Abstract
Background and Purpose
The cerebrospinal fluid (CSF) biomarkers play an important supportive role as diagnostic and predictive indicators of Alzheimer's disease (AD). About 30% of controls in old age show abnormal values of CSF biomarkers and display a higher risk for AD compared with those showing normal values. The cut-off values are determined by their diagnostic accuracy. However, the current cut-off values may be less accurate, because controls include high-risk groups of AD. We sought to develop models of patients with AD, who are homogenous for CSF biomarkers.
Methods
We included participants who had CSF biomarker data in the Alzheimer's Disease Neuroimaging Initiative database. We investigated the factors related to CSF biomarkers in patients with AD using linear mixed models. Using the factors, we developed models corresponding to CSF biomarkers to classify patients with mild cognitive impairment (MCI) into high risk and low risk and analyzed the conversion from MCI to AD using the Cox proportional hazards model.
Results
APOE ε4 status and age were significantly related to CSF Aβ1-42. CSF t-tau, APOE ε2 status and sex were significant factors. The CSF p-tau181 was associated with age and frequency of diagnosis. Accordingly, we modeled the three CSF biomarkers of AD. In MCI without APOE ε4, our models were better predictors of conversion.
Alzheimer's disease (AD) is the most common cause of dementia. In the current clinical setting, AD is diagnosed by clinical criteria proposed by McKann et al.1 Development of disease modifying drugs requires accurate diagnostic tools. The crerbrospinal fluid (CSF) amyloid beta (Aβ1-42), total tau (t-tau), and phosphorylated tau (p-tau181) are promising diagnostic biomarkers.2 They are correlated with the pathogenesis of AD. CSF biomarkers are not only an important diagnostic tool for AD, but also an important prognostic indicator of the disease decades before its onset.23
Because the concentrations of CSF biomarkers are continuous values, arbitrary cut-off values should be determined for easy diagnosis. For example, AlzBio3 immunoassay kit (Innogenetics, Ghent, Belgium) is one of the most popular kits for CSF protein assay.4 The cut-off points include: Aβ1-42<192 pg/mL, t-tau>93 pg/mL, p-tau181>23 pg/mL, t-tau/Aβ1-42>0.39, or p-tau181/Aβ1-42>0.1 for the diagnosis for AD.2 Although the cut-off points were determined after considering the diagnostic accuracy, the values of patients and controls are centered around the cut-off points. In addition, the CSF biomarkers of controls who represent a high-risk group show an AD signature pattern. Therefore, we need to determine other ways to define the cut-off values for the CSF biomarkers.
The results of CSF biomarkers in AD are homogenous compared with those of the controls.5 In this study, we determined the factors associated with CSF biomarkers in AD. We then defined new cut-off values using appropriate models based on those factors.
We included subjects who had data involving CSF Aβ1-42, t-tau, or p-tau181 in the Alzheimer's Disease Neuroimaging Initiative (ADNI) database. The participants included 631 patients with amnestic mild cognitive impairment (aMCI) and 234 patients with AD whose diagnoses were determined at baseline. Among patients with AD, a patient who reverted to aMCI during a follow-up visit was excluded. The participants' ages ranged between 55 and 90 years (inclusive), good overall health to be included in the study. Other inclusion criteria were: treatment with medications stably for 4 weeks, appropriate visual and auditory acuity for neuropsychological testing, and scores on modified Hachinski scales ≤4 and geriatric depression scales <6.78 The patients with aMCI met the criteria proposed by Petersen et al.9 They had abnormal memory function which was tested by delayed paragraph recall of logical memory II. In addition, their Mini-Mental State Examination (MMSE) scores were 24–30 with a memory Clinical Dementia Rating (CDR) score of at least 0.5. Patients with AD met the ‘probable’ criteria of the National Institute of Neurological and Communicative Disorders and Stroke and the Alzheimer's Disease and Related Disorders Association.1 The ADNI includes patients with early stages of AD and MMSE scores of 20–26 and a sum-of-box CDR of 1–9 at their baseline visits. The exclusion criteria were: absence of other neurologic diseases such as Parkinson's disease, multi-infarct dementia, brain