Abstract
A 21-year-old female presented with acute epidural hemorrhage (EDH) on the left temporal region associated with skull fracture after traffic accident. She was neurologically deteriorated at four-hour after an admission, and follow-up computed tomography revealed increased amount of EDH. Under the general anesthesia, emergency craniotomy was performed. During the surgery, massive bleeding from the base of middle cranial fossa was observed. However, we could not identify an origin of bleeding and foramen spinosum due to brain swelling and obscured surgical field. Consequently, her systolic blood pressure was dropped to 60 mm Hg with >110 beat/min of heart rate. Therefore, we decided to perform an intraoperative angiography after gauze packing into the middle cranial fossa. Intraoperative angiography showed a large pseudoaneurysm with massive contrast leakage of the middle meningeal artery (MMA). Intraoperative endovascular embolization of the pseudoaneurysm and MMA by using n-butyl-2-cyanoacrylate was done. After that, her vital sign became stable, and we could complete the operation after the achievement of adequate hemostasis. Intraoperative angiography and endovascular embolization of MMA was effective in achieving adequate hemostasis in case with brisk bleeding from the middle cranial fossa could not be controlled in an open surgical field.
Acute epidural hemorrhage (EDH) represents one of the most urgent neurosurgical lesions, and most frequently occur as a result of skull fracture with subsequent damage to the middle meningeal artery (MMA). In most cases, arterial bleeding focus could be identified and controlled in an open surgical field. On the other hand, recent advance in endovascular surgery have led to apply such technique to various craniofacial lesions. There are some published reports to treat EDH by using endovascular surgery without an open surgery.258) In the present study, we describe the intraoperative endovascular embolization to occlude a pseudoaneurysm and contrast leakage from the MMA in case with brisk bleeding from the middle cranial fossa could not be controlled in an open surgical field.
A 21-year-old female patient presented with headache via emergency room after traffic accident. Her vital sign was stable without any neurological deficits at presentation. Computed tomography (CT) revealed an EDH on the left temporal region (Figure 1A), and fractures of pelvic bone and both clavicles were also diagnosed via plane radiography. Four-hour after an admission, she suffered abrupt neurological deterioration with 11 of Glasgow Coma Scale score. Follow-up CT showed an increased amount of EDH (Figure 1B), and we decided to perform an emergency craniotomy and hematoma evacuation under the general anesthesia. During the surgery, massive bleeding from the base of middle cranial fossa was observed. Even though aggressive hemostasis was attemped, we could not identify an origin of bleeding and foramen spinosum due to brain swelling and obscured surgical field. Eventually, her systolic blood pressure was dropped to 60 mm Hg with >110 beat/min of heart rate. Therefore, we decided to perform an intraoperative angiography after gauze packing into the middle cranial fossa.
An angled 5 Fr Envoy guiding catheter (Cordis Neurovascular, Miami Lakes, FL, USA) was advanced into the left external carotid artery (ECA) and intraoperative angiography was done. It demonstrated a large pseudoaneurysm and excessive contrast leakage from the MMA which appeared torn and irregular (Figure 2A). Embolization of the MMA was performed immediately after the angiography without systemic heparinization. The MMA was catheterized using a Excelsior SL-10 microcatheter (Stryker Neurovascular, Fremont, CA, USA) upto the orifice of a pseudoaneurysm, and 1.4 mL of 33% n-butyl-2-cyanoacrylate (NBCA) (Hystoacryl®; B. Braun, Melsungen, Germany) was infused occluding the pseudoaneurysm and MMA (Figure 2B). Completion control ECA angiography was confirmed complete occlusion of pseudoaneurysm of MMA and no contrast leakage from the MMA (Figure 2C). After that, her vial sign became stable, and we could complete the operation after the achievement of complete hemostasis.
