This article has been
cited by other articles in ScienceCentral.
Abstract
Objective
Forehead deformities are often caused by lack of treatment or incorrect restoration of the frontal buttress, so the underlying frontal buttress should be restored to its previous position to ensure that the previous forehead contour is restored in cases of complex depressed skull fractures. However, since brain injuries from skull fractures could have fatal consequences, the clinical concern in primary surgery has been to save the patient's life, and cosmetic concerns have always been secondary. We retrospectively reviewed fronto-orbital fracture patients who underwent primary restoration with primary bone fragments or an alloplastic implant and compared the surgical outcomes of autologous bone (group 1) and artificial materials (group 2).
Methods
A retrospective review was conducted of 47 patients with fronto-orbital fractures between March 2012 and January 2018. The patients underwent primary reconstruction with primary bone fragments or an alloplastic implant. The surgical results were evaluated by the incidence of infection and cosmetic satisfaction of patients.
Results
Infections occurred in one patient (5%) in group 1 and in two patients (15.3%) in group 2, which was not a statistically significant difference. In contrast, at 6 months after surgery, patient satisfaction showed a statistically significant between-group difference (group 1: 4.32 points, group 2: 3.54 points, p=0.001).
Conclusion
Primary reconstruction using fractured bone fragments is an effective and preferable method that could result in better surgical outcomes than restoration using an alloplastic implant.
Keywords: Frontal sinus, Skull fractures, Fracture treatment
INTRODUCTION
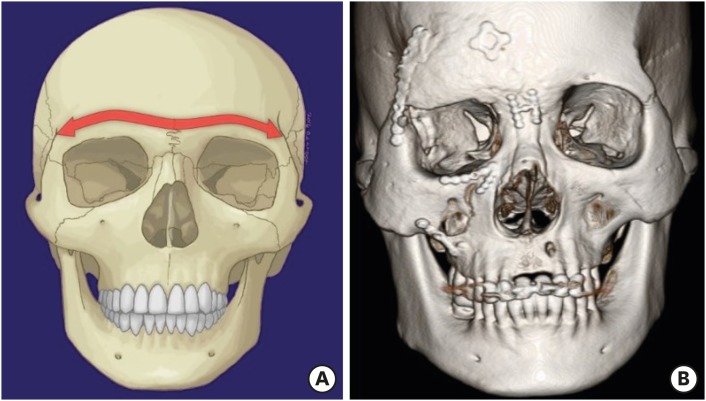
Forehead deformities caused by depressed skull fractures cause aesthetic problems and restoring an aesthetically acceptable forehead appearance significantly depends on the precise restoration of the fronto-orbital buttress. The transverse frontal buttress is a complex structure formed by the frontal bone, frontal sinus, and supraorbital rim that determines the upper facial width and projection of the forehead (
FIGURE 1).
58) As the horizontal frontal buttress, which forms the boundary between the mid-facial bone and the upper facial bone, is located at the bottom of the cranium, skull fractures are often accompanied by fronto-orbital buttress fractures. Forehead deformities are often caused by lack of treatment or incorrect restoration of the frontal buttress, so the underlying frontal buttress should be restored to its previous position to ensure that the previous forehead contour is restored in cases of complex depressed skull fractures (
FIGURE 2 &
3). However, since brain injuries from skull fractures could have fatal consequences, the clinical concern in primary surgery has been to save the patient's life, and cosmetic concerns have always been secondary.
1)
FIGURE 1
(A) The transverse frontal buttress is a complex structure formed by the frontal bone, frontal sinus, and supraorbital rim that determines the upper facial width and projection of the forehead. (B) Forehead deformities are often caused by lack of treatment or incorrect restoration of the frontal buttress.
