Abstract
Purpose
This study was conducted to examine differences in health care utilization and related costs between before and after the introduction of the designated doctor system, and to find out factors making the differences.
Methods
Data were collected from 200 medical aid beneficiaries having one or more chronic diseases, registered in the designated doctor system during the year of 2012, and the relationship between the use of health services and claimed medical expenses was analyzed through paired t-test and multiple regression analysis using the SPSS 18.0 program.
Results
There was a decrease in the number of total benefit days and the number of outpatient and medication days, but some cases showed an increase after the designation of medical institution. In general, hospital stay increased after the introduction of the system. However, the number of medical institutions utilized was reduced in most cases after designation. Conversely, medical expenses increased in most cases after the designation of medical institution.
Figures and Tables
Table 1
General Characteristics of Beneficiaries with Designated Doctor System (N=200)

Table 2
Characteristics of Designated Doctor System (N=200)
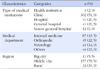
Table 3
A Change in Trend of Health Care Utilisation before and after the Introduction of Designated Doctor System based on the Characteristics of Individual Patient

Table 4
A Change in Trend of Health Care Utilisation before and after the Introduction of Designated Doctor System based on the Characteristics of Health Care Facilities

Table 5
Factors related to Change of Total Beneficial Day and Outpatient Day

References
1. Ministry of Health & Welfare. 2014 guideline of medicaid management. Sejong: Ministry of Health & Welfare;2014. p. 510.
2. Shin HU, Shin YS, Hwang DK, Yoo YS, Choi GC, Lim SJ. Report No.: 2008-18-5. Monitoring the designated doctor system. Research Report. Seoul: Korea Institute for Health and Social Affairs;2008. 12.
3. Ministry of Health & Welfare. From July implementation of type 1 medicaid beneficiaries copayments and designated doctor system, operation of medical aid qualification management system [Internet]. Gwacheon: Ministry of Health & Welfare;2007. cited 2015 August 16. Available from: http://www.mohw.go.kr/user.tdf?a=user.tbdata.BoardApp&c=2002&board_id=gp_tb_data&seq=41480&cp=2&pg=1&npp=10&mc=P_04_01&skin=p_new_m4_common&.
4. Ministry of Health & Welfare. Findings of research paper on "actual status of health care utilization by medical aid beneficiaries" [Internet]. Gwacheon: Ministry of Health & Welfare;2007. cited 2014 August 22. Available from: http://www.mohw.go.kr/user.tdf?a=user.tbdata.BoardApp&c=2002&board_id=gp_tb_data&seq=41707&cp=2&pg=1&npp=10&mc=P_04_01&skin=p_new_m4_common&silkuk.
5. Shin YS, Choi BH, Shin HU, Hwang DK, Eun SJ. Report No.: 2005-30. The research regarding the healthcare expenditure and medical treatment material service use actual condition and a improvement program. Policy Report. Seoul: Ministry of Health & Welfare. Korean Institute for Health and Social Affairs;2005.
6. Gwon GS. Report No.: MONO1201508314. Development of platforms for therapeutic technologies to control age-related chronic disessest. Research Report. Daejeon: Korea Research Institute of Bioscience & Biotechnology;2014.
7. Jung YH, Ko SJ, Kim EJ. Report No.: 2013-31-19. A study on the effective chronic disease management. Research Report. Seoul: Korea Institute for Health and Social Affairs;2013.
8. Lee JH. Introduction of familiy doctor system [Internet]. Seoul: Health Right Network;2009. cited 2014 August 22. Available from: http://www.konkang21.or.kr/bbs/board.php?bo_table=pds1&wr_id=965.
9. Lee JH, Choi YJ, Choi JS, Kim SR. Patient assessment of primary care under the designated practice scheme for medical aid beneficiaries, using the Korean Primary Care Assessment Tool (K-PCAT): A district of Seoul, South Korea. J Korean Med Assoc. 2012; 55(2):187–197. DOI: 10.5124/jkma.2012.55.2.187.

10. Lee JW, Yang SI, Kim KH. A study on influential factors on satisfaction with the use of medical services by the qualified recipients of medical aid (focusing on the period after the introduction of the selected medical center system). J Digit Convergence. 2014; 12(3):289–297. DOI: 10.14400/JDC.2014.12.3.289.
11. Lim SJ. The effect of case management for medicaid on healthcare utilization by the medicaid system. J Korean Acad Community Health Nurs. 2010; 21(4):375–385. DOI: 10.12799/jkachn.2010.21.4.375.
12. No SS. Medicaid recipients in accordance with the selection of medical aid agency change in health care utilization [master's thesis]. [Gwangju]: Chonnam National University;2013. 37.
13. Ministry of Health & Welfare. National Health Insurance Corporation. Medical care statistics. Seoul: National Health Insurance Corporation;2012. p. 723.
14. Hong SO. The effects of copayments on healthcare utilization in the type I medicaid beneficiaries [dissertation]. [Seoul]: Seoul National University;2009. 103.
15. Kim YO. Impact of implementing outpatient cost-sharing system to medical type 1 recipient on the health utilization and expenditure [master's thesis]. [Seoul]: Yonsei University;2008. 66.
16. Choi J, Oh JJ. The effects of designated doctor system on the health of medical aid beneficiaries. J Korean Acad Community Health Nurs. 2012; 23(4):438–445. DOI: 10.12799/jkachn.2012.23.4.438.
17. Shin YS. Direction to go for medical aid. Health Welf Policy Forum. 2010; 167:28–38.
18. Hong SW. Factors influencing health-related quality of life in Korean medicaid beneficiaries. J Korean Acad Nurs. 2009; 39(4):480–489. DOI: 10.4040/jkan.2009.39.4.480.

19. National Health Insurance Corporation. The first half of 2014 health insurance key statistics [Internet]. Seoul: National Health Insurance Corporation;2014. cited 2015August 16. Available from: http://www.nhis.or.kr/bbs7/boards/B0039/3156.
20. Korea Human Resource Development Institute for Health & Welfare. Quarternary period medical aid management experienced job training course. 1st ed. Cheongwon: Korea Human Resource Development Institute for Health & Welfare;2013. p. 129.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download