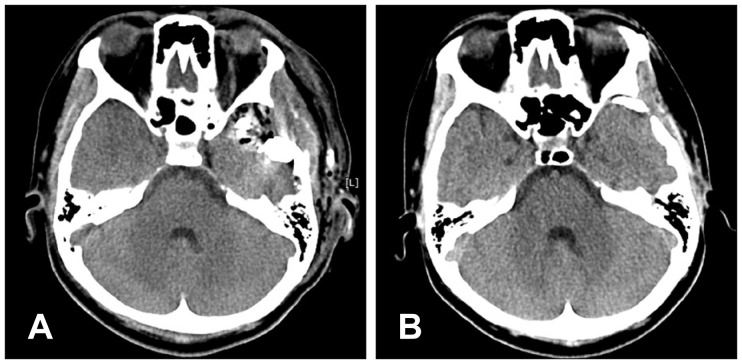
After the surgery, the patient immediately regained consciousness without any neurological deficits. Postoperative CT revealed no residual EDH with hyperdense materials in middle cranial fossa made by NBCA. CT 4 months after the operation revealed decreased amount of hyperdense materials in middle cranial fossa and no residual hematoma (Figure 3). After residual orthopedic problems were treated, she could be discharged 2 months after the brain surgery without any neurological deficits.
Acute EDH is one of the most common intracranial traumatic lesions to require emergent surgery under general anesthesia.1) The bleeding source, typically a branch of the MMA, can generally be controlled with bipolar diathermy. Occasionally, the main trunk of the MMA is ruptured because of a fracture involving the petrous bone. In these cases, hemostasis can be achieved by packing the foramen spinosum with bone wax or a combination of bone wax and surgicel.7) In the present case, however, we could not achieve adequate hemostasis due to the brain swelling and obscured surgical filed by brisk bleeding from the base of middle cranial fossa. It made the patient unstable during the surgery, and almost contributed to surgical mortality.
Endovascular access to MMA is relatively easy, and embolization of MMA could be achieved in a short time without systemic heparinization. We used NBCA to occlude MMA, and we achieved complete occlusion of pseudoaneurysm of MMA. During the procedure, NBCA was extravasated into the epidural space. Because a dura matter was intact, however, intra-axial tissue damage was not occurred by using NBCA. Packed cottonoids and gauzes might be adhered with NBCA and dura matter, however, it could be meticulously dissected with Metzenbaum seizure and double-handed dissector, and almost removed. Tiny pieces of cottonoids were remained, however, they did not lead to infection.
Traumatic intracranial vascular injury would lead to severe complication. Intracranial pseudoaneurysms are less than 1% of all intracranial aneurysms, and mostly associated with head trauma. Carotid artery is usually involved, and pseudoaneurysm of MMA is rare. About 70% of traumatic MMA pseudoaneurysms are associated with a fracture crossing the MMA in the temporal region.3)
Some authors favor an early treatment of the pseudoaneurysm of MMA due to the possible severe consequences of acute and delayed hemorrhage.4568) Whether the simple presence of a pseudoaneurysm, however, is an indication for intervention is unclear, especially in cases of small amount of EDH which are not needed to operate.3) Regardless of this controversy, intraoperative endovascular embolization of MMA seems to be obviously beneficial, especially in case of brisk bleeding which could not be controlled in open surgical field.
References
1. Bullock MR, Chesnut R, Ghajar J, Gordon D, Hartl R, Newell DW, et al. Surgical management of acute epidural hematomas. Neurosurgery. 2006; 58(3 Suppl):S7–S15. discussion Si-SivPMID: 16710967.

2. de Andrade AF, Figueiredo EG, Caldas JG, Paiva WS, De Amorim RL, Puglia P, et al. Intracranial vascular lesions associated with small epidural hematomas. Neurosurgery. 2008; 62:416–420. discussion 420-421PMID: 18382319.

3. Jussen D, Wiener E, Vajkoczy P, Horn P. diagnosis and endovascular treatment of two cases and review of the literature. Neuroradiology. 2012; 54:1133–1136. PMID: 22218611.
