal endoscopy revealed a polypoid mass with bleeding at the upper body and lesser curvature of the stomach. Wedge resection of the stomach was performed and histopathological analysis confirmed the mass to be a mature cystic teratoma. There was no recurrence after the operation during follow-up.
Teratomas arise from totipotent cells and contain elements from the all three germ cell layers: ectoderm, endoderm, and mesoderm [1]. Teratomas can occur at any body part but the stomach is not a common place for teratomas to occur. Indeed, gastric teratoma is a very rare disease and comprises less than 1% of all teratomas [12]. The main presentation of gastric teratoma is a palpable abdominal mass, and gastrointestinal bleeding without a palpable mass is not common [1]. We present a case of gastric teratoma that caused gastrointestinal bleeding and was successfully managed by operation.
A 5-month-old male infant has presented with pale facial color and dark-colored stool some days previously. He was born weighing 4,120 g at the 37th gestational week and no significant event occurred during the gestational period. His parents denied any previous medical problem and he was appeared well-developed and well-nourished, weighing 11.6 kg. On physical examination, the abdomen was soft and flat, and there was no palpable mass or tender point.
Further evaluation of the dark-colored stool revealed a melena that had begun 1 month previous. Laboratory tests indicated severe anemia. Serum hemoglobin level was 6.1 g/dL, serum iron level was decreased at 14 µg/dL (normal, 33-193 µg/dL), serum total iron binding capacity level was elevated at 509 µg/dL (normal, 252-456 µg/dL), and serum ferritin level was 5 µg/dL. Other laboratory findings were unremarkable.
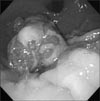
An ultrasonographic scan showed no remarkable abnormal findings. Upper gastrointestinal endoscopy revealed a 3 cm-sized polypoid mass with bleeding at the lesser curvature of the upper gastric body (Fig. 1). At first, we planned to carry out an endoscopic polypectomy, but the polyp had such a large base that the polypectomy could not be performed. Therefore we chose to carry out an open laparotomy instead.
On exploratory laparotomy, a 4.5×3.5 cm sized exophytic and endophytic mass was found at the lesser curvature of the upper gastric body. A small bowel diverticulum was also found at the distal ileum and the diverticulum showed no signs of complication. Wedge resection of the stomach and diverticulectomy were performed. Histopathologically the gastric polypoid mass was confirmed to be a mature cystic teratoma (Fig. 2, 3). He was discharged at 7 days after operation without obvious complication. There was no sign of recurrence during follow-up.
Teratomas can occur everywhere in the body. The most common site of occurrence for teratomas in infancy and childhood is the sacrococcygeal region (60%-65%). Following this are the gonadal region (10%-20%), mediastinal region (5%-10%), presacral region (5%), and intracranial, retroperitoneal, cervical regions (<5%) [3]. Gastrointestinal teratomas are an extremely rare disease and gastric teratomas comprise less than 1% of all teratomas [12]. In spite of the rarity of gastric teratomas, they are the most common teratomas of the gastrointestinal tract [4].
After the first report of gastric teratoma by Eusterman and Sentry [5], approximately 140 cases of gastric teratoma have been reported in English literature. More than 90% of gastric teratomas occur in infants and neonates, showing significant male predominance, with only about 10 cases having been reported in female patients. Adult cases have also been reported [6] and tumor occurrence is possible at any age [127].
Gastric teratomas most commonly present as an exogastric mass, making up 65% of reported cases. The rest are made up of masses that are both endogastric (9%) and exogastric (26%) [3]. Most tumors were reported to be located at posterior wall of the stomach or along the greater curvature [27]. Pathologic results of most reported cases are mature, but immature and malignant gastric teratomas also have been reported [267].
The most common presented symptom is abdominal distension with or without palpable mass. Intestinal obstruction [12], jaundice [8], and respiratory distress [9] due to mass effect are other reported presentations. As in the patient from the current study, gastrointestinal bleeding also can be presented [12]. Bleeding may come from mucosa ulceration over the intra-gastric part of the gastric teratoma [1].
