Abstract
Purpose
Metacarpal bone fracture is a commonly encountered. The authors applied a minimally invasive open reduction technique that comprises only a stab incision to treat metacarpal bone fractures, thereby minimizing complications that accompany traditional open reduction methods while retaining the advantages of closed reduction techniques.
Methods
A 5-year retrospective study was carried out of all patients who underwent surgical treatment performed by two separate hand surgeons. Total 37 patients were operated. Fourteen patients of conventional open reduction group and 23 patients of minimal invasive group were included in the study.
Metacarpal bone fracture is a commonly encountered upper limb trauma, comprising one fifth of upper extremity fractures and one half of hand fractures12. Treatment for metacarpal bone fractures can be either surgical or nonsurgical, and the former may further be divided into open reduction and closed reduction using percutaneous pinning3.
In many cases, metacarpal fractures can be treated nonoperatively. However, fractures with severe angulation45, rotation6, shortening7, unstable fractures such as long oblique fractures, fractures with bone loss, and multiple fractures3 require surgical management. Due to the lack of high-level evidence from prospective cohorts or randomized controlled trials, however, debate still exists on whether closed or open reduction technique produces optimal results589.
The open reduction technique may easily be applied to stable fractures, and is also favored when dealing with unstable fractures with poor maintenance of reduction. Open reduction is usually indicated for transverse shaft fractures that either are significantly displaced or have residual angulation of more than 10 degrees in the second and third metacarpals, 20 to 30 degrees in the ring metacarpal, and 30 to 40 degrees in the small finger metacarpal and indicated for most spiral and oblique fractures, particularly if there is evidence of a rotational deformity on physical examination, because fracture reduction is difficult to maintain by closed techniques and the anatomical positions of these bones may hinder complete reduction.
Authors applied a mini-open reduction technique that comprises only a stab incision to treat metacarpal bone fractures, thereby minimizing complications that accompany traditional open reduction methods while retaining the advantages of closed reduction techniques, and analyzed the results. This study was approved by the Institutional Review Board of the Catholic University of Korea. All data were analyzed anonymously and according to the principles in the Declaration of Helsinki (1975, revised in 2008).
Patients with isolated second to fifth metacarpal bone fractures that underwent surgical treatment at our institute from January 2010 through December 2015 were included and data were retrospectively reviewed in the study. Patients with other concomitant trauma, or those exhibiting a limited range of motion from previous traumatic event were excluded. A total of 37 patients were treated as subjects, with 14 patients (37.8% of total) under going open reduction and internal fixation (ORIF) using titanium plate and screws (open reduction group, group I), and 23 patients (62.2% of total) undergoing mini-open reduction (mini-open reduction group, group II).
All patients were admitted to the hospital through outpatient clinic or emergency room, and surgery was done under general anesthesia within two weeks from the date of the injury. Depending on the degree of fracture and degree of associated injury, the admission date was varied from pod 2 to 7. Pain control started with nonsteroidal anti-inflammatory drugs and applied pethidine intravenous (IV) when control was difficult and patients were treated with IV antibiotics until discharge. The patient maintained a short arm splint for 4–6 weeks.
Results in both groups were analyzed based on operation time, and the total sum score (ten being the highest score) given by two separate hand surgeons on a scale of one to five after reviewing post-reduction radiographic images. Also, other variables including the degree of recovered range of motion of the involved metacarpophalangeal (MCP) joint six months after the surgery, subjective pain reported by the patient using the visual analogue scale (VAS) postoperative two weeks, number of cases that required secondary procedures to release postsurgical adhesions, and postoperative complications were also evaluated. The surgical scar sites were also assessed after 6 months using the Vancouver scar scale (VSS).
We received informed consent from the patients to submit the imanges containing any part of the patient's body to the paper.
Under general anesthesia, a three to five centimeter-long dorsal incision was made depending on the location and the degree of the fracture. The periosteum of the metacarpal bone was exposed with careful dissection to avoid any injury to the extensor digitorum communis tendons and adjacent superficial veins and nerves. The periosteum was elevated for subsequent reduction and plate fixation, with the aid of bone holding forceps to maintain reduction if deemed necessary. Depending on the severity of the fracture, a 4 to 6-hole plate along with 8 to 12mm screws were used for bicortical plate fixation (Fig. 1). The periosteum was then closed using Vicryl 4-0 sutures, and anti-adhesion agent was applied before skin closure with 5-0 Vicryl and 5-0 Nylon sutures. Sutures were removed 10 to 14 days after the surgery, during a short arm splint was applied.
Under fluoroscopic guidance, a 3 mm sized longitudinal incision was made on the dorsum above the fracture site visualized, while taking care not to injure the extensor digitorum communis tendons. Authors reached the fracture site with gentle dissection using the Freer elevator (Fig. 2). The fractured segment was then reduced to appropriate position through simultaneous distal traction of the involved finger and direct palpation using the elevator (Fig. 3), while any intervening tissue was pulled aside to facilitate the procedure. A 0.9–1.1 mm sized Kirschner wire (K-wire) was inserted from the proximal side of the fractured metacarpal bone toward the opposite side of the bone to avoid injury to the MCP joint. The K-wire was advanced to include the whole fractured area, while maintaining the reduction and alignment with the help of the Freer elevator (Fig. 4). In patients with unfavorable fractures which reduction cannot be maintained with intramedullary pinning only, transverse pining method was utilized (Fig. 5). An anti-adhesion agent was applied through the stab incision site followed by skin closure, and the tip(s) of the K-wire was buried under the deep skin to minimize unwarranted interference on the range of motion.
