Abstract
Purpose
To evaluate clinical and radiological outcomes for the comminuted metadiaphyseal fractures of the proximal humerus treated with a separate minimally invasive approach deltopectoral approach for fracture fragment reduction and deltoid splitting approach for cephalo-diaphyseal plate fixation.
Materials and Methods
Eighteen patients (6 men and 12 women), who underwent surgery between March 2007 and February 2011, were included. A deltopectoral approach was used to expose and reduce the fracture fragments and an additional deltoid splitting approach was used to expose the humeral head. A locking plate was inserted under the muscle window and a cephalo-diaphyseal fixation was performed. All patients were examined and interviewed using the Visual Analog Scale (VAS) score, Constant score and standardized X-rays to check the time to fracture healing, neck-shaft angle (NSA).
Results
All fractures were united, and mean healing time was 20 weeks. The average VAS score was 3.5 points (range, 0-5) and the average Constant score was 66.5 points (range, 30-90). Final functional outcomes were four cases of excellent, six cases of good, six cases of fair and two cases of poor. The average NSA was 127.5° (range, 100-140).
Conclusion
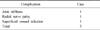
A separate approach and cephalo-diaphyseal plate fixation in operative treatment of the metadiaphyseal fractures of the proximal humerus is an effective, reliable treatment option that could reduce the fracture fragments accurately, with less dissection of the soft tissue and lower the complications. A further study including many cases and longer follow-up will be needed to improve the quality of the study.
Figures and Tables
Fig. 1
(A, B) Preoperative radiographs of 63-year-old woman with comminuted meta-diaphyseal fracture of humerus. Note the long spiral and displacement of the fracture fragments.
(C, D) Radiographs at postoperative 18 months shows good alignment and bone union. Neck-shaft angle (NSA) was 130° and the medial cortex was anatomically reduced.
(E, F) Preoperative radiographs of 55-year-old woman with comminuted meta-diaphyseal fracture of humerus.
(G, H) Radiographs at 12 months show good alignment and bone union. NSA was 130° and the medial cortex was anatomically reduced.

References
1. Acklin YP, Sommer C. Plate fixation of proximal humerus fractures using the minimally invasive anterolateral delta split approach. Oper Orthop Traumatol. 2012. 24:61–73.

2. Agudelo J, Schürmann M, Stahel P, et al. Analysis of efficacy and failure in proximal humerus fractures treated with locking plates. J Orthop Trauma. 2007. 21:676–681.

3. Bae SW, Kim WJ, Song BY, Choi NH, Lee JH. Postoperative functional assessments in adult humerus shaft fractures -comparison among plates and screws, intramedullary nail and external fixator-. J Korean Soc Fract. 2001. 14:228–235.

4. Blum J, Hansen M, Rommens PM. Angle-stable intramedullary nailing of proximal humerus fractures with the PHN (proximal humeral nail). Oper Orthop Traumatol. 2009. 21:296–311.
5. Bono CM, Grossman MG, Hochwald N, Tornetta P 3rd. Radial and axillary nerves. Anatomic considerations for humeral fixation. Clin Orthop Relat Res. 2000. (373):259–264.
6. Gardner MJ, Griffith MH, Dines JS, Lorich DG. A minimally invasive approach for plate fixation of the proximal humerus. Bull Hosp Jt Dis. 2004. 62:18–23.
7. Jiang R, Luo CF, Zeng BF, Mei GH. Minimally invasive plating for complex humeral shaft fractures. Arch Orthop Trauma Surg. 2007. 127:531–535.

8. Kim DW, Kim CK, Jung SW, Kim HS. Operative treatment of displaced proximal humerus fractures with the angular stable locking compression plate. Clin Should Elbow. 2011. 14:27–34.

9. Koch PP, Gross DF, Gerber C. The results of functional (Sarmiento) bracing of humeral shaft fractures. J Shoulder Elbow Surg. 2002. 11:143–150.

10. Laflamme GY, Rouleau DM, Berry GK, Beaumont PH, Reindl R, Harvey EJ. Percutaneous humeral plating of fractures of the proximal humerus: results of a prospective multicenter clinical trial. J Orthop Trauma. 2008. 22:153–158.

11. Lau TW, Leung F, Chan CF, Chow SP. Minimally invasive plate osteosynthesis in the treatment of proximal humeral fracture. Int Orthop. 2007. 31:657–664.

12. Lill H, Hepp P, Rose T, König K, Josten C. The angle stable locking-proximal-humerus-plate (LPHP) for proximal humeral fractures using a small anterior-lateral-deltoid-splitting-approach-technique and first results. Zentralbl Chir. 2004. 129:43–48.
13. Min WK, Sin SJ, Jeon IH, et al. Fixation failure of LCP during the treatment of proximal humerus fractures. J Korean Fract Soc. 2006. 19:188–192.

14. Oh CH, Oh JH, Kim SH, Jo KH, Bin SW, Gong HS. Hemiarthoplasty with bone block graft and low profile prosthesis for the comminuted proximal humerus fractures. J Korean Fract Soc. 2008. 21:213–219.

15. Park CH, Park SH, Seo JS. Internal fixation of proximal humerus fracture with locking compression plate. J Korean Shoulder Elbow Soc. 2009. 12:44–52.

16. Park JY, Oh JH, Kho DH, Jung JK. Intramedullary nail on the humeral fracture. J Korean Fract Soc. 2008. 21:244–254.





 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download