Abstract
Cerebral venous sinus thrombosis (CVST) is a rare disease. Early diagnosis and treatment are important, as CVST is potentially fatal. Pregnancy and puerperium are known risk factors for CVST. Here, we report the case of a patient who developed superior sagittal sinus thrombosis after a normal vaginal delivery. A 20-year-old woman presented with a headache and seizures two days after a normal vaginal delivery. Initially, brain computed tomography (CT) showed a subarachnoid hemorrhage in the right parietal lobe and sylvian fissure, together with mild cerebral edema. CT angiography revealed superior sagittal sinus thrombosis. Multiple micro-infarctions were seen on diffusion-weighted magnetic resonance images. An intravenous infusion of heparin and mannitol was administered immediately. Two days after treatment initiation, the patient showed sudden neurological deterioration, with left-sided hemiplegia. Brain CT showed moderate brain edema and hemorrhagic densities. Emergency decompressive craniectomy was performed, and heparin was re-administered on post-operative day (POD) 1. On POD 9, the patient's mental state improved from stupor to drowsy, but the left-sided hemiplegia persisted. CT angiography showed that the superior sinus thrombosis had decreased. Superior sagittal sinus thrombosis is an uncommon complication, with an unfavorable outcome, after delivery. Timely diagnosis and treatment are important for preventing neurological deterioration.
Cerebral venous sinus thrombosis (CVST) is a rare occurrence during pregnancy and the postpartum period.1) Patients generally have symptoms like seizures, headaches, and other neurologic deficits. These symptoms transpire because of obstruction of cerebral venous sinuses, and decreased drainage of cerebrospinal fluid, leading to intracranial hypertension.2) Early diagnosis and treatment of CVST, which is potentially fatal, are quite important. Pregnancy and puerperium are known CVST risk factors.
Here, we report the case of a young woman who developed CVST two days after normal vaginal delivery.
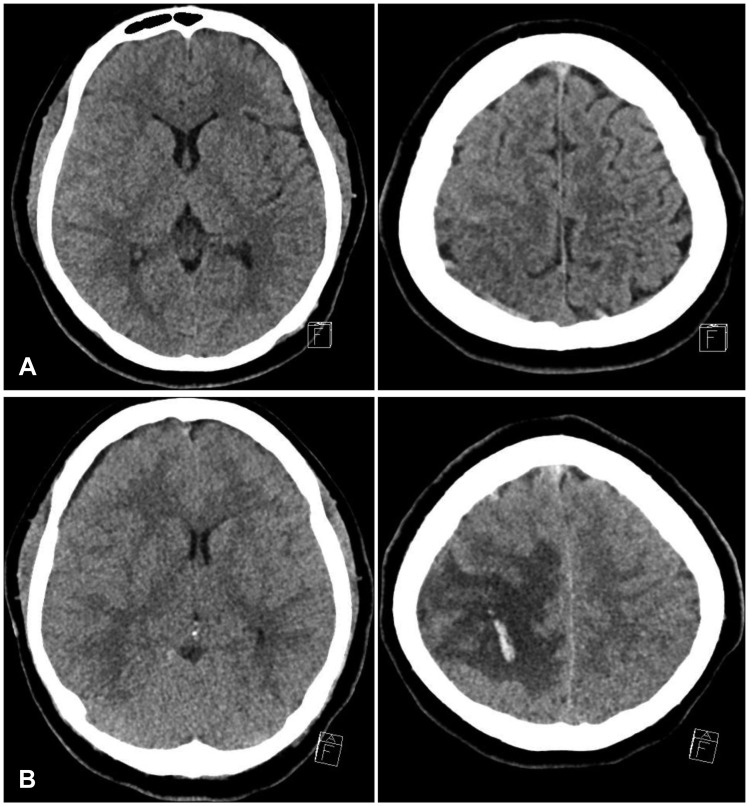
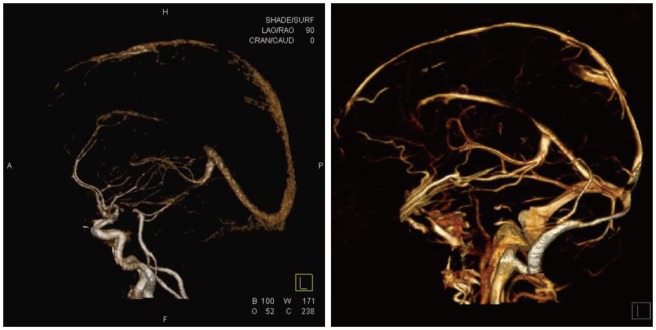
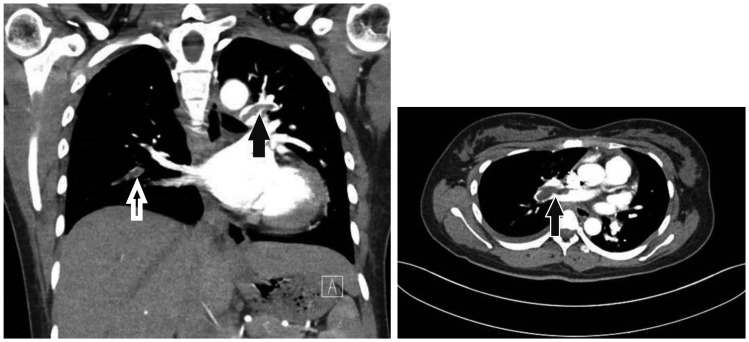
A 20-year-old woman, primigravida, presented with a headache and seizures two days after normal vaginal delivery. She had no past medical history, and no family history of hematological disorder. The seizure was generalised tonic-clonic seizure, and stopped spontaneously after two minutes. She felt an intense headache and had a seizure. After postictal state, her body temperature, heart rate, and blood pressure were 37℃, 88 beats/min, and 130/80 mmHg, respectively. Neurological deficits were not identified. Initially, brain computed tomography (CT) revealed subarachnoid hemorrhage (SAH) in the right parietal lobe and sylvian fissure, and mild cerebral edema (Figure 1A). Considering the patient's age, and absence of a past medical history, brain CT angiography was performed to rule out diseases such as cerebral aneurysm, arteriovenous malformation, or sinus thrombosis. We found a superior sagittal sinus thrombosis. Multiple micro-infarctions were seen on diffusion magnetic resonance (MR) imaging (MRI). Sinus thrombosis was treated with conservative medical treatment, including immediate intravenous administration of heparin and mannitol, as well as blood pressure maintenance. Cerebral digital subtraction angiography was planned to identify definite etiology. Two days after treatment was initiated, patient showed a sudden neurological deterioration, with left side hemiplegia. At the time, she had not been experiencing seizures or a headache. Her consciousness level was E2V3M5 on the Glasgow Coma Scale (GCS). Brain CT showed moderate brain edema, with hemorrhagic densities and midline shift (Figure 1B). Emergency surgical decompression with duroplasty was performed. After the operation, intracranial pressure was controlled using mannitol. To address CVST, systemic heparinization