In both groups, after the operation, the surgeons confirmed full range of motion of the MCP, proximal interphalangeal, and distal interphalangeal joint of the involved digit. Subsequent scar management and postoperative massage using silicone ointment and sheet were carried out. In the mini-open reduction group, the K-wire(s) was removed 4 weeks after the surgery.
Statistical analyses were conducted with an independent sample t-test, and p<0.05 was considered significant.
Statistical analyses was conducted using SAS software ver. 9.3 (SAS Institute, Cary, NC, USA).
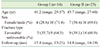
Patient demographic data are presented in Table 1. The mean age in group I and group II was 41.2 and 43.7 respectively, with no significant difference. Male patients were dominant in both groups. The number of cases of unfavorable fractures was 9 in group I (total 14) and 14 in group II (total 23), with no significant difference. The mean follow-up duration was 15.4 months in group I, and 14.8 months in group II. There is no significant difference in patients demographics between group I and group II.
The mean operative time was 41 minutes in group I and 24 minutes in group II, which was significantly shorter than the former (p=0.02). There was no significant difference between two groups in the mean radiological reduction result, with group I scoring 8.2±1.1 and group II scoring 8.5±0.9. The mean VAS score was 4.3±0.7 and 2.7±0.8 in each group, showing a significantly higher result in group I (p=0.02). The mean active range of motion of the MCP joint at six months was 88.4° in group I and 88.0° in group II, with no significant difference. In group I, there was one case that underwent an additional adhesiolysis at five months after the surgery, whereas group II required no further procedures; however, there was no significant difference between two groups.
Both groups had no major postoperative complications that required surgical intervention. There was one case of stitch abscess and one case of minimal wound disruption in group I, and two patients developed superficial infection at the wire insertion site in group II. All such minor complications were resolved with conservative care. Scar quality assessment using the VSS resulted in 5.7±1.1 in group I and 3.9±0.9) in group II, indicating superior outcome in the latter (p=0.03) (Table 2).
There exists yet no absolute guideline on operative techniques for treating metacarpal fractures. Before choosing a certain surgical technique, many variables such as the location of the fracture (intra-articular or extra-articular), pattern of the fracture (transverse, oblique, spiral or comminuted), or presence of any bony displacement must all be taken into consideration, as well as the surgeon's preference and skill3.
In addition to closed reduction, there are various open reduction fixation techniques depending on the type and position of the fracture. K-wires may be used in nearly any fracture pattern. Pinning technique is relatively easy, requires minimal dissection and minimizing soft tissue trauma. It can be used single or multiple and may be used in combination of other fixation technique. Composite wiring is used in a combination of K-wires. It provides additional stability and fracture compression and superior strength, stiffness, and approximation compared with crossed K-wires alone. Cerclage and interosseous wiring can be applicable for oblique and spiral metacarpal shaft fractures. These wires are rigid enough to permit early motion. But these techniques need additional dissection and are contraindication when there is bone loss, comminution, or osteopenia. Intramedullary fixation can be used alone and successfully employed for transverse fractures. It is easy to perform and allow active motion. Also, it has advantage of no exposed pins and secondary removal is unnecessary. But, rotational control may be difficult and in case of infection or re-fracture, hardware removal may be very difficult. External fixation can be indicated for highly comminuted open shaft fracture with or without bone loss and comminuted articular fracture and fractures with injury of loss of surrounding soft tissue. It also has disadvantage that prominence of the device make difficult for activities of daily life and there are highly risk of pin-site infection, may impede tendon gliding and cause of adhesion.
Debate still exists on whether closed reduction using K-wires or open reduction using plate and screws produces optimal results. Ozer et al.10 compared intramedullary nailing using K-wire with open reduction using plate and screws, and concluded that the former resulted in increased loss of reduction, more injury to MCP joint, and a higher rate of secondary procedures necessary to remove K-wires11. On the other hand, Greeven et al.12 reported that patients treated with open reduction showed a higher tendency to require secondary procedures such as tenolysis compared with those treated otherwise. In all three studies, there was no significant difference between patient groups regarding final functional outcome. Facca et al.13 held closed reduction to be superior to open reduction, as he reported that patients with fifth metacarpal neck fractures who were treated with locking plates exhibited paradoxical poor movement of MCP joint despite of early mobilization, compared with those treated with K-wire fixation.
