Abstract
Lumbar fusion using the pedicle screw system is a popular operative procedure, with favorable clinical results and high fusion rates. However, the risk of adjacent segment disease after lumbar fusion is problematic. We report a complicated case of severe retrolisthesis at L3-4 level following dynamic interspinous process stabilization at L2-3 level and a fusion at L4-5 level. The radiological and clinical findings of this complication are discussed, and a review of the literature is presented.
Instrumented spinal fusion has been recommended for anticipated postoperative instability after wide decompression, unstable spondylolisthesis, and degenerative scoliosis. However, instrumented fusion poses the risk of higher morbidity, adjacent segment disease (ASD), and mortality in geriatric patients.5) In particular, the development of ASD is problematic because it can necessitate further surgical intervention and adversely affect functional outcomes.8) Furthermore, the recent dramatic increase in the number of spinal fusions performed has been accompanied by a commensurate increase in ASD. The concept of dynamic posterior stabilization was introduced to overcome the shortcomings associated with screw fixation and fusion in patients with neurogenic intermittent claudication due to lumbar spinal stenosis.9) The procedure involves distraction of the posterior elements of adjacent vertebral bodies, and increase of canal and foraminal dimensions at the expense of limiting spine extension. Here, we report a complicated case of severe retrolisthesis at L3-4 level following dynamic interspinous process stabilization at L2-3 level, and fusion at L4-5 level with a review of relevant literature.
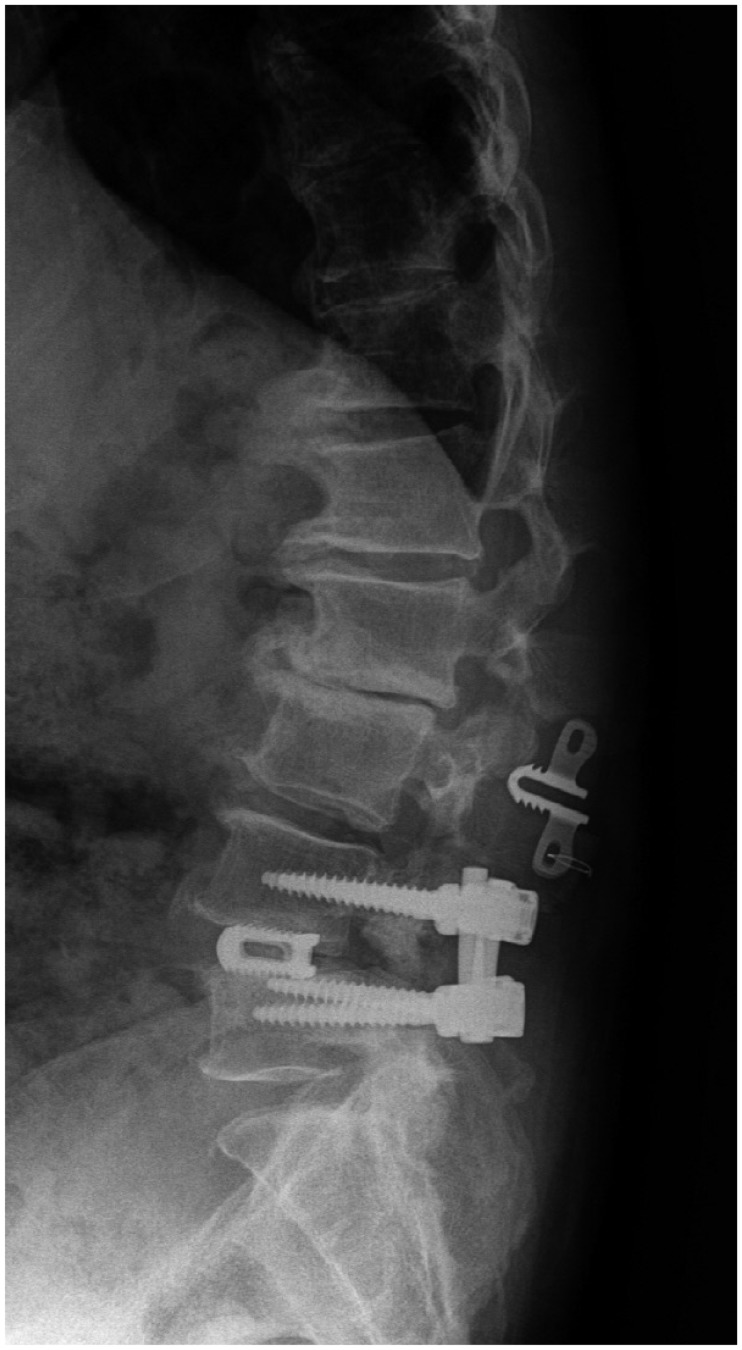
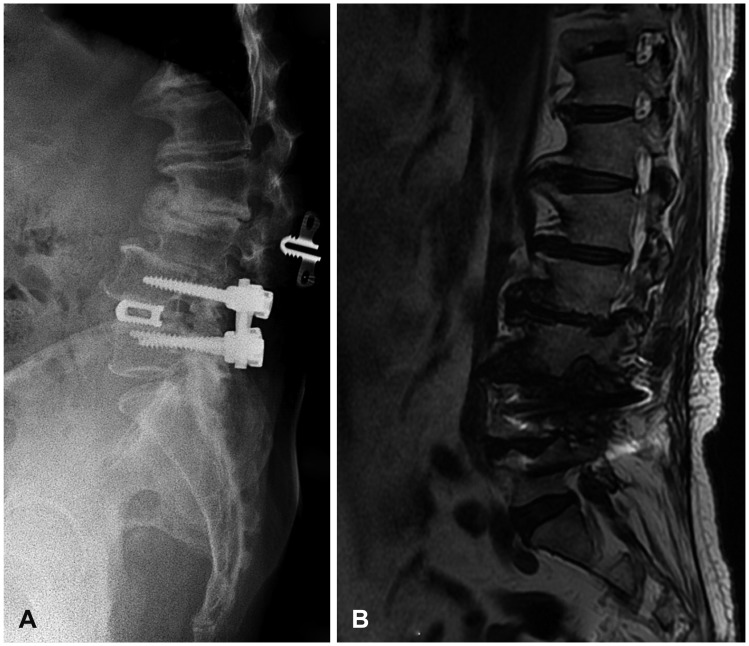
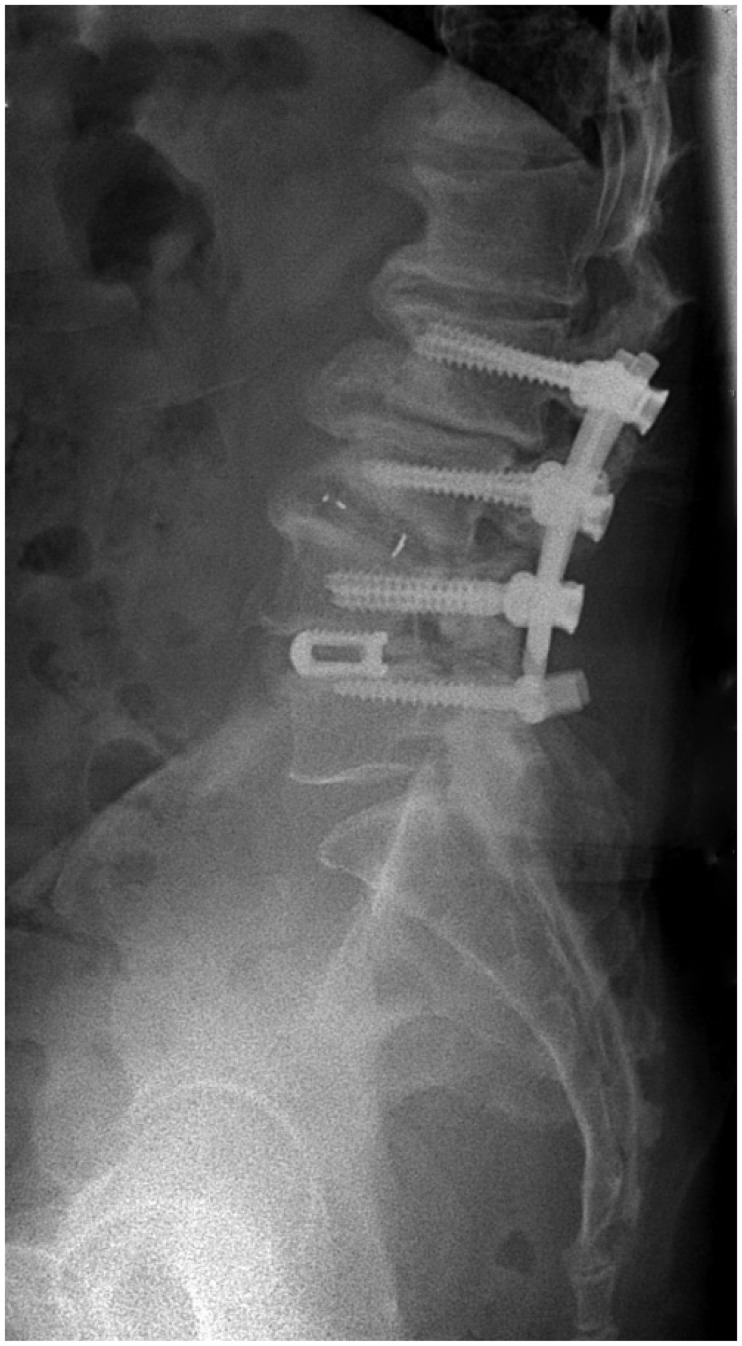
A 71-year-old man had disabling pain with claudication in both legs for 3 years before admission. Conservative treatment failed to improve his symptoms, and radiological studies, including simple radiographs and magnetic resonance imaging (MRI), revealed central stenosis at L2-3 and L3-4, and degenerative spondylolisthesis at L4-5 (Figure 1). Preoperative laboratory tests and bone marrow density (BMD) results were all within normal range. He underwent L4-5 posterior lumbar interbody fusion (PLIF) using titanium threaded cages with screw fixation, and simultaneous L2-3 and L3-4 decompression with “interspinous