Abstract
A 43-year-old man was admitted for head trauma after falling backward. The patient complained of diplopia. Unilateral internuclear ophthalmoplegia (INO) was diagnosed during the neurologic examination. Initially, no specific finding was shown on T2-weighted, T1-weighted, and fluid attenuated inversion recovery brain magnetic resonance image (MRI) or brain computed tomography (CT). However, susceptibility-weighted imaging (SWI) definitively demonstrated a tiny hemorrhage at the midline of the pontomesencephalic junction. The patient's symptom improved after 12 weeks. We discuss the clinical significance of SWI when traumatic INO due to a tiny hemorrhage is suspected.
Internuclear ophthalmoplegia (INO), is caused by lesions in the medial longitudinal fasciculus (MLF), and is characterized by paresis of adduction of the lateral gaze with horizontal jerk nystagmus in the contralateral abducting eye. Although several traumatic INOs have been reported in the literature, it is difficult to radiologically confirm INO when the lesion is tiny. This report presents a case of traumatic unilateral INO due to a tiny hemorrhage at the pontomesencephalic junction diagnosed using susceptibility-weighted imaging (SWI).
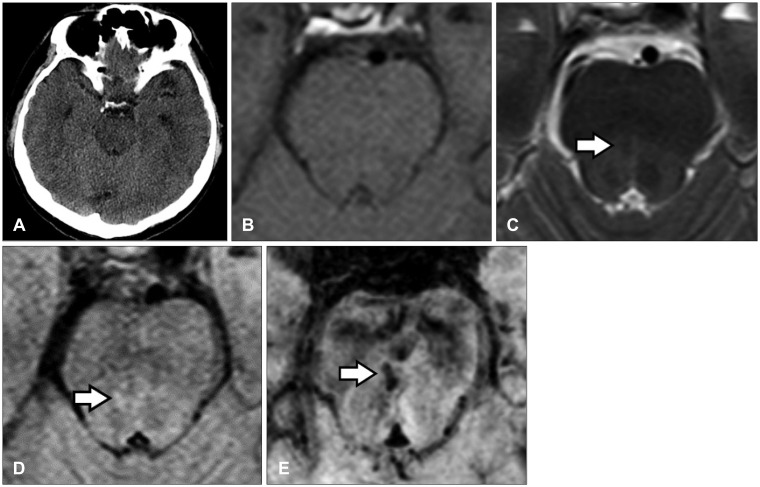
A 43-year-old man was admitted to our neurosurgical department for head trauma after falling backward. The patient had an occipital scalp laceration, brief loss of consciousness with retrograde amnesia, headache, dizziness, and diplopia with left gaze limitation of the right eye. Paresis of adduction of the lateral gaze in the right eye with horizontal jerk nystagmus in the contralateral abducting eye was observed during the neurologic examination at admission (Figure 1A). Initially, brain computed tomography (CT) performed in the emergency department revealed no specific finding (Figure 2A). However, 16 hours after injury, brain MRI showed a faint signal change in the right midline pontomesencephalic junction (Figure 2B-D). Eventually, SWI was performed, which definitively demonstrated a tiny hemorrhage (Figure 2E). Within 12 weeks, the patient's gaze abnormality was fully resolved, and patient reported no subjective complaint of diplopia (Figure 1B).
The ocular motor abnormalities of the present patient were consistent with unilateral INO. The most common cause of unilateral INO is a small paramedian pontine infarction, whereas the most common cause of bilateral INO is demyelinating plaque associated with multiple sclerosis.1415) Occasionally, INO is an unexplained consequence often associated with mild head injury.236)
The paramedian pontine reticular formation allows a horizontal conjugate gaze by simultaneously innervating the ipsilateral lateral rectus through the abducens neurons and the contralateral medial rectus through the fibers that originate in the ipsilateral internuclear neurons of the abducens nucleus and cross to traverse the MLF on the opposite side. A lesion in the MLF results in paresis of adduction of the lateral gaze.