In the present case, we didn't find any clues from ultrasonography. However, generally ultrasonography, CT, and MRI are known as useful tools for diagnosis [6]. Furthermore, the presence of calcification or bony structures in gastric tumors confirmed by plain abdominal X-ray or other diagnostic tools suggest a gastric teratoma [16]. Endoscopy can also be helpful for patients who have relatively small tumors like the boy in our case. Endoscopic findings such as hair or bony structures on the tumor suggests a diagnosis of teratoma [6].
The treatment of choice for gastric teratoma is total excision and primary repair of the gastric wall. Because most gastric teratomas are mature and benign, they show good prognosis after surgical excision [6]. The need for adjuvant therapy such as chemotherapy or radiation therapy after complete excision of immature and malignant gastric teratomas is still not clearly understood due to their rarity. Nonetheless, up until now, complete excision without adjuvant therapy has shown good prognosis [710].
Most patients from the reported cases of gastric teratoma have shown good prognosis without recurrence, but there is one report of a tumor recurring 20 years after complete rescection, as such regular follow-up is required [6]. As with other teratomas, gastric teratomas can also lead to an elevated level of serum α-FP. Thus, monitoring of the serum α-FP level at follow-up is recommended in order to detect any recurrence or presence of a residual tumor [147]. In this case, because we did not expect the gastric teratoma as a diagnosis, serum α-FP and human chorionic gonadotropin (HCG) levels were not checked preoperatively. Serum α-FP and HCG levels were within normal range after operation.
Figures and Tables
Fig. 2
Gross finding shows 4.2×3.4×3.0 cm sized multi-lobulated mass, with both exo- and endophytic growth.

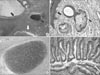
Fig. 3
Microscopic findings. (A) All 3 germ layer tissues; black arrow, squamous epithelium lined cystic lesion from ectoderm; black arrowhead, cartilage from mesoderm; white arrow, small intestinal epithelium from endoderm (H&E, ×40). (B) Ectoderm origin tissues; black arrow, squamous epithelium; black arrowhead, sebaceous gland (H&E, ×100). (C) Mesoderm origin tissue; cartilage (H&E, ×100). (D) Endoderm origin tissue; gastrointestinal epithelium (H&E, ×100).
ACKNOWLEDGMENTS
This work was supported by clinical research grant in 2014 from Pusan National University Hospital.
References
1. Wakhlu A, Wakhlu AK. Paediatric gastric teratoma. Eur J Pediatr Surg. 2002; 12:375–378.
2. Anilkumar MG, Jagadishkumar K, Girish GN, Sunila . Immature gastric teratoma in an infant. Indian J Surg. 2013; 75:Suppl 1. 453–455.
3. Yoon SE, Goo HW, Jun S, Lee IC, Yoon CH. Immature gastric teratoma in an infant: a case report. Korean J Radiol. 2000; 1:226–228.
4. Yaji PR, Joshi S, Kinhal V, Ravishankar TH, Jayaprakasha G, Melapure A, et al. Gastric teratoma in an infant: a rare case report and discussion. Indian J Surg. 2013; 75:Suppl 1. 152–154.
5. Eusterman GB, Sentry EG. Benign tumours of the stomach: report of 27 cases. Surg Gynecol Obstet. 1922; 34:372–378.
6. Gupta V, Babu RY, Rana S, Vaiphei K, Rao KL, Bhasin DK. Mature gastric teratoma: recurrence in adulthood. J Pediatr Surg. 2009; 44:e17–e19.
7. Saha M. Malignant gastric teratoma: report of two cases from a single center. Pediatr Surg Int. 2010; 26:931–934.
8. Kumar V, Godara R, Bharadwaj R, Arora M. Gastric teratoma-unusual cause of neonatal obstructive jaundice: a case report. Indian J Surg. 2013; 75:Suppl 1. 421–424.
9. Jeong HC, Cha SJ, Kim GJ. Rapidly grown congenital fetal immature gastric teratoma causing severe neonatal respiratory distress. J Obstet Gynaecol Res. 2012; 38:449–451.
10. Gupta DK, Srinivas M, Dave S, Agarwala S, Bajpai M, Mitra DK. Gastric teratoma in children. Pediatr Surg Int. 2000; 16:329–332.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download