was restarted on post-operative day (POD) 1. On POD 9, the patient's mental state was improved from stupor to drowsy, but left side hemiplegia persisted. Brain CT angiography showed a decrease in size of the superior sinus thrombosis (Figure 2). On POD 28, she developed chest pain. Chest and lower extremity CT angiography was performed to rule out conditions such as deep vein thrombosis and pulmonary thromboembolism. We found a pulmonary thromboembolism at the pulmonary trunk bifurcation (Figure 3). After consultation, we changed the patient's medication to dabigatran (pradaxa). On POD 58, brain swelling reduced, and cranioplasty was performed. Finally, she recovered to E4V5M6 on GCS, and was discharged from hospital.
CVST is rare in developed countries, with an incidence rate ranging from 1:10,000 to 1:25,000.1.8) There are no specific symptoms for CVST. Diagnosis is very difficult owing to the condition's rarity and the obscurity of symptoms. Of help, is to note a patient's background and history. Risk factors easily identifiable from a medical history include, pregnancy, puerperium, connective tissue disease, malignancy, contraceptive use, and infections such as, sinusitis, otitis, and mastoiditis.7) Young individuals, especially young women, are more vulnerable. The International Study on CVST reported that 78% of all cases were aged less than 50 years, and that the incidence of CVST was three times greater in women than men.3) When a young, pregnant, or postpartum woman presents with new onset, stroke-like symptoms, such as headaches and seizure, it is significant to examine for the CVST risk factors. If CVST is suspected, CT venography or MR venography should be performed. However, due to its small size, CVST is hard to detect using these conventional modalities. A recent study proved that T2*/susceptibility-weighted MRI sequences are very effective in detecting such lesions. Treatment for CVST is still controversial; however, heparin has been reported as a safe and effective treatment. This is true even when CVST is accompanied by hemorrhagic lesions. Anti-seizure medication should be given to those who present with early seizures. Anticoagulation therapy for CVST averts aggravation of the thrombus, and allows for improvement of the occlusion lesion. This therapy is supported by European Federation of Neurological Societies guidelines. However, in cases of hemorrhagic presentation, appropriate therapy is highly controversial. It has been reported that 39% to 41% of CVST patients present with intracerebral hemorrhage, hemorrhagic venous infarcts, or isolated SAH.4) Although heparin and warfarin have been used for more than 50 years, newer oral anticoagulants (e.g., dabigatran, rivaroxaban, apixaban) might offer an alternative to traditional therapies for CVST, and pulmonary thromboembolism.5)
It is reassuring that although CVST is more usual in connection with puerperium than in the ordinary people, it also has a more favorable outcome. The mortality rate of CVST for all causes is 2% to 10%, but this is noteworthy lower in the puerperium population.6) This case emphasizes the importance of preserving a broad differential diagnosis in women presenting with postpartum seizure. Although eclampsia is the most reasonable cause, other rare conditions, that require decidedly different management, may be responsible.
Here, we presented an extremely rare case of a postpartum patient with CVST. The patient was successfully recovered with surgical decompression and anticoagulants. CVST should be considered in pregnant and young women. Superior sagittal sinus thrombosis is an uncommon complication with an unfavorable outcome after delivery. Timely diagnosis and treatment seem to be important in preventing deterioration of neurological function.
References
1. Borum SE, Naul LG, McLeskey CH. Postpartum dural venous sinus thrombosis after postdural puncture headache and epidural blood patch. Anesthesiology. 1997; 86:487–490. PMID: 9054267.