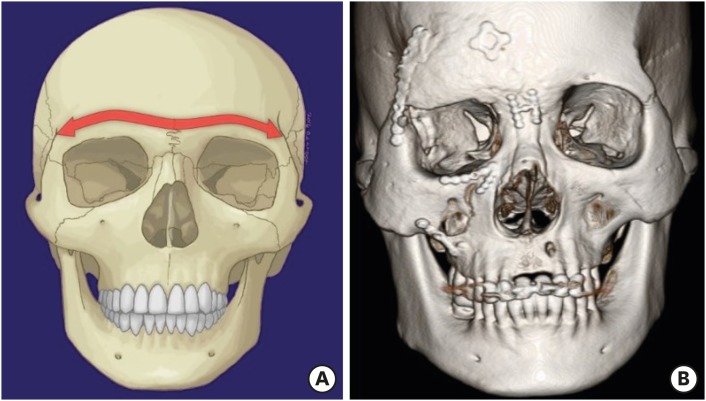
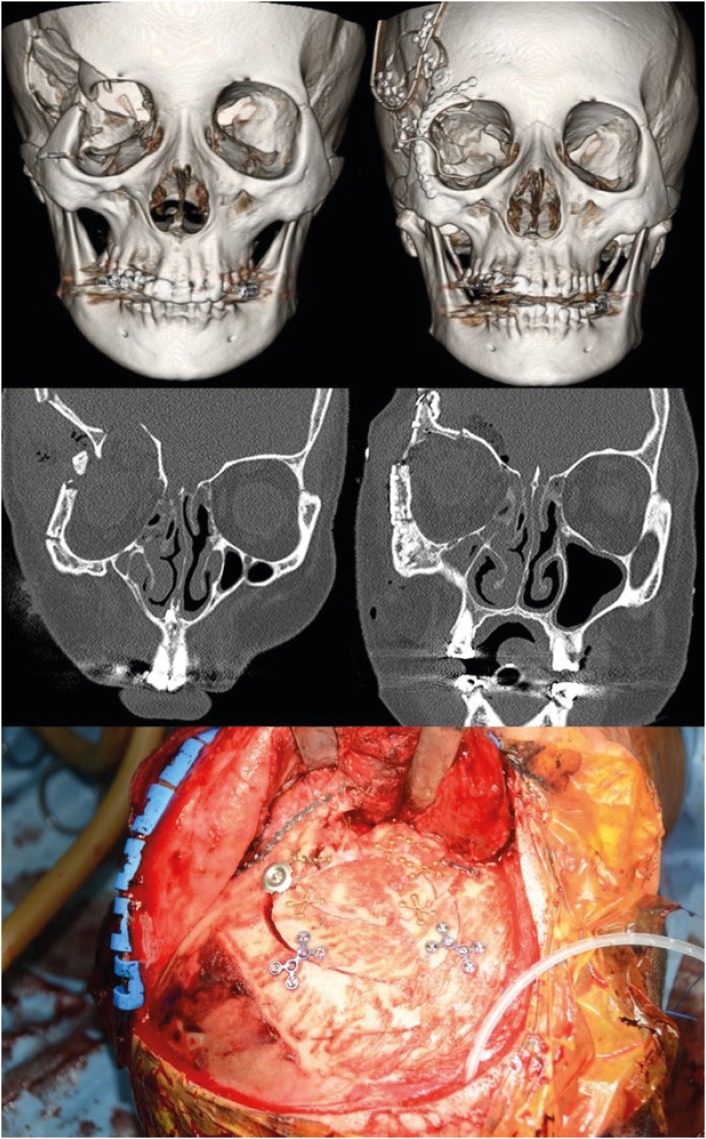
FIGURE 2
A 59-year-old woman with a compound comminuted depressed fronto-orbital fracture, underwent fronto-orbital reconstruction with primary bone fragments. Preoperative and postoperative three-dimensional computed tomography images.
