This article has been
cited by other articles in ScienceCentral.
Abstract
Brown-Séquard syndrome (BSS) is an incomplete spinal cord injury caused by damage to one-half of the spinal cord. Most cases of BSS result from penetrating trauma or tumors, and acute cervical disc herniation is a relatively rare cause of BSS. In this case, a 34-year-old man with a sudden onset posterior neck pain and left side motor weakness was admitted to the local spine hospital. Pain and temperature sensation of pain was decreased below the right C4 dermatome. The left arm and leg motor grade was 0. Magnetic resonance imaging (MRI) showed a huge trans-ligamentous herniated disc rupture from the center to the left at the level of C3–4, and anterior cervical discectomy and fusion were performed. After emergency surgery, left arm and leg motor grade recovered to 2, and normal voiding function returned. MRI verified complete removal of the cervical herniated disc. This case describes the approach to rapid diagnosis in a patient with characteristic clinical symptoms of BSS and radiological findings of a herniated cervical disc. Rapid and accurate diagnosis and immediate decompressive surgery increased the possibility of a good surgical outcome, even if the neurologic deficits are grave at the time of admission.
Keywords: Brown-Sequard syndrome, Herniated disc, Anterior cervical discectomy and fusion
INTRODUCTION
Brown-Séquard syndrome (BSS) is characterized by a hemisection injury of the spinal cord and shows clinical features such as paralysis on the damaged ipsilateral side, decreased proprioception, and decreased pain and temperature sensation on the contralateral side. Causes of BSS include traumatic injury, tumor, ischemia, and hemorrhage. Relatively, cervical disc herniation (CDH) is a rare cause of BSS. This case report describes the progress after surgical treatment of the BSS patient induced by CDH and like to suggest the cases that other spine surgeon can refer to when a similar patient is encountered in the clinic.
CASE REPORT
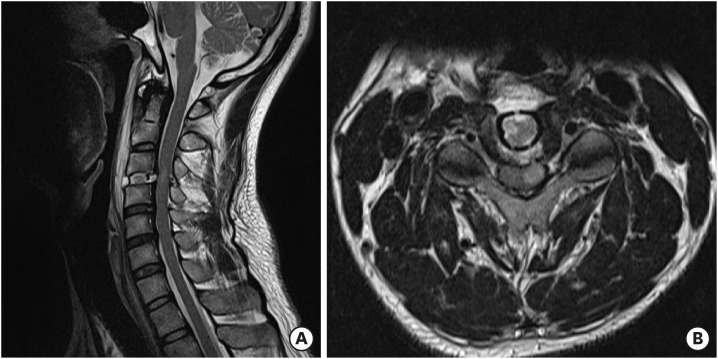
