Abstract
Background
Heart failure is a rare condition of thyrotoxicosis. We report a case of thyrotoxicosis-inducing heart failure.
Case report
A 29-year old female had been suffered from thyrotoxicosis for 3 years without proper medication. She complained progressive dyspnea and palpitation with atrial fibrillation with rapid ventricular response. Marked cardiomegaly, and severe right ventricular dysfunction with biatrial enlargements were found on Two-dimensional (2D) echocardiography. We treated her with medications for heart failure and thyrotoxicosis, and the patient's symptoms and objective cardiac functions are improved after two weeks.
Thyrotoxicosis can cause many cardiovascular manifestations including palpitation, arrhythmia, cardiomegaly, peripheral edema, and angina. Severe thyrotoxicosis could worsen sinus tachycardia or atrial fibrillation and leads to heart failure, which is called tachycardia-induced cardiomyopathy. We report a case of a patient with severe heart failure due to uncontrolled hyperthyroidism which was completely recovered after comparably short-term treatment with anti-thyroid drugs and treatment of heart failure.
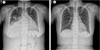
A 29-year-old female patient visited our hospital emergency department with aggravating dyspnea for 3 days. She had underlying Graves' disease for 3 years but did not have regular medication, and she had no other underlying diseases or risk factors that could cause severe heart failure. Physical examination revealed decreased breathing sound in right lower lung field and pitting edema in extremities. Chest X-ray showed marked cardiomegaly with cardiothoracic (CT) ratio 0.8 and right side pleural effusion. Pleural fluid analysis showed transudate effusion with serum albumin 3.1 g/dL and pleural fluid albumin 1.2 g/dL. On electrocardiography (ECG), she showed atrial fibrillation with rapid ventricular response. In laboratory findings, she had subclinical hyperthyroidism with thyroid stimulating hormone (TSH) 0.05 uIU/mL, T3 1.32 ng/mL and free T4 1.45 ng/dL, and elevated pro-B type natriuretic peptide (pro-BNP) with 843 pg/mL. Two dimensional (2D) echocardiography showed biatrial enlargements (left atrial dimension 48.5 mm), severe right ventricular dysfunction, moderate left ventricular systolic dysfunction with decreased ejection fraction (39.8%), severe mitral regurgitation (Grade III), and severe tricuspid regurgitation (Grade III-IV) due to coaptation failure. We diagnosed thyrotoxic heart failure and performed electric cardioversion for rhythm conversion, and the rhythm changed to sinus rhythm. She was treated with inotropics (dopamine) due to low systolic blood pressure (80 mmHg), medication for heart failure (digoxin, aldactone, beta blocker, and loop diuretics), and methimazole 5 mg per day for Graves' disease. After two weeks of treatment, her symptoms were gradually improved. On follow-up thyroid function tests show normal values with TSH 0.03 uIU/mL, T3 0.69 ng/mL, and free T4 0.49 ng/dL. ECG remained normal sinus rhythm, and cardiomegaly improved with CT ratio 0.55 on follow-up chest X-ray two weeks later (Fig. 1, 2). Follow-up 2D echocardiography showed improved right ventricular dysfunction, and left ventricular ejection fraction (54%) with moderate mitral regurgitation (Grade II-III) and mild tricuspid regurgitation (Fig. 3). Her general condition was tolerable, and was discharged without any discomforts. So she was discharged with methimazole 5 mg per day.
After discharge, she had no other heart failure symptoms and follow-up laboratory tests on out-patient department were stabilized with decreased pro-BNP 527.3 pg/mL, TSH 0.03 uIU/mL, T3 1.14 ng/mL, and free-T4 0.85 ng/dL. Methimazole dose was decreased to 2.5 mg per day after 2 months, and she showed tolerable state until her recent follow-up.
This patient had uncontrolled hyperthyroidism, and gradually developed dyspnea with marked cardiomegaly, right side pleural effusion, atrial fibrillation, and severe right ventricular dysfunction with moderate left ventricular dysfunction. After proper treatments of heart failure and thyrotoxicosis, clinical symptoms were markedly improved and cardiac functions on follow-up 2D echocardiography recovered in two weeks.
Severe heart failure in thyrotoxicosis is a rare manifestation, but its prognosis is comparably favorable.1,2 Goland et al. reported two case of dilated cardiomyopathy in hyperthyroidism, and they had recovered without any sequel.3 Cardiac manifestations in thyrotoxicosis are well established, including palpitation, enlargement of the heart, high output heart failure, hypertrophic cardiomyopathy, angina syndrome without evidence of coronary artery, and even sudden cardiac death.4-6 Moreover, atrial fibrillation or sinus tachycardia can be developed, which may be caused by disruption of calcium circulation to heart cells and structural changes of the heart.7-9 Hong et al. suggested that right ventricular dysfunction combined with thyrotoxicosis-associated left ventricular dysfunction was not secondary to thyrotoxicosis-associated left ventricular dysfunction, and anti-thyroid hormone treatment might improve right ventricular dysfunction.10 In our case, severe cardiomegaly and biventricular dysfunctions were improved with comparably short term anti-thyroid hormone treatment. She had no other underlying condition except hyperthyroidism affected to severe heart failure, and the response to anti-thyroid hormone treatment was favorable, even her thyroid function tests showed no significant changes. So we recommend detailed examination of patient's medical history should be acquired with treatment for heart failure. In addition, it is important to treat the underlying cause of heart failure despite poor management before admission.
Figures and Tables
Fig. 1
Initial electrocardiography (ECG) and follow-up ECG. Initial atrial fibrillation (A) was converted to normal sinus rhythm (B).

References
1. Umpierrez GE, Challapalli S, Patterson C. Congestive heart failure due to reversible cardiomyopathy in patients with hyperthyroidism. Am J Med Sci. 1995; 310:99–102.

2. Ebisawa K, Ikeda U, Maruta M. Irreversible cardiomyopathy due to thyrotoxicosis. Cardiology. 1994; 84:274–277.

3. Goland S, Shimoni S, Kracoff O. Dilated cardiomyopathy in thyrotoxicosis. Heart. 1999; 81:444–445.

4. Woeber KA. Current concepts: Thyrotoxicosis and the Heart. N Engl J Med. 1992; 327:94–98.
5. Ladénson PW. Thyrotoxicosis and the heart: something old and something new. J Clin Endocrinol Metab. 1993; 77:332–333.

6. Polikar R, Burger AG, Scherrer U, et al. The thyroid and the heart. Circulation. 1993; 87:1435–1441.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download