2. Ehtisham A, Stern BJ. Cerebral venous thrombosis: a review. Neurologist. 2006; 12:32–38. PMID: 16547444.
3. Ferro JM, Canhão P, Stam J, Bousser MG, Barinagarrementeria F. Prognosis of cerebral vein and dural sinus thrombosis: results of the International Study on Cerebral Vein and Dural Sinus Thrombosis (ISCVT). Stroke. 2004; 35:664–670. PMID: 14976332.
4. Ghandehari K, Riasi HR, Noureddine A, Masoudinezhad S, Yazdani S, Mirzae MM, et al. Safety assessment of anticoagulation therapy in patients with hemorrhagic cerebral venous thrombosis. Iran J Neurol. 2013; 12:87–91. PMID: 24250911.
5. Gross PL, Weitz JI. New anticoagulants for treatment of venous thromboembolism. Arterioscler Thromb Vasc Biol. 2008; 28:380–386. PMID: 18296593.

6. Lanska DJ, Kryscio RJ. Risk factors for peripartum and postpartum stroke and intracranial venous thrombosis. Stroke. 2000; 31:1274–1282. PMID: 10835444.

7. Park DS, Moon CT, Chun YI, Koh YC, Kim HY, Roh HG. Clinical characteristics of cerebral venous thrombosis in a single center in Korea. J Korean Neurosurg Soc. 2014; 56:289–294. PMID: 25371777.

8. Stam J. Thrombosis of the cerebral veins and sinuses. N Engl J Med. 2005; 352:1791–1798. PMID: 15858188.

FIGURE 1
(A) Initial brain computer tomography (CT) shows acute infarct in the right high parietal lobe subcortical/deep white matter and left cerebellar hemisphere. Also evident is subarachnoid hemorrhage on the right sylvian fissure, and frontotemporal convexity sulci. There is no apparent midline shift before exacerbation. (B) Follow-up brain CT shows the aggravating venous infarct, with focal hemorrhage on the right high frontoparietal lobe, and swelling after exacerbation.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download