A 34-year-old man with a sudden onset posterior neck pain and left side motor weakness was admitted to the local spine hospital. The patient had no previous medical history or disease. The patient developed the symptoms after getting his head hit against an abruptly closing door. On physical examination at the time of admission, motor power of the left upper and lower extremities was 0. Proprioceptive sensation was decreased below the left C4 dermatome, with associated numbness. Pain and temperature sensation was decreased below the right C4 dermatome. Urinary sensation and anal tone were intact at the time of admission but suddenly decreased 1 hour after admission. Magnetic resonance imaging (MRI) showed an acutely ruptured, large transligamentous herniated disc from the center to the left at the C3–4 level, and findings of a cervical cord contusion (
FIGURE 1). Emergency C3–4 anterior cervical discectomy and fusion (ACDF) was performed because a definite traumatic event caused symptoms within a short time. Postoperative MRI revealed that all C3–4 disc fragments were completely removed (
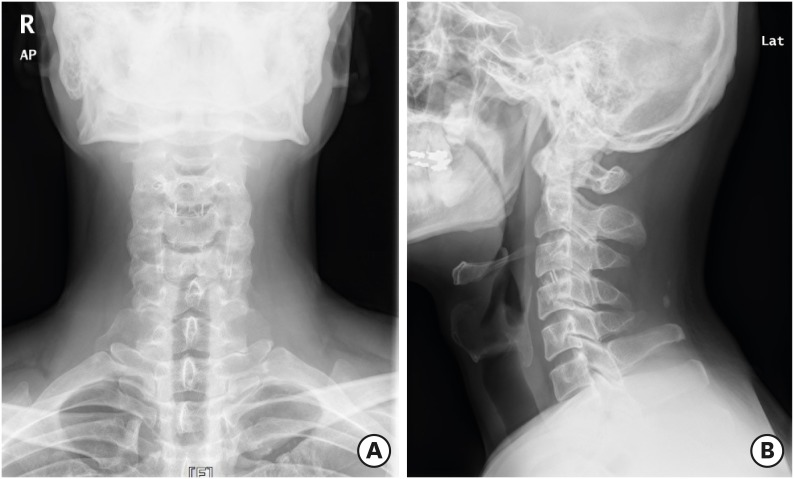
FIGURE 2). Left side motor activity began to recover 1 day after surgery and left upper and lower extremity motor grade recovered to 2+ and 3+ after 4 days. The patient could sense urinary retention at 4 days after surgery, and urinary function completely recovered by 11 days after surgery. The patient was able to ambulate with a walker at 16 days after surgery. Pain decreased after surgery, but impaired temperature sensation and numbness were still present at discharge. The patient was discharged 23 days after surgery and received comprehensive rehabilitation therapy. At 6 months after surgery, cervical-spine X-ray images (
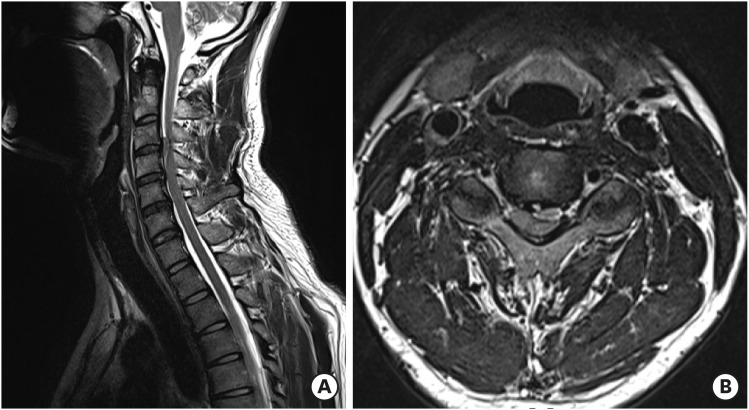
FIGURE 3) and MRI (
FIGURE 4) confirmed that the inserted cage was well maintained, and the fusion status was good. Signal changes present on postoperative MRI were decreased at 6-month follow-up (
FIGURE 4). Motor grade improved to 4+ at 5 months after surgery. Sensory changes below the C4 dermatome showed improvement, but persisted during the follow-up period.
FIGURE 1
Preoperative cervical MRI. Sagittal (A) MRI shows a herniated disc at the C3–4 level. Axial (B) MRI shows a huge transligamentous disc rupture from the center to the left at the C3–4 level. Findings indicating contusion were also observed.
MRI: magnetic resonance imaging.
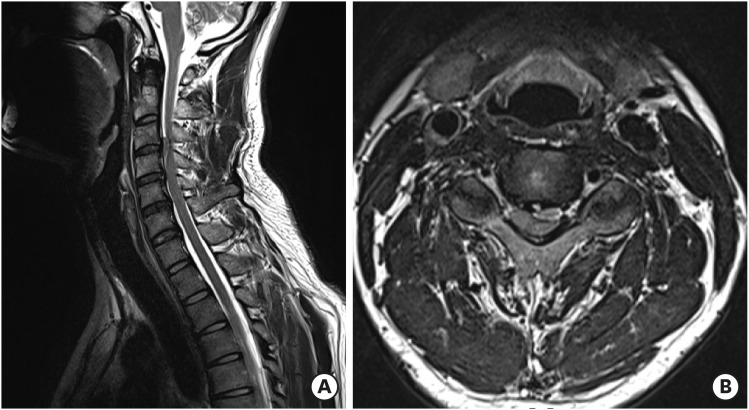
FIGURE 2
Postoperative cervical MRI. Sagittal (A) and axial (B) MRI shows a properly inserted cage and complete removal of the disc at C3–4. Signal changes persist in the left spinal cord.
MRI: magnetic resonance imaging.