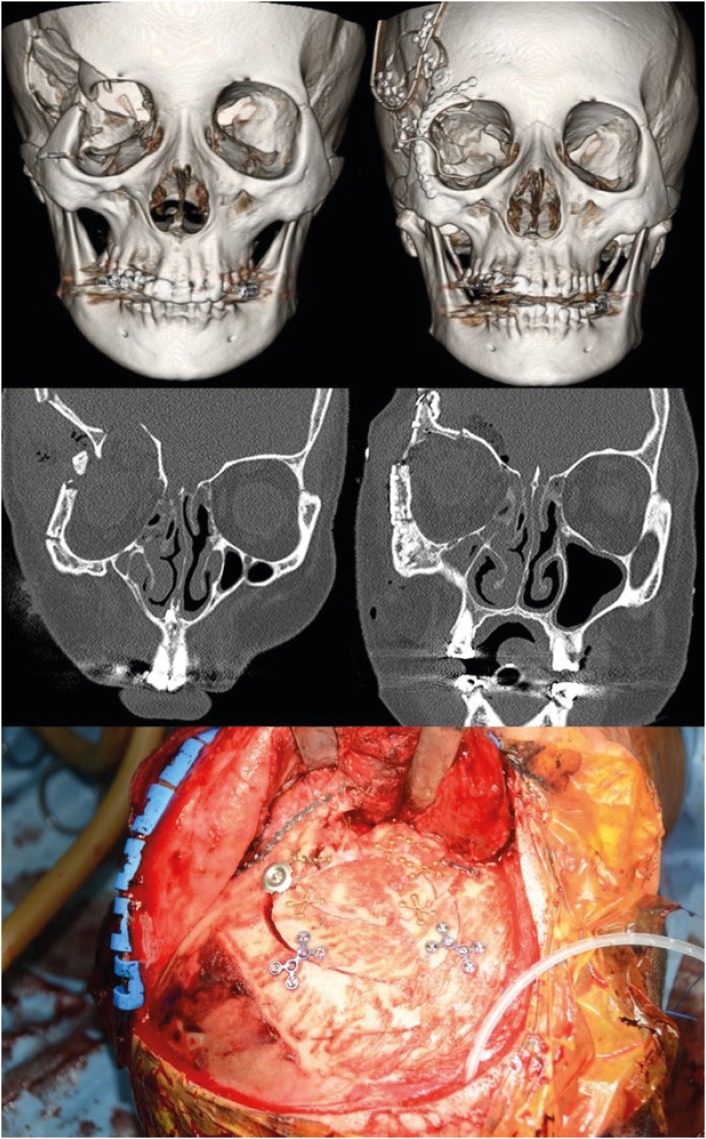
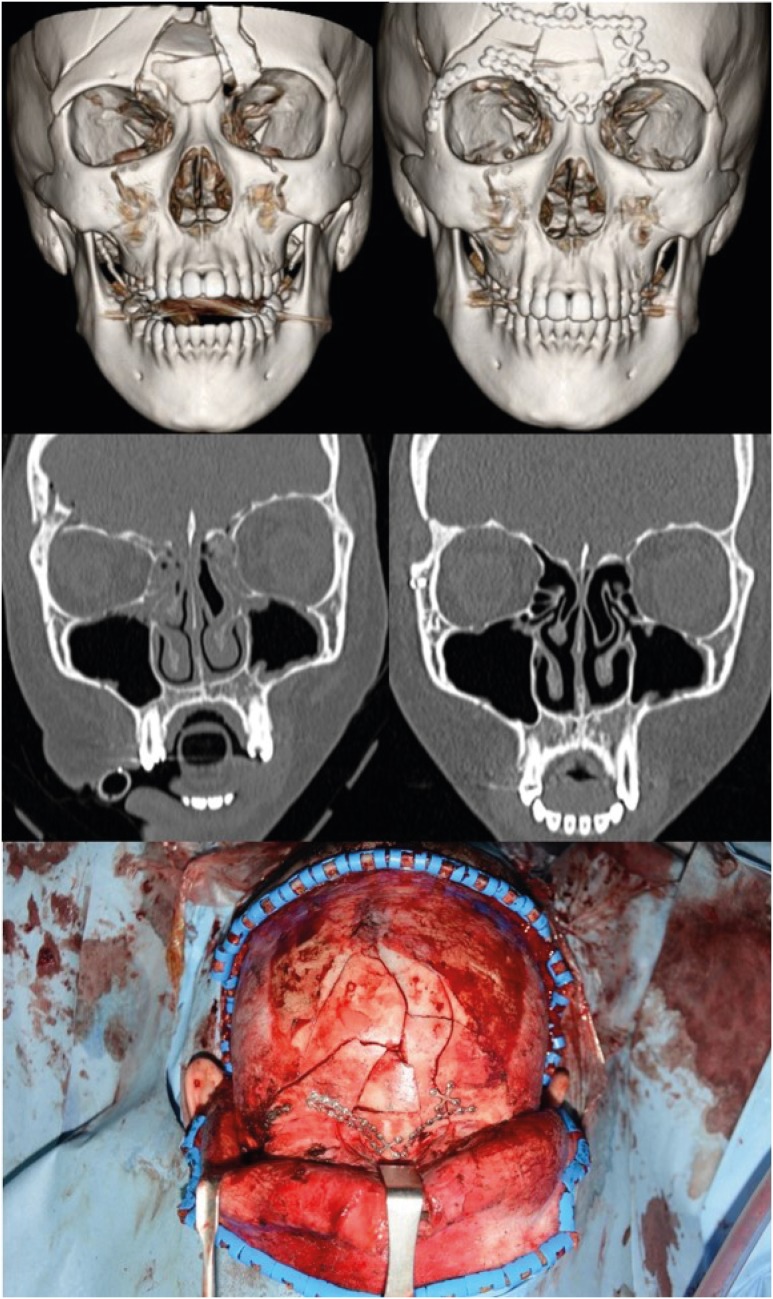
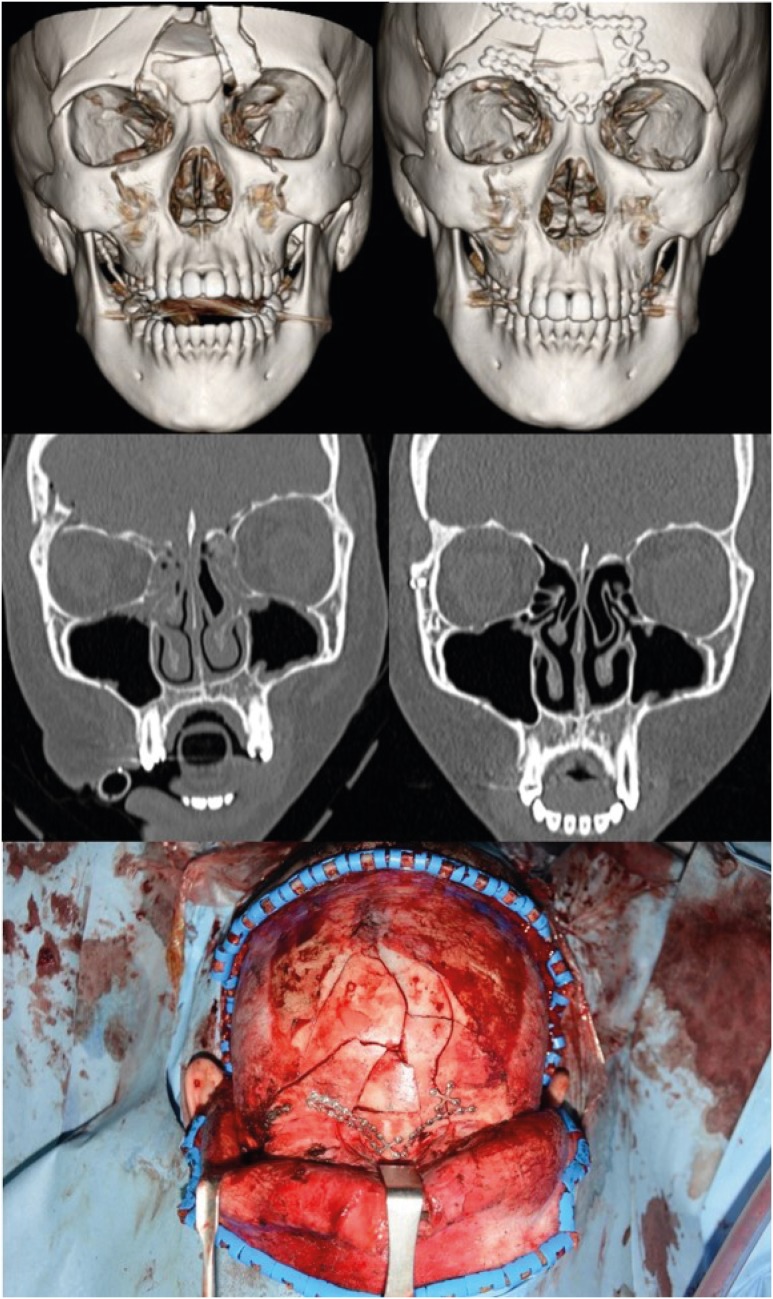
FIGURE 3
A 19-year-old woman with a compound comminuted depressed fronto-orbital fracture, underwent fronto-orbital restoration with primary bone fragments. Preoperative and postoperative three-dimensional computed tomography images.
Forehead deformities caused by improper restoration of the frontal buttress in primary surgery are very difficult to reconstruct in delayed surgery. In particular, severe forehead deformities remain when a depressed skull fracture is reconstructed with alloplastic implants without treating the frontal buttress in primary surgery, and those deformities are very difficult to correct in subsequent surgery; therefore, they remain a challenge for craniofacial surgeons.