The pathogenesis of the isolated damage to the MLF associated with head trauma is unclear, but several mechanisms have been suggested. Common hypotheses on the anatomical origin of post-traumatic MLF injury include differential displacement of the brainstem with resultant stretching of the MLF fibers,12) shearing forces in the brainstem caused by a blow to the head,8) and shearing forces caused by the angular acceleration or deceleration of the head upon impact.10) The shearing forces generated by angular movement exert the maximal effect where the difference between the densities of the cerebrospinal fluid and the adjacent neural tissue is the greatest. Because the MLF is located near the aqueduct and the floor of the fourth ventricle, it is vulnerable to these shearing forces. The posterior portion of the brainstem can be displaced downwardly than the anterior portion because the latter is tethered by small penetrating arteries of the basilar artery.12) Therefore, the shearing forces can create a temporary downward displacement of the posterior brainstem and cause shear injury to the MLF.7) Furthermore, the shearing forces within the brainstem can damage the perforating branches of the basilar artery, resulting in decreased blood flow or focal brainstem hemorrhage.13) In addition, the formation of a subdural hematoma causes a mass effect on the MLF fibers.8)
In most cases, MRI is used to demonstrate the MLF lesion.5111320) Although the standard method to the detect brain hemorrhage is computed tomography CT, but MRI may be as reliable as CT for detecting small hemorrhage associated with trauma.418) But, as we know, conventional MRI can fail to demonstrate a tiny hemorrhage in some patients. If the hemorrhage is very tiny in the brain stem, neuro-images, including brain MRI, may reveal a normal brainstem finding in a patient with traumatic INO.6) Few studies have been conducted in previously documented cases of traumatic INO to correlate structural lesions with possible underlying mechanisms,19) and no previous report had demonstrated microhemorrhage in a traumatic INO case using SWI. The extremely high sensitivity of SWI is particularly suited for the visualization and detection of traumatic hemorrhages, helping correlate clinical findings with the underlying anatomical lesion.1) It uses a high-resolution, completely velocity-compensated, three-dimensional gradient-recalled echo sequence based on both magnitude and phase data. Changes in the signal depend on the paramagnetic properties of deoxyhemoglobin in acute hemorrhage and the intravascular spontaneous blood oxygen-level dependent effect.17) SWI has recently been introduced as a tool to visualize venous vasculature and cerebral microhemorrhages based on the susceptibility difference between deoxyhemoglobin and the surrounding brain tissue.91618)
In this case report, we demonstrated that a traumatic microhemorrhage of the right MLF was responsible for the unilateral INO that presented immediately after head trauma and that SWI was more sensitive than other imaging to identify traumatic INO (Figure 2B-E). It was difficult to identify the cause of the INO using conventional images. T2-weighted, fluid-attenuated inversion recovery image, and isosignal on T1-weighted images showed a faint signal change (Figure 2B-D). But it was difficult to confirm the lesion as a hemorrhage. Eventually, SWI was performed, which showed a prominent hypointense spotty lesion (Figure 2E). As our case demonstrates, the SWI can be useful in precise identification of the anatomical lesions that correlate with the SWI. This technique may improve the diagnostic level of INO by showing greater accuracy for small hemorrhages in the pontomesencephalic junction.
References
1. Akiyama Y, Miyata K, Harada K, Minamida Y, Nonaka T, Koyanagi I, et al. Susceptibility-weighted magnetic resonance imaging for the detection of cerebral microhemorrhage in patients with traumatic brain injury. Neurol Med Chir (Tokyo). 2009; 49:97–99. PMID: 19318732.