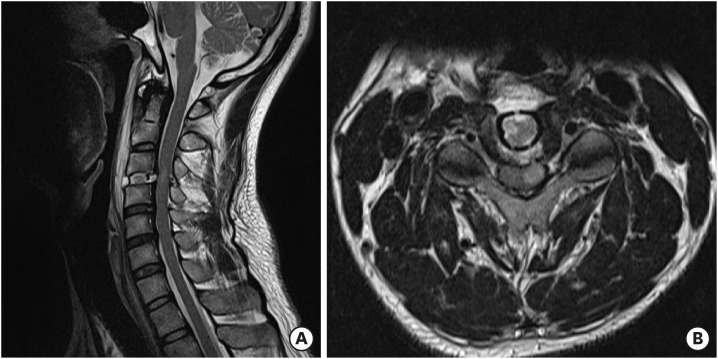
FIGURE 3
Cervical X-ray images 6 months after surgery. Cervical anteroposterior (A) and lateral (B) X-ray images show a well-maintained cage at the C3–4 level.
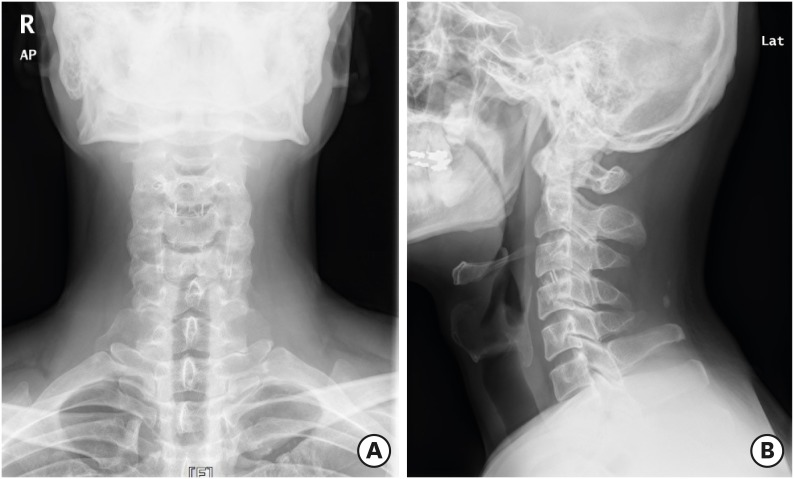
FIGURE 4
Cervical MRI 6 months after surgery. Sagittal (A) and axial (B) MRI shows fusion of C3–4 and decreased signal change in the spinal cord at C3–4.
MRI: magnetic resonance imaging.

DISCUSSION
BSS is an uncommon spinal cord disorder.
4) About 11,000 spinal cord injuries occur each year in the USA, but only about 500 BSS cases have been reported to date.
5,7) The most common causes of BSS are traumatic injury and spinal cord tumor.
1,10,12) CDH is a relatively rare cause of BSS
3,6) and only few reports of BSS caused by CDH have been published until now.
9)
Among cases of CDH causing BSS, most occur due to degenerative change and sudden CDH rupture after acute trauma is also very rare. As the prevalence of BSS is not high and the causes vary, there is no standard treatment protocol. However, several case reports have shown better outcomes with surgery than with conservative treatment. Choi et al.
2) and Kohno et al.
4) reported the results of ACDF in 10 patients with BSS, most of whom recovered motor function, as in the present case. One patient showed symptom improvement despite onset 15 months prior. BSS reportedly has the best prognosis among causes of incomplete spinal cord injury.
8,11) Roth et al.
11) reported that when upper extremity motor impairment was greater than lower extremity impairment, most patients were discharged from the hospital with the ability to walk.
In the present case, the patient was transferred to the hospital when he had characteristic clinical features of BSS. Based on MRI findings and acute trauma caused by a vertical compressive force to the head and neck, a diagnosis of BSS due to acute traumatic CDH was made. A good outcome was obtained with emergency surgery following rapid diagnosis. As a result, the motor grade on long-term follow-up improved from G0 to G4+.
When a patient with acute BSS due to CDH is encountered clinically, good surgical results can be expected when appropriate surgical treatment is performed promptly, even if the neurological deficits are grave at the time of admission.
CONCLUSION
BSS is rarely caused by an acutely herniated cervical disc. This case describes the approach to rapid diagnosis in a patient with characteristic clinical symptoms of BSS and radiological findings of a herniated cervical disc. Rapid and accurate diagnosis and immediate decompressive surgery increased the possibility of a good surgical outcome, even if the neurologic deficits are grave at the time of admission.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download