1)
Skull fractures can be treated with autogenous bone or artificial materials in primary surgery, but the use of reconstructive materials is controversial because complications such as infection or exposure of implants that encircle the brain could affect the patient's long-term results. Extensive debridement including contaminated bone fragments and secondary reconstruction using an alloplastic implant have been performed for a long time, but implants are susceptible to infection and the degree to which the complexity of the frontal buttress can be reconstructed is limited.
12347910) Modern advanced antibiotics have increased the ability to control infection after surgery, and surgeons have therefore attempted primary reconstruction with primary bone fragments in complex skull fractures.
6) Several reports have shown that primary restorations with bone fragments did not differ in terms of the infection rate compared to delayed reconstructions.
12347910)
In this study, we conducted a retrospective review of fronto-orbital fracture patients who underwent primary restoration with primary bone fragments or an alloplastic implant and compared the outcomes of autologous bone to that of artificial materials.
MATERIALS AND METHODS
All 125 patients who were diagnosed with a fronto-orbital fracture between March 2012 and January 2018 were enrolled. The diagnosis was made using three-dimensional facial bone computed tomography (Brilliance iCT; Philips Medical Systems, Eindhoven, The Netherlands). Seventy-eight cases were excluded, and a total of 47 cases were ultimately included in this study. The exclusion criteria were as follows: 1) difficulties in primary reconstruction of the frontal buttress due to unstable vital signs with severe cerebral edema or elevated intracranial pressure; 2) the need for a decompressive craniectomy procedure due to accompanying hematoma; 3) extensive debridement of the external wound and additional secondary reconstructive surgery.
All operations were performed collaboratively by a plastic surgeon and a neurosurgeon. The frontal buttress and accompanying facial bone fracture were operated on by the plastic surgeon, while the posterior table of the frontal bone and calvarium were operated on by the neurosurgeon. When an extensive bony defect of the frontal buttress was present, reconstruction was conducted using a polymethyl methacrylate (DePuy CMW™; DePuy International Ltd., Blackpool, United Kingdom).
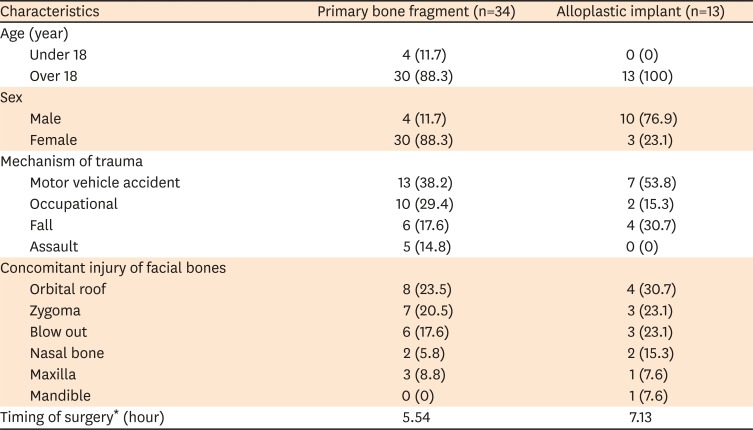
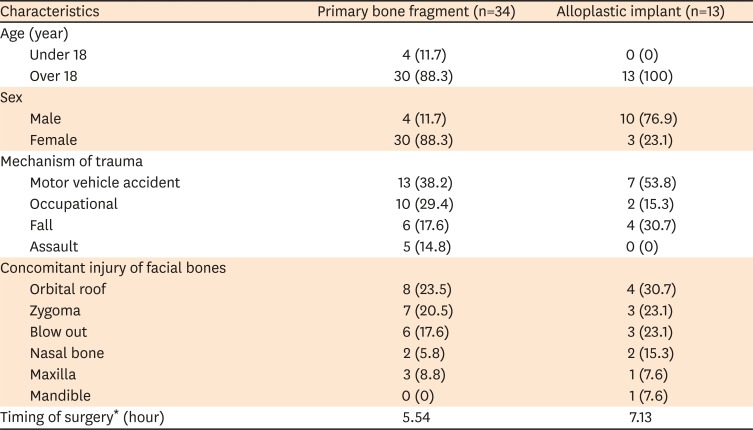
We classified the patients into two groups depending on whether autologous (group 1, n=34) or artificial (group 2, n=13) materials were used for primary reconstruction of the frontal buttress. The demographic information of the patients is shown in
TABLE 1. We also compared the infection rate and patients' aesthetic satisfaction between the groups. To analyze patients' satisfaction, a 5-point Likert scale (1: not at all satisfied, 5: completely satisfied) was administered to all patients at 6 months after surgery. Additionally, postoperative computed tomography was obtained in all patients 1 year postoperatively in the outpatient clinic.