4. Kinoshita Y, Yasukouchi H, Tsuru E, Okudera T, Yokota A. [Delayed epidural bleeding caused by traumatic pseudoaneurysm of the middle meningeal artery: case report]. No Shinkei Geka. 2004; 32:1139–1143. PMID: 15570878.
5. Lammy S, McConnell R, Kamel M, Rennie I, Al-Haddad S.is there a role for endovascular treatment? Br J Neurosurg. 2013; 27:383–385. PMID: 22946965.
6. Lim DH, Kim TS, Joo SP, Kim SH. Intracerebral hematoma caused by ruptured traumatic pseudoaneurysm of the middle meningeal artery: a case report. J Korean Neurosurg Soc. 2007; 42:416–418. PMID: 19096582.
7. Pascual JM, Prieto R. Surgical management of severe closed head injury in adults. In : Quinones-Hinojosa A, editor. Schmidek and sweet operative neurosurgical techniques. ed 6. Philadelphia, PA: Elsevier;2012. p. 1513–1538.
8. Suzuki S, Endo M, Kurata A, Ohmomo T, Oka H, Kitahara T, et al. Efficacy of endovascular surgery for the treatment of acute epidural hematomas. AJNR Am J Neuroradiol. 2004; 25:1177–1180. PMID: 15313705.
FIGURE 1
Initial brain computed tomography reveals acute epidural hemorrhage (EDH) on the temporal region (A) and follow-up brain CT obtained 4 hours after admission shows increased amount of EDH (B).
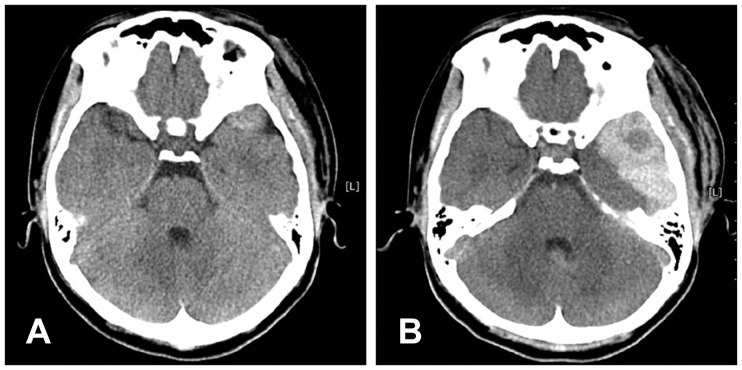
FIGURE 2
Intraoperative angiography of the left external carotid artery (A) depicts a large pseudoaneurysm (white arrow in A) and contrast leakage (white arrowheads in A) from the middle meningeal artery (MMA) which appeared torn and irregular. Native image (B) demonstrates glue case in a pseudoaneurysm, MMA and extravasation into the epidural space. Completion control angiography (C) shows complete occlusion of a pseudoaneurysm and MMA without extravasation.
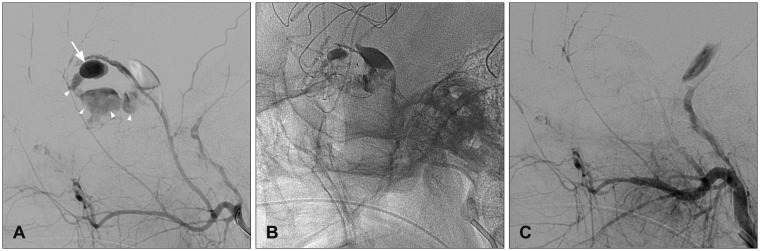
FIGURE 3
Postoperative computed tomography (CT) (A) shows no residual epidural hemorrhage with hyperdense materials in middle cranial fossa made by n-butyl-2-cyanoacrylate. CT 4 months after the operation (B) revealed decreased amount of hyperdense materials in middle cranial fossa and no residual hematoma.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download