tumor, Huntington's disease, normal pressure hydrocephalus, brain tumor, progressive supranuclear palsy, seizure disorder, subdural hematoma, multiple sclerosis, or history of significant head trauma followed by persistent neurologic defaults or known structural brain abnormalities. Participants did not have major depression or bipolar disorder within the past 1 year, or alcohol/drug abuse within the past two years. They had no history of schizophrenia. Subjects who were contraindicated for MRI due to the presence of aneurysmal clips or pacemakers were excluded. We downloaded ADNI data on June 2014. The characteristics of people with normal cognition, aMCI and patients with AD including age, sex, years of education, APOE ε2 status, and APOE ε4 status are summarized in Table 1.
All subjects underwent neurological examination, physical examination, and neuropsychological assessments at baseline. Furthermore, CSF and blood samples were drawn, and MRI and FDG-PET scans were obtained. The protocols for cognitive testing, CSF, MRI, and PET are described in detail at http://adni.loni.usc.edu/. The follow-up interval was 6–12 months. In the present study we used results from the baseline and longitudinal results of CSF Aβ1-42, t-tau, or p-tau181.
The patients underwent lumbar puncture (LP) in the morning after overnight fast.211 LP was carried out after MRI and before PET scan. If the test sequences of MRI and PET scan were reversed with LP, at least a three-day window was required between MRI and LPs, and at least a 12-hour window between PET scan and LPs. The patients repeated LPs annually. The “Run” means the test run which was assayed with the same kit and batch at the same time.
CSF Aβ1-42, t-tau, or p-tau181 were assessed using the multiplex xMAP Luminex platform (Luminex Corp., Austin, TX, USA) and Innogenetics/Fujirebio AlzBio3 immunoassay kits (Innogenetics).4
First, we developed mixed models with a random intercept and random slope, using age, sex, time from baseline, APOE ε2 alleles, and APOE ε4 alleles as fixed effects and run as a random effect. We used the compound symmetric as the covariate matrix. We also tested other covariate matrices, without any differences with the compound symmetric. The purpose of the first analysis was to identify the biological factors affecting the concentrations of CSF Aβ1-42, t-tau, or p-tau181 in AD. The allele number of APOE ε2 homozygote was regarded as 1, because APOE ε2 homozygotes were few. We arbitrarily selected the factors with p≤0.10 and used them in the final fitting models. In addition, we monitored the interactions among the significant factors. In the event of significant interactions among factors, we created fitting models by stratifications. We defined the upper 95% confidence interval curve for Aβ1-42, the lower curve for t-tau, or p-tau181 as new cut-off lines.
We compared MCI conversion to AD between old and new cut-off values using Cox proportional hazards model. The time variables included years from baseline visit to follow-up visit at the time of conversion.
The statistical analyses were conducted using PASW (version 21.0; IBM Corp., Armonk, NY, USA). Graphical presentations were performed using R (version 3.0.1).
Table 2 displays the selection of the factors affecting CSF biomarker concentrations of patients with AD, using the mixed models. We selected factors with p≤0.10 and determined the interaction between the factors. Based on significant interactions, we separated factors to create a fitting model. We selected APOE ε4 status (p<0.001) and age (p=0.10) as the factors significantly related with CSF Aβ1-42. For CSF t-tau, APOE ε2 status (p=0.009) and sex (p<0.001) were significant factors. Age (p=0.005) and time from diagnosis (p=0.004) were the significant factors for CSF p-tau181. We identified interactions between CSF Aβ1-42 related factors (APOE ε4 status and age, p=0.020) and between t-tau related factors (APOE ε2 status and sex, p=0.034).
As shown in Fig. 1, the distribution of CSF Aβ1-42 according to the number of APOE ε4 varies with respect to age. In the absence of APOE ε4, a linear increase was observed in age. In APOE ε4 heterozygotes, a parabolic shape with apex at about 67 was observed. In APOE ε4 homozygotes, the CSF Aβ1-42 decreased linearly with respect to age. The CSF t-tau is related to gender by APOE ε2 (Fig. 2). The distribution of CSF p-tau181 decreased linearly with age at baseline visit (Fig. 3).