TABLE 1
Demographic information of the patients (n=47)
|
Characteristics |
Primary bone fragment (n=34) |
Alloplastic implant (n=13) |
|
Age (year) |
|
|
|
Under 18 |
4 (11.7) |
0 (0) |
|
Over 18 |
30 (88.3) |
13 (100) |
|
Sex |
|
|
|
Male |
4 (11.7) |
10 (76.9) |
|
Female |
30 (88.3) |
3 (23.1) |
|
Mechanism of trauma |
|
|
|
Motor vehicle accident |
13 (38.2) |
7 (53.8) |
|
Occupational |
10 (29.4) |
2 (15.3) |
|
Fall |
6 (17.6) |
4 (30.7) |
|
Assault |
5 (14.8) |
0 (0) |
|
Concomitant injury of facial bones |
|
|
|
Orbital roof |
8 (23.5) |
4 (30.7) |
|
Zygoma |
7 (20.5) |
3 (23.1) |
|
Blow out |
6 (17.6) |
3 (23.1) |
|
Nasal bone |
2 (5.8) |
2 (15.3) |
|
Maxilla |
3 (8.8) |
1 (7.6) |
|
Mandible |
0 (0) |
1 (7.6) |
|
Timing of surgery* (hour) |
5.54 |
7.13 |
A statistical analysis was conducted to evaluate differences between the two groups. The Fisher exact test was used to compare the rate of infectious complications, and the independent t-test was used to compare patients' aesthetic satisfaction level and the timing of surgery. The p-values less than 0.05 were considered to indicate statistical significance. All analyses were performed using SPSS version 20.0 (IBM Corp., Armonk, NY, USA).
RESULTS
The patients ranged in age from 9 to 84 years (mean, 40.8 years; four patients were under 18 years old), and 40 (85.1%) were men and 7 (17.9%) were women. The most common cause of injury was motor vehicle accidents (20 cases), followed by occupational injuries (12 cases), falls (10 cases), and assault (5 cases). Of the 47 patients, 20 had concomitant facial bone fractures, in the following order of frequency: orbital roof (12 cases), zygoma (10 cases), blowout (9 cases), maxilla (4 cases), nasal bone (4 cases), and mandible (1 case) (
TABLE 1). Age, sex, mechanism of trauma, and the presence of a concomitant fracture did not show significant differences between groups. In addition, all operations were performed as emergency surgery, and the time from injury to operation did not show statistically significant differences between the two groups (group 1: 5.54 hours, group 2: 7.13 hours;
p=0.279) (
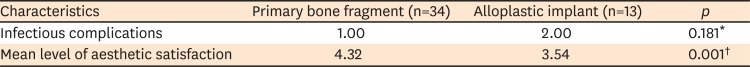
TABLE 1). Infections occurred in one patient (5%) in group 1 and in two patients (15.3%) in group 2, which was not a statistically significant difference (
TABLE 2). In contrast, at 6 months after surgery, patient satisfaction showed statistically significant differences between the two groups (group 1: 4.32 points, group 2: 3.54 points,
p=0.001) (
TABLE 2).
TABLE 2
Statistical analysis of the two groups
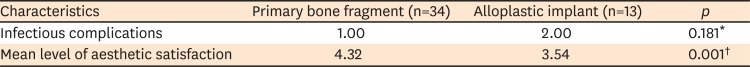
|
Characteristics |
Primary bone fragment (n=34) |
Alloplastic implant (n=13) |
p
|
|
Infectious complications |
1.00 |
2.00 |
0.181*
|
|
Mean level of aesthetic satisfaction |
4.32 |
3.54 |
0.001†
|
DISCUSSION
The midface buttress system is the bony supporting structure that provides stability to the facial skeleton, and reconstructing these buttresses is the primary surgical goal in procedures conducted to maintain the facial shape in patients with a facial bone fracture. Within this buttress system, the transverse frontal buttress is a complex structure consisting of the frontal bone, frontal sinus, supraorbital rim, and orbital roof that determines forehead width and projection. It plays an important role in the aesthetic aspect of the forehead and requires sophisticated restoration in cases of complex depressed skull fractures. However, brain injuries in patients with skull fractures can have fatal consequences, so the clinical concern in primary surgery has been to save the patient's life, and cosmetic concerns have always been secondary.
