Abstract
Background
Alarm services in the Order Communication System improve awareness for related physicians including orthopaedic surgeons, internal medicine doctors, and other relevent doctors. This prospective observational multicenter study was to compare the diagnostic and treatment rates of osteoporosis between an alarm service group and a no alarm service group.
Methods
From January 2017 to december 2017, The subjects included patients aged 50 years or older with hip fractures from 16 hospital-based multicenter cohorts. Among the 16 hospitals, 5 university hospitals established an alarm service for osteoporosis management (i.e., Alarm group) and 11 university hospitals did not set-up alarm services (i.e., Control group). The rate of dual energy X-ray absorptiometry (DXA) test and the initiation rate of antiosteoporosis medications between the 2 groups were compared at enrollment and at 6 months follow-up.
Results
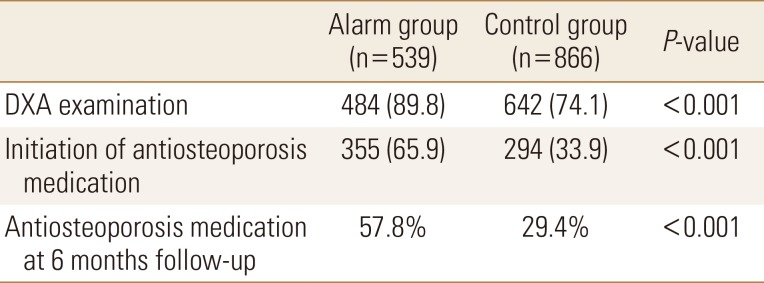
During the study period, 1,405 patients were enrolled. The DXA examination rate and initiation rate of osteoporosis treatment between the Alarm group and the Control group were 484 patients (89.8%) vs. 642 patients (74.1%) (P<0.001) and 355 patients (65.9%) versus 294 patients (33.9%) (P<0.001), respectively. At 6 months follow-up, the rate of anti-osteoporosis management between the 2 groups decreased (57.8% vs. 29.4%).
Conclusions
This prospective multicenter study demonstrates that alarm services can improve awareness of physicians, and it resulted in a significantly higher rate of examination of DXA and initiation of anti-osteoporosis medication in the Alram group. Therefore, alarm service is a simple and effective tool to increase anti-osteoporosis management as part of the fractuure liaison service in South Korea.
Osteoporosis is defined as an illness characterized by decreased bone strength that results in increased risk of fracture.[1] According to reports from the Korea National Health and Nutrition Examination Survey (KNHANES 2008–2009) data, prevalence of osteoporosis in adults aged 50 years or older is 22% (35.5% in women and 7.5% in men) and the rae for treatment was only 12.8% (14.4% in women and 4.0% in men).[2] In addition, only 37% of patients with fragility fractures were prescribed anti-osteoporosis drugs within 6 months post-fracture.[3]
Anti-osteoporosis medications have been shown to prevent fragility osteoporotic fractures not only for patients with osteoporosis but also for patients with previous fragility fractures.[456] To date, numerous studies have repored that anti-osteoporosis medication in patients with osteoporotic fragility fractures reduces the risks of subsequent fragility fractures.[45]
A fracture liaison service (FLS) is a multidisciplinary system approach to reducing subsequent fracture risk in patients with a recent fragility fracture. This service identifies patients at the time that they are treated at the hospital for a fracture and provides them easy access to osteoporosis care.[7]
The FLS program for the prevent of secondary fragility fractures has been operating and has reported successful outcomes in many countries over the last 3 decades.[8] Although many studies have reported cost-effectiveness of the FLS programs,[910] the FLS program in Korea is still young and in the beginning stages. Among several factors in the FLS program, the coordinator-based education is the most important.[1112] However, in Korea, coordinator-based FLS programs are difficult to operate because of reimbursement for education costs by insurance company.