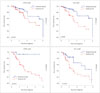
We assumed that the conversion to AD may be predicted accurately in patients with MCI using the new models. To test this hypothesis, the CSF results of MCI, based on age, sex, APOE ε2, and APOE ε4 were used to distinguish the normal/abnormal conditions as shown in Fig. 4. As shown in Fig. 5, in MCI without APOE ε4, our cut-off methods showed lower false positives in the predicted normal group and lower false negatives in the predicted AD group (Fig. 5). However, in MCI with APOE ε4 heterozygotes, our cut-off methods produced higher false negative rate in the predicted normal group. In APOE ε4 homozygotes, it played no role in predicting the conversion, because APOE ε4 homozygote itself was a significant predictor of disease.
In our study, we considered only patients with AD for the determination of the cut-off values for the CSF biomarkers. In addition, conversion from MCI to AD can be more accurately predicted by considering age, sex, APOE ε2, and APOE ε4 status. The new cut-off methods were particularly accurate for subjects without APOE ε4.
Our study provided insight into the role of CSF biomarkers by plotting their concentrations according to the related factors. The interaction between age and APOE ε4 affected the concentrations of CSF Aβ1-42, and therefore, age and the APOE ε4 status were analyzed separately (Fig. 1). In the APOE ε4 non-carriers, the concentration of CSF Aβ1-42 was correlated linearly with age, although it showed a negative quadratic curve according to age in the APOE ε4 heterozygotes. In the APOE ε4 homozygotes, it was reduced to a negative correlation depending on age. Interestingly, the t-tau levels varied between patients with and without APOE ε2 (Fig. 2). The levels of t-tau also differed according to sex. The CSF p-tau181 concentration was decreased according to age.
Our cut-off methods were accurate predictors of conversions particularly in MCI without APOE ε4 (Fig. 5). Introduction of preventive medicines may decrease the cost of our methods by decreasing falsely classified MCI with AD signatures. In addition, it increases the effectiveness of preventive medicines by decreasing the falsely classified MCI without AD signatures. However, our methods may decrease the specificity for MCI with APOE ε4.
Age was an important factor associated with CSF Aβ1-42 in AD without APOE ε4 and with p-tau181. The older patients with AD show mixed pathologies of subcortical vascular dementia, hippocampal sclerosis, argyrophilic grain disease, and suspected non-amyloid pathology.121314 The additional pathologies can cause dementia in patients with less severe amyloid or tau burden in their brain. However, further studies are required to elucidate the role of gender in CSF t-tau. In addition, the further studies are needed to account for the age-related changes in CSF Aβ1-42 found in the APOE ε4 heterozygotes, because of the lower number of patients in young (<70) and old (>80) groups compared with the 70–80 year age group.
We found two noble points. First, we found factors that affect CSF biomarkers in patients with AD. Recently, Li et al.15 and Lautner et al.16 reported that age, sex, and APOE ε4 are factors that affect CSF Aβ1-42 in subjects with normal cognition. These two studies overlooked that the CSF biomarkers in subjects with normal cognition showed average results for two completely different groups–high risk and low risk groups for AD. The proportion of high risk patients for AD increased with age in subjects with normal cognition. Second, we have redefined the cut-off methods of CSF biomarkers using factors that affect CSF biomarkers. In this study, we indicated that the current cut-off values for APOE ε4 noncarrier was less specific and resulted in several false negatives.
In conclusion, we established better cut-off values of CSF biomarkers, which were made only from patients with AD, and not from controls. In addition, age, sex, and APOE genotype play a key role in the interpretation of the cut-off values of CSF biomarkers.
Figures and Tables
Fig. 1
Correlation of CSF Aβ1-42 with age and APOE ε4 status in Alzheimer's disease. The blue lines represent the fitting models for concentration of CSF Aβ1-42 and the surrounding gray zones denote 95% confidence intervals. The horizontal red dotted line is a cut-off values that distinguishes normality and abnormality as determined by a previous study. CSF: cerebrospinal fluid.