1) However, it is very difficult to restore forehead deformities caused by incorrect restoration of the frontal buttress in a primary operation to the delicate pre-traumatic forehead contour in delayed surgery. In particular, a severe forehead deformity remains when a depressed skull fracture is reconstructed with an alloplastic implant without treating the frontal buttress in primary surgery.
4) Therefore, the underlying transverse frontal buttress should be restored to its prior position in primary surgery to preserve the previous forehead contour.
If the fracture is severely comminuted, reconstruction of the fronto-orbital buttress using autologous bone is challenging. In such cases, alloplastic implants have been used to replace the bony defect. The traditional surgical method involved extensive debridement including contaminated bony fragments to reduce the risk of infection, and secondary reconstruction was carried out later.
12347910) However, in the late 1960s, a method of restoration using primary bone fragments began to be implemented, and several studies showed that the postoperative infection rates were not higher than after conventional surgery. Kriss et al.
7) reported that the rate of infection in 79 patients who underwent immediate reconstruction with primary bone fragments was 2.5%. Braakman
3) reviewed 185 patients who received immediate replacement of bone fragments and the infection rate was 4.6%. Nadell and Kline
9) documented 85 patients who received primary bone fragment replacement, and reported an infection rate of 9.2% after surgery. Blankenship et al.
2) reported 31 pediatric patients who underwent bone fragment replacement. None of the patients in their study developed a postoperative infection. All of the above studies were performed on patients who underwent surgery within 24 hours of the injury. The timing of surgery is a major risk factor for postoperative infection. Most authors claim that surgery should be performed within 24 hours because the rate of infection increases significantly over time.
37)
The current surgical options for secondary reconstruction of forehead deformities range from bone rearrangement followed by osteotomy to less complicated methods of onlay grafting with autogenous bone or alloplastic material. Recently, computer-aided design and computer-aided prefabricated implants have been claimed to have the advantage of enabling a precise fit to the complex shape of the frontal buttress during craniofacial reconstruction, but the utility of these techniques in emergency surgery is limited.
Reconstruction using autogenous bone has other advantages in pediatric patients. In this study, there were four children under the age of 18 years. Reconstruction with an alloplastic implant in pediatric patients may cause re-fractures due to the greater bony gap between artificial bone and autogenous bone or loosening of fixation as bone grows.
7) Therefore, reconstruction with primary bone fragments is recommended for fractures in children.
The patients who were enrolled in this study underwent surgery within 24 hours after trauma, and the postoperative infection rate, timing of surgery, and postoperative aesthetic satisfaction were compared between both groups. There was no statistically significant difference in the timing of surgery between the two groups. Postoperative infections occurred in one patient in group 1 (treated using primary bone fragments) and in two patients in group 2 (treated using alloplastic materials), but the difference was not statistically significant. This suggests that restoration with primary bone fragments does not increase the risk of infection and that further studies will be needed with more cases. The mean follow-up period was 13.2 months and the aesthetic satisfaction of the patients was evaluated at a 6-month postoperative follow-up visit when the overlying soft tissue swelling had resolved. In the patient satisfaction survey, we used a 5-point Likert scale (1: completely dissatisfied, 5: completely satisfied). Patient who were not satisfied complained of forehead deformation and scarring of the forehead. Group 1 (treated with primary bone fragments) showed a significantly higher level of aesthetic satisfaction than group 2 (treated with alloplastic materials). Although there was no significant difference in the rate of infection, restoration using primary bone fragments led to higher aesthetic satisfaction than restoration using alloplastic implants. Therefore, the use of primary bone fragments is considered to be a better method for reconstructing the complex structure of the frontal buttress, as well as a more promising way to avoid secondary surgery due to the possibility of implant infection over long-term observation.
CONCLUSION
In conclusion, restoring fronto-orbital fractures with primary bone fragments did not increase the incidence of postoperative infections. Patients treated with primary bone fragments were more satisfied in terms of cosmetic outcomes than those who received surgery using alloplastic implants. Therefore, we propose that immediate restoration using fractured primary bone fragments in patients with fronto-orbital fractures is a desirable method to restore the pretraumatic condition of the forehead.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download