U” insertion at L2-3 level (Figure 2). Immediately after surgery, his presenting symptoms were much improved. However, at 3-month follow-up, he complained of back pain, late-onset back discomfort, and reduced range of motion. There was no neurologic deficit, and bowel and bladder function was normal. However, radiographs of the lumbar spine showed retrolisthesis at the L3 vertebra (Figure 3). At the patient's request, he was treated conservatively with anti-inflammatory medication, muscle relaxants, and bed rest. However, the back and radiating pain in both legs were aggravated and he was not able to walk independently. At 6-month postoperative follow-up, radiographs and MRI revealed aggravated stenosis at the L2-3 level and severe stenosis with retrolisthesis at the L3-4 level (Figure 4). He then underwent posterior fusion at L2-3 and interbody fusion at L3-4 with instrumentation from L2 to L4 (Figure 5). After surgery, complete pain relief was achieved and he was able to ambulate without difficulty. He complained only of mild back stiffness when walking, at 20 months after revision surgery.
Spinal fusion including PLIF provides posterior fusion and anterior column support, and is a common surgery for degenerative spondylolisthesis. Unfortunately, fusion alters the normal biomechanics of the spine, and a loss of motion at fused levels is compensated for by increasing motion at adjacent unfused segments.10) The resulting degeneration that develops at mobile segments above and below a fused spinal segment constitutes ASD. Disc degeneration is a common finding adjacent to a fused segment, and listhesis, instability, hypertrophic facet joint arthritis, herniated nucleus pulposus, and stenosis have also been reported as ASD.6) Theoretically, dynamic stabilization alters the movements and load transmissions of adjacent segments by restricting motion in the direction or plane that produces pain, but otherwise allows a full range of motion.912) The hypothesis that could decrease the stress on the adjacent segments, led to the development of various dynamic stabilization devices. However, biomechanical comparison study showed no significant difference between interspinous device and fusion device in terms of protection of adjacent segments.
Hartmann et al.7) reported that the interspinous and rigid device caused a significant increase of range of motion (ROM) at adjacent levels during all directions of motion.