Authors were able to directly manipulate the fracture site with surgical instrument through minimal skin incision, which enabled authors to constantly maintain the reduced position while inserting wires. In cases of unstable fractures, such method can facilitate primary bone healing better than simple closed reduction by allowing secure bone-to-bone contact. Fractures can be generally categorized into stable and unstable groups depending on whether reduction is well-maintained or not. Most surgeons opt for ORIF when treating unstable fractures, such as transversely displaced fractures, long spiral fractures, short oblique fractures, and displaced condyle fractures with more than 25% of articular surface involvement14. In unstable fractures, one of the main complications is metacarpal shortening due to poor reduction maintenance, and also angulation may develop; such outcomes are not uncommon when unstable fractures are managed simply with closed reduction and K-wire fixation. Authors were able to minimize such complications by inserting a Freer elevator or a bone hook through a stab incision and using the instrument to securely maintain reduction while pinning the fracture site. While maintaining secure bone-to-bone contact, authors inserted the wire into the metacarpal bone from cortex to cortex under fluoroscopy guidance, thereby eliminating unwarranted interference with the joint movement and thus enabling limited but early mobilization.
Both groups showed comparable clinical outcomes regarding post-reduction x-ray evaluation and range of motion recovery. There was no significant difference in range of motion six months after the surgery between two groups, as all the patients regained full motion recovery. Authors also evaluated the degree of range of motion two months after the surgery to compare recovery speed, which also did not show significant difference between two groups. One of the notable advantages of this proposed technique is the reduction of operation time. Although not included in this study, authors feel that operating time was well comparably reduced to that of closed reduction and K-wire fixation, which is the most frequently applied technique in treating stable fractures. Also, this method showed superior outcome regarding postoperative pain, as soft tissue injury following dissection is minimal. Furthermore, there was one case in the ORIF group that developed adhesion which required surgical release, whereas no adhesion was noted in the mini-open reduction group. Although this does not have any statistical significance, it can be assumed that such mini-open reduction should carry much lower risk of developing postsurgical adhesion compared with the open reduction technique, as the former requires much less incision and dissection than the latter. As for complications, both groups had acceptable outcomes as only a few patients developed minor acute wound-related problems. Another advantage is the reduction of postoperative scar, which was nearly unnoticeable compared with that of conventional dorsal incision in the open reduction group. Patient satisfaction regarding scar quality was significantly higher, making it an aesthetically tolerable technique that may be applied to socially active patients, as well as young female patients.
Although not included in this study, authors assume that this technique may prevent many complications that arise from open reduction method, such as contracture, extension lag, tendon rupture due to fixating material, or plate prominence1516, which are all consequences of wide dissection required for open reduction method, while maintaining the fixation until bony union, especially in the case of unfavorable fracture. Also, it may minimize secondary procedures compared with open reduction method, as 25% of patients treated with open reduction are reported to undergo removal procedures due to plate-related complications15. Furthermore, for patients who feel uncomfortable having titanium plates remained in their body after ORIF, or for those that need to undergo specific imaging studies such as magnetic resonance imaging in the future, mini-open reduction may be an attractive alternative. This technique is relatively easy to perform and does not require extensive surgical expertise, although care must be taken not to injure the extensor digitorum tendons and associated structures, as the visual field obtained through the stab incision can be seemingly limited. Also, the surgeon can simply extend the stab incision intraoperatively to switch to ORIF in case complete reduction seems unlikely due to soft tissue impingement in the fracture site, or in case multiple, severe fractures not previously detected in preoperative images are diagnosed during the surgery. Finally, it puts significantly less financial burden on patients compared with open reduction using plate and screws.
Admittedly, the technique presented in this study has several potential drawbacks. Our technique cannot replace the traditional open reduction and plate fixation in case of multiple, comminuted fracture that requires rigid fixation. This type of fracture is likely to require planning of traditional open reduction techniques or external fixation. Also, it still accompanies low risk of inflicting injury to vessels or nerves adjacent to the incision site, especially in case of an untrained surgeon. All such drawbacks must therefore be taken into account before execution.
The restricted number of cases, along with the fact that the study was conducted by a single surgeon, places limitations to this study. A more reliable result may be achieved by both increasing the number of subjects and minimizing the surgeon's bias. Also, authors excluded first metacarpal bone fractures from the study, since first metacarpal bones have unique anatomical structure and location different from those of other metacarpal bones, and thus would be difficult to assess its range of motion in the similar context to the rest of the metacarpal bones. Finally, authors mainly focused on comparing with ORIF in treating unstable fractures; however, additional studies that compare with closed reduction and K-wire fixation, yet another widely performed technique in treating metacarpal fractures, need to be conducted as well.
To our knowledge, no randomized or non-randomized studies comparing ORIF with K-wire fixation have been reported, and this is the first comparative study for K-wire fixation with ORIF in metacarpal fractures. By retaining the ability of ORIF to achieve complete reduction and yet minimizing downsides such as soft tissue adhesion and scarring, authors were able to produce satisfactory outcomes, and thus propose this method as an alternative to ORIF in treating most metacarpal fractures excluding intra-articular fractures.
Figures and Tables
Fig. 1
Depending on the severity of the fracture, a 4 to 6-hole plate along with 8 to 12 mm screws were used for bicortical plate fixation.

