Abstract
Purpose
To analyze the clinical result of a conventional reconstruction plate (CRP) fixation and locking compressive plate (LCP) fixation on the surgical treatment of an adult's displaced intercondylar fracture of humerus.
Materials and Methods
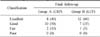
A total of 40 patients enrolled in the study were treated between August 2002 and May 2012. Fixation with a CRP was performed in 20 patients (group A) and anatomical locking compression plate fixation was performed in 20 patients (group B). The clinical and functional evaluation was performed according to the Mayo elbow performance score and Cassebaum classification of elbow range of motion (ROM), disabilities of the arm, shoulder and hand score.
Results
The Mayo elbow functional evaluation scores, eight cases were excellent, 10 cases were good, and two cases were fair in group A, and 12 cases were excellent, seven cases good, and one case fair in group B; both groups showed satisfactory results. The durations of attaining 90 to 120 degrees of the ROM of joints postoperatively were 8.3 days on average (6 to 15 days) in group A and 5.5 days on average (5 to 9 days) in group B, demonstrating a significant difference between the two groups (p=0.04). Although the correlations of clinical results according to the difference of bone mineral densities (BMDs) were not statistically significant between the two groups (p=0.35), loss of fixation occurred due to loosening of screws in two patients with low BMDs in whose operations reconstruction plates were used.
Figures and Tables
Fig. 1
One case from group A. (A) Initial radiographs show AO/ASIF type C2 fracture of the distal humerus. (B) Postoperative radiographs show a bilateral reconstruction plate through chevron osteotomy of olecranon. (C) At postoperative one year, the patient has excellent range of motion of the elbow from 0° to 150°.

Fig. 2
One case from group B. (A) Initial radiographs show AO/ASIF type C2 fracture of the distal humerus. (B) Postoperative radiographs show a bilateral locking compression plate through chevron osteotomy of olecranon. (C) At postoperative one year, the patient has excellent range of motion of the elbow from 0° to 135°.

Fig. 3
Follow-up radiographs show screw loosening of the lateral reconstruction plate in a patient with low bone mineral densities in whose operations reconstruction plates were used.

References
1. Helfet DL, Schmeling GJ. Bicondylar intraarticular fractures of the distal humerus in adults. Clin Orthop Relat Res. 1993; (292):26–36.

2. Henley MB. Intra-articular distal humeral fractures in adults. Orthop Clin North Am. 1987; 18:11–23.

3. Kang CN, Wang JM, Roh KJ, Yun YH, Cho DY. Multiple K Wires fixation of the intercondylar fracture of humerus in adults. J Korean Soc Fract. 1993; 6:325–330.

4. Papaioannou N, Babis GC, Kalavritinos J, Pantazopoulos T. Operative treatment of type C intra-articular fractures of the distal humerus: the role of stability achieved at surgery on final outcome. Injury. 1995; 26:169–173.

5. Greiner S, Haas NP, Bail HJ. Outcome after open reduction and angular stable internal fixation for supra-intercondylar fractures of the distal humerus: preliminary results with the LCP distal humerus system. Arch Orthop Trauma Surg. 2008; 128:723–729.

7. Jupiter JB. Complex fractures of the distal part of the humerus and associated complications. Instr Course Lect. 1995; 44:187–198.

8. O'Driscoll SW, Jupiter JB, Cohen MS, Ring D, McKee MD. Difficult elbow fractures: pearls and pitfalls. Instr Course Lect. 2003; 52:113–134.
9. Ring D, Gulotta L, Roy A, Jupiter JB. Concomitant nonunion of the distal humerus and olecranon. J South Orthop Assoc. 2003; 12:27–31.
10. Ring D, Jupiter JB. Complex fractures of the distal humerus and their complications. J Shoulder Elbow Surg. 1999; 8:85–97.

11. Schuster I, Korner J, Arzdorf M, Schwieger K, Diederichs G, Linke B. Mechanical comparison in cadaver specimens of three different 90-degree double-plate osteosyntheses for simulated C2-type distal humerus fractures with varying bone densities. J Orthop Trauma. 2008; 22:113–120.

12. Aitken GK, Rorabeck CH. Distal humeral fractures in the adult. Clin Orthop Relat Res. 1986; (207):191–197.

13. Gabel GT, Hanson G, Bennett JB, Noble PC, Tullos HS. Intraarticular fractures of the distal humerus in the adult. Clin Orthop Relat Res. 1987; (216):99–108.

15. Wang KC, Shih HN, Hsu KY, Shih CH. Intercondylar fractures of the distal humerus: routine anterior subcutaneous transposition of the ulnar nerve in a posterior operative approach. J Trauma. 1994; 36:770–773.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download