Moreover, the interspinous spacer implants are designed to make increased segmental kyphosis at the treated level. As a result, this segmental kyphosis can accelerate the retrolisthesis on the adjacent level as a compensatory mechanism to maintain a global balance.211)
In the present case, to resolve ASD, we performed decompression and interspinous U stabilization at the upper adjacent L2-3 level and PLIF at L4-5 level for spinal stenosis. Although the mechanism involved remains uncertain, alterations in biomechanical stress appear to play a pivotal role in the development of ASD. Numerous biomechanical studies have confirmed that the fusion process imposes significant additional stress on adjacent segments,4) and a radiographic analysis found that posterior fusion increased the mobility of remaining free segments.1) Furthermore, in addition to facet loading and increased mobility, intradiscal pressure is also increased; this has been shown to cause disc degeneration at adjacent levels in longitudinal animal studies.3) When facets and a disc degenerate, the translation of an adjacent segment may occur and produce retrolisthesis. Our patient unexpectedly experienced severe retrolisthesis at the adjacent intermediate segment despite insertion of an interspinous U at upper level and fusion at lower level. Initially, we believed that simultaneous dynamic stabilization at an adjacent stenotic level would prevent ASD, but it failed to do so, and severe retrolisthesis occurred. Interspinous implantation at above level combined with fusion surgery would increase the rate of complications in adjacent segment. This case suggests that the combined use of interspinous distraction device should be cautious during the lumbar fusion surgery.
We report a complicated case of severe retrolisthesis at an adjacent segment following combined fusion surgery and an interspinous U device insertion. Our experience emphasizes that the combined use of interspinous distraction device on an adjacent level should be cautious during the lumbar fusion surgery.
References
1. Axelsson P, Johnsson R, Strömqvist B. The spondylolytic vertebra and its adjacent segment. Mobility measured before and after posterolateral fusion. Spine (Phila Pa 1976). 1997; 22:414–417. PMID: 9055370.
2. Barrey C, Roussouly P, Le Huec JC, D'Acunzi G, Perrin G. Compensatory mechanisms contributing to keep the sagittal balance of the spine. Eur Spine J. 2013; 22(Suppl 6):S834–S841. PMID: 24052406.