Fig. 3
The fractured segment was then reduced to appropriate position through simultaneous distal traction of the involved finger and direct palpation using the elevator.

Fig. 4
After comfirmed reduction and alignment, authors further advanced the initially inserted K-wire to reach the opposite side of the metacarpal base.

Fig. 5
In patients with unfavorable fractures, K-wires are inserted transverse direction while maintaining the reduction with Freer elevator.

References
1. Chung KC, Spilson SV. The frequency and epidemiology of hand and forearm fractures in the United States. J Hand Surg Am. 2001; 26:908–915.

2. Feehan LM, Sheps SB. Incidence and demographics of hand fractures in British Columbia, Canada: a populationbased study. J Hand Surg Am. 2006; 31:1068–1074.

3. Ben-Amotz O, Sammer DM. Practical management of metacarpal fractures. Plast Reconstr Surg. 2015; 136:370e–379e.

4. Henry MH. Fractures of the proximal phalanx and metacarpals in the hand: preferred methods of stabilization. J Am Acad Orthop Surg. 2008; 16:586–595.

5. Diaz-Garcia R, Waljee JF. Current management of metacarpal fractures. Hand Clin. 2013; 29:507–518.

6. Freeland AE, Lindley SG. Malunions of the finger metacarpals and phalanges. Hand Clin. 2006; 22:341–355.

7. Low CK, Wong HC, Low YP, Wong HP. A cadaver study of the effects of dorsal angulation and shortening of the metacarpal shaft on the extension and flexion force ratios of the index and little fingers. J Hand Surg Br. 1995; 20:609–613.

8. Friedrich JB, Vedder NB. An evidence-based approach to metacarpal fractures. Plast Reconstr Surg. 2010; 126:2205–2209.

9. Bloom JM, Hammert WC. Evidence-based medicine: metacarpal fractures. Plast Reconstr Surg. 2014; 133:1252–1260.
10. Ozer K, Gillani S, Williams A, Peterson SL, Morgan S. Comparison of intramedullary nailing versus plate-screw fixation of extra-articular metacarpal fractures. J Hand Surg Am. 2008; 33:1724–1731.

11. Mumtaz MU, Farooq MA, Rasool AA, Kawoosa AA, Badoo AR, Dhar SA. Unstable metacarpal and phalangeal fractures: treatment by internal fixation using AO minifragment plates and screws. Ulus Travma Acil Cerrahi Derg. 2010; 16:334–338.
12. Greeven AP, Bezstarosti S, Krijnen P, Schipper IB. Open reduction and internal fixation versus percutaneous transverse Kirschner wire fixation for single, closed second to fifth metacarpal shaft fractures: a systematic review. Eur J Trauma Emerg Surg. 2016; 42:169–175.

13. Facca S, Ramdhian R, Pelissier A, Diaconu M, Liverneaux P. Fifth metacarpal neck fracture fixation: Locking plate versus K-wire? Orthop Traumatol Surg Res. 2010; 96:506–512.

14. Dabezies EJ, Schutte JP. Fixation of metacarpal and phalangeal fractures with miniature plates and screws. J Hand Surg Am. 1986; 11:283–288.





 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download