Fig. 2
The concentration of cerebrospinal fluid t-tau according to sex and APOE ε2 status in Alzheimer's disease. The horizontal bars are zones of mean±standard deviation.

Fig. 4
Classification of patients with MCI based on the new cut-off lines of CSF biomarkers. The converters with high CSF tau (dark triangle) above upper 95% CI line (MCI with abnormalities in Aβ1-42, t-tau, and p-tau181) represent false negatives. The cut-off lines of Aβ1-42 represent the upper 95% CI lines in Fig. 1. The cut-off lines of t-tau and p-tau181 are the lower 95% CI lines of Figs. 2 and 3, respectively. Patients who showed the low tau (black circles) may have non-Alzheimer's disease dementia. CI: confidence interval, CSF: cerebrospinal fluid, MCI: mild cognitive impairment.

Fig. 5
Kaplan-Meier curves comparing conversion from MCI to dementia using existing/new diagnostic methods. p was obtained by the Cox proportional hazards model adjusting for age, gender, education years, and clinical dementia rating sum of box. The left column represents the results of current diagnostic methods, and the right column displays results of new diagnostic methods. The upper panels show results for MCI without APOE ε4, and the lower panels displays results of MCI with APOE ε4 heterozygotes. AD: Alzheimer's disease, ADNI: Alzheimer's Disease Neuroimaging Initiative, MCI: mild cognitive impairment.
Acknowledgements
This study was supported by intramural funds from Ilsan Hospital, National Health Insurance Service and by grants from the Original Technology Research Program for Brain Science through the National Research Foundation of Korea funded by the Korean Government (MSIP; No. 2014 M3C7A1064752).
The data used in preparation of this article were obtained from the Alzheimer's Disease Neuroimaging Initiative (ADNI) database (adni.loni.ucla.edu). As such, the investigators within the ADNI contributed to the design and implementation of ADNI and/or provided data but did not participate in analysis or writing of this report. A complete listing of ADNI investigators can be found at: http://adni.loni.ucla.edu/wp-content/uploads/how_to_apply/ADNI_Acknowledgement_List.pdf.
References
1. McKhann G, Drachman D, Folstein M, Katzman R, Price D, Stadlan EM. Clinical diagnosis of Alzheimer's disease: report of the NINCDS-ADRDA Work Group under the auspices of Department of Health and Human Services Task Force on Alzheimer's Disease. Neurology. 1984; 34:939–944.

2. Shaw LM, Vanderstichele H, Knapik-Czajka M, Clark CM, Aisen PS, Petersen RC, et al. Cerebrospinal fluid biomarker signature in Alzheimer's disease neuroimaging initiative subjects. Ann Neurol. 2009; 65:403–413.

3. Walhovd KB, Fjell AM, Brewer J, McEvoy LK, Fennema-Notestine C, Hagler DJ Jr, et al. Combining MR imaging, positron-emission tomography, and CSF biomarkers in the diagnosis and prognosis of Alzheimer disease. AJNR Am J Neuroradiol. 2010; 31:347–354.

4. Olsson A, Vanderstichele H, Andreasen N, De Meyer G, Wallin A, Holmberg B, et al. Simultaneous measurement of beta-amyloid (1-42), total tau, and phosphorylated tau (Thr181) in cerebrospinal fluid by the xMAP technology. Clin Chem. 2005; 51:336–345.

5. Shin S, Kim JH, Cho JH, Kim GS, Choi SA, Lee JH. Alzheimer's Disease Neuroimaging Initiative. Mild cognitive impairment due to Alzheimer disease is less likely under the age of 65. Alzheimer Dis Assoc Disord. 2015; 29:26–31.

6. Nettiksimmons J, Harvey D, Brewer J, Carmichael O, DeCarli C, Jack CR Jr, et al. Subtypes based on cerebrospinal fluid and magnetic resonance imaging markers in normal elderly predict cognitive decline. Neurobiol Aging. 2010; 31:1419–1428.

7. Hachinski VC, Iliff LD, Zilhka E, Du Boulay GH, McAllister VL, Marshall J, et al. Cerebral blood flow in dementia. Arch Neurol. 1975; 32:632–637.

8. Sheikh JI, Yesavage JA. Geriatric Depression Scale (GDS): recent evidence and development of a shorter version. In : Brink TL, editor. Clinical Gerontology: A Guide to Assessment and Intervention. New York: The Haworth Press;1986. p. 165–174.
9. Petersen RC, Smith GE, Waring SC, Ivnik RJ, Tangalos EG, Kokmen E. Mild cognitive impairment: clinical characterization and outcome. Arch Neurol. 1999; 56:303–308.
10. Bertens D, Knol DL, Scheltens P, Visser PJ. Alzheimer's Disease Neuroimaging Initiative. Temporal evolution of biomarkers and cognitive markers in the asymptomatic, MCI, and dementia stage of Alzheimer's disease. Alzheimers Dement. 2015; 11:511–522.

11. Shaw LM, Vanderstichele H, Knapik-Czajka M, Figurski M, Coart E, Blennow K, et al. Qualification of the analytical and clinical performance of CSF biomarker analyses in ADNI. Acta Neuropathol. 2011; 121:597–609.

12. Savva GM, Wharton SB, Ince PG, Forster G, Matthews FE, Brayne C. Medical Research Council Cognitive Function and Ageing Study. Age, neuropathology, and dementia. N Engl J Med. 2009; 360:2302–2309.

14. Caroli A, Prestia A, Galluzzi S, Ferrari C, van der Flier WM, Ossenkoppele R, et al. Mild cognitive impairment with suspected nonamyloid pathology (SNAP): Prediction of progression. Neurology. 2015; 84:508–515.





 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download