3. Chen CS, Cheng CK, Liu CL, Lo WH. Stress analysis of the disc adjacent to interbody fusion in lumbar spine. Med Eng Phys. 2001; 23:483–491. PMID: 11574255.

4. Dekutoski MB, Schendel MJ, Ogilvie JW, Olsewski JM, Wallace LJ, Lewis JL. Comparison of in vivo and in vitro adjacent segment motion after lumbar fusion. Spine (Phila Pa 1976). 1994; 19:1745–1751. PMID: 7973970.

5. Deyo RA, Cherkin DC, Loeser JD, Bigos SJ, Ciol MA. Morbidity and mortality in association with operations on the lumbar spine. The influence of age, diagnosis, and procedure. J Bone Joint Surg Am. 1992; 74:536–543. PMID: 1583048.

6. Etebar S, Cahill DW. Risk factors for adjacent-segment failure following lumbar fixation with rigid instrumentation for degenerative instability. J Neurosurg. 1999; 90:163–169. PMID: 10199244.

7. Hartmann F, Dietz SO, Kuhn S, Hely H, Rommens PM, Gercek E. Biomechanical comparison of an interspinous device and a rigid stabilization on lumbar adjacent segment range of motion. Acta Chir Orthop Traumatol Cech. 2011; 78:404–409. PMID: 22094153.
8. Park P, Garton HJ, Gala VC, Hoff JT, McGillicuddy JE. Adjacent segment disease after lumbar or lumbosacral fusion: review of the literature. Spine (Phila Pa 1976). 2004; 29:1938–1944. PMID: 15534420.

9. Park SC, Yoon SH, Hong YP, Kim KJ, Chung SK, Kim HJ. Minimum 2-year follow-up result of degenerative spinal stenosis treated with interspinous u (coflex). J Korean Neurosurg Soc. 2009; 46:292–299. PMID: 19893715.
10. Refae HH. Nearby segment disease in the lumber spine. J Am Sci. 2013; 9:143–148.
11. Webb H, van Woerden H. Interspinous devices for lumbar stenosis-a review of the literature. Internet J Surg. 2003; 5:3059.
12. Yoon SM, Lee SG, Park CW, Yoo CJ, Kim DY, Kim WK. Late complications of the single level ‘interspinous U’ in lumbar spinal stenosis with mild segmental instability. Korean J Spine. 2008; 5:89–94.
FIGURE 1
Preoperative T2-weighted magnetic resonance imaging shows spinal stenosis at L2-3 and L3-4, and spondylolisthesis at L4-5.
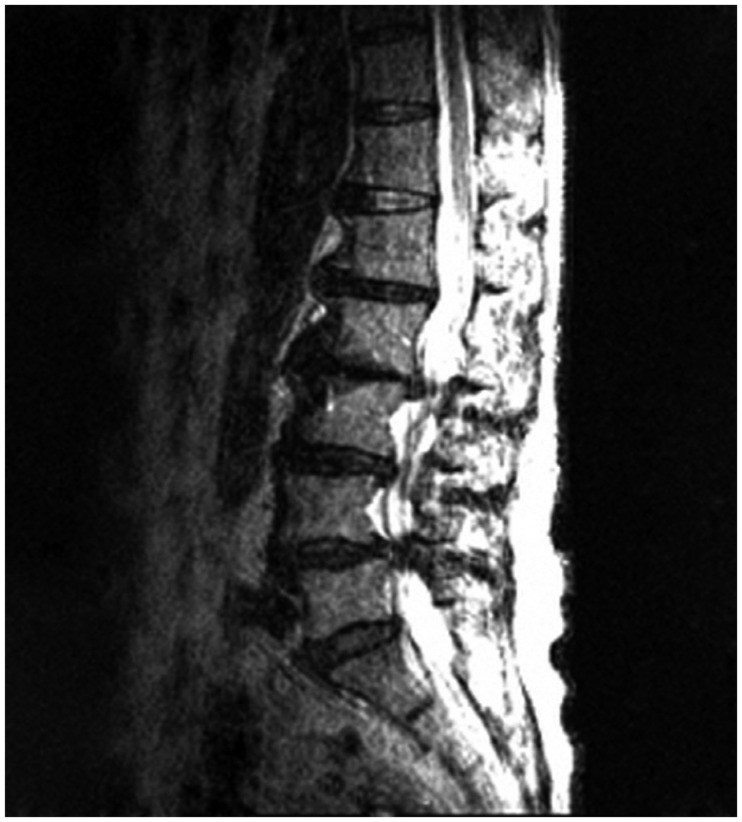
FIGURE 2
Simple lateral radiograph taken immediately after surgery shows no retrolisthesis at the L3-4 level.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download