2. Baker RS. Internuclear ophthalmoplegia following head injury. Case report. J Neurosurg. 1979; 51:552–555. PMID: 479939.
3. Beck RW, Meckler RJ. Internuclear ophthalmoplegia after head trauma. Ann Ophthalmol. 1981; 13:671–675. PMID: 7258960.
4. Bradley WG Jr. MR appearance of hemorrhage in the brain. Radiology. 1993; 189:15–26. PMID: 8372185.

5. Chan JW. Isolated unilateral post-traumatic internuclear ophthalmoplegia. J Neuroophthalmol. 2001; 21:212–213. PMID: 11725189.

6. Constantoyannis C, Tzortzidis F, Papadakis N. Internuclear ophthalmoplegia following minor head injury: a case report. Br J Neurosurg. 1998; 12:377–379. PMID: 10070436.

7. Crompton MR. Brainstem lesions due to closed head injury. Lancet. 1971; 1:669–673. PMID: 4101614.
8. Devereaux MW, Brust JC, Keane JR. Internuclear ophthalmoplegia caused by subdural hematoma. Neurology. 1979; 29:251–255. PMID: 571072.

9. Fiebach JB, Schellinger PD, Gass A, Kucinski T, Siebler M, Villringer A, et al. Stroke magnetic resonance imaging is accurate in hyperacute intracerebral hemorrhage: a multicenter study on the validity of stroke imaging. Stroke. 2004; 35:502–506. PMID: 14739410.
10. Hardman JM. The pathology of traumatic brain injuries. Adv Neurol. 1979; 22:15–50. PMID: 384769.
11. Hsu HC, Chen HJ, Lu K, Liang CL. Reversible bilateral internuclear ophthalmoplegia following head injury. Acta Ophthalmol Scand. 2001; 79:57–59. PMID: 11167289.

12. Johnson RT, Yates PO. Brain stem haemorrhages in expanding supratentorial conditions. Acta Radiol. 1956; 46:250–256. PMID: 13361934.

13. Jung DS, Park KP. Posttraumatic bilateral internuclear ophthalmoplegia with exotropia. Arch Neurol. 2004; 61:429. PMID: 15023822.

14. Keane JR. Traumatic internuclear ophthalmoplegia. J Clin Neuroophthalmol. 1987; 7:165–166. PMID: 2958510.
15. Kim JS. Internuclear ophthalmoplegia as an isolated or predominant symptom of brainstem infarction. Neurology. 2004; 62:1491–1496. PMID: 15136670.

16. Liang L, Korogi Y, Sugahara T, Shigematsu Y, Okuda T, Ikushima I, et al. Detection of intracranial hemorrhage with susceptibility-weighted MR sequences. AJNR Am J Neuroradiol. 1999; 20:1527–1534. PMID: 10512241.
17. Ogawa S, Lee TM, Kay AR, Tank DW. Brain magnetic resonance imaging with contrast dependent on blood oxygenation. Proc Natl Acad Sci U S A. 1990; 87:9868–9872. PMID: 2124706.

18. Schellinger PD, Jansen O, Fiebach JB, Hacke W, Sartor K. A standardized MRI stroke protocol: comparison with CT in hyperacute intracerebral hemorrhage. Stroke. 1999; 30:765–768. PMID: 10187876.

19. Strauss C, Ganslandt O, Huk WJ, Jonas JB. Isolated unilateral internuclear ophthalmoplegia following head injury: Findings in magnetic resonance imaging. Neuroophthalmology. 1995; 15:15–19.

20. Walsh WP, Hafner JW Jr, Kattah JC. Bilateral internuclear ophthalmoplegia following minor head trauma. J Emerg Med. 2003; 24:19–22. PMID: 12554035.

FIGURE 1
Neuro-ophthalmologic examination of the patient. (A) One day after head trauma. (B) Twelve weeks after head trauma.
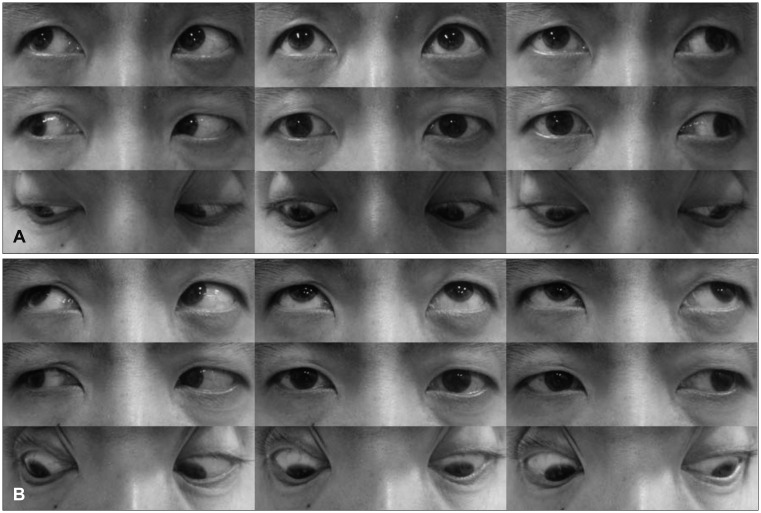
FIGURE 2
Neuro-image findings of the patient. (A) Brain computed tomography. (B) T1-weighted image (WI). (C) T2-WI. (D) Fluid-attenuated inversion recovery image. (E) Susceptibility-WI (SWI). The white arrows in C, D and E indicate signal changes in the pontomesencephalic junction. The SWI E most definitely revealed a microhemorrhage.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download