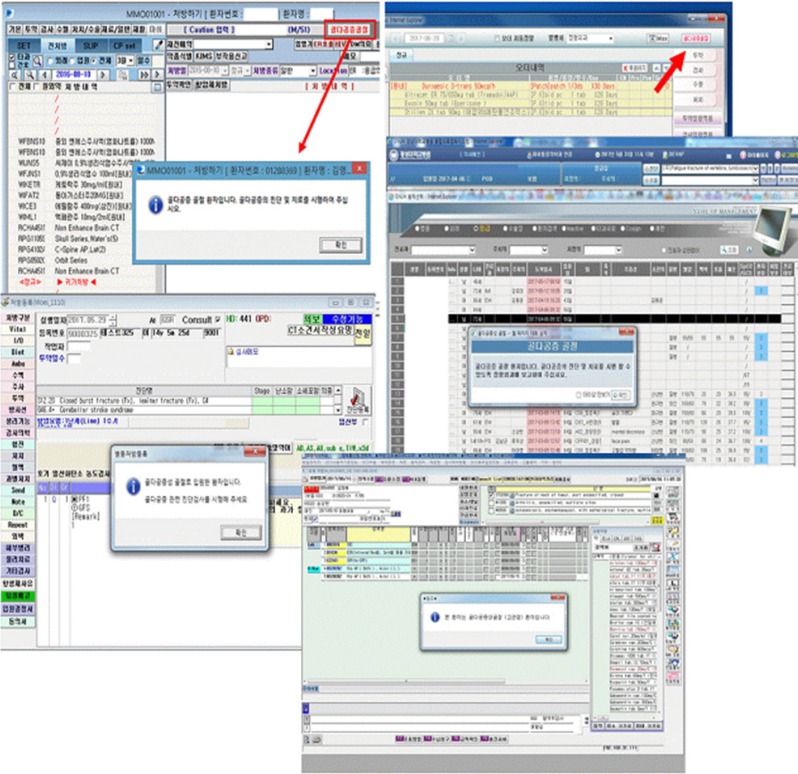
Therefore, an alarm service has been designed in order to improve the use of osteoporosis medication through the hospital's computer system. Alarm services in the Order Communication System (OCS) were included as a necessity of dual energy X-ray absorptiometry (DXA) and anti-osteoporosis medications on the computer monitor when the patient visited the emergency room or an outpatient clinic. Alarm services in the OCS improves awareness for related physicians including orthopaedic surgeons, internal medicine doctors, and other relevant doctors. This prospective observational multicenter study was to compare the diagnostic and treatment rates of osteoporosis between an alarm service group and a no alarm service group.
The design and protocol of this prospective study were approved by the Institutional Review Board at the hospital. All patients were informed that their medical data would be used for scientific study, and written informed consent was obtained from each of the patients.
The subjects of this study were patients aged 50 years or older, included in a hospital based multicenter cohort involving those with hip fractures (including femur neck, intertrochanter, and subtrochanter fractures). The cohort was established in April 2016, when eligible patients had been registered from 16 university hospitals. Data of the patients were collected at the central office using the Korea National Institute of Health web-based system (an Internet-based Clinical Research and Trial Management System (iCreaT, Cheongju, Korea). The inclusion criteria of this study featured the following: (1) patients who sustained hip fractures due to lowenergy trauma [13]; (2) those who were operating with either internal fixation or hemiarthroplasty; and (3) those who were aged 50 years or older at the time of surgery. The exclusion criteria were the following: (1) patients with metabolic bone diseases; (2) those with pathological fractures; and (3) those who suffered atraffic accident or industrial trauma.
The alarm service is a pop-up massage in the OCS of the hospital and was developed tor improve awareness of diagnosis and initiation of treatment for osteoporosis (Fig. 1). These alarm services automatically appear in the OCS when patients with hip fractures aged 50 years or older visited the emergency room or an outpatient clinic. Additionally, this service would appear if the patient qualified for International Classification of Diseases, tenth revision diagnostic codes S72.0 (fracture of the femur neck ) and S72.1 (trochanteric fracture).
The patients were separated into 2 groups. The Alarm group (i.e., treatment) included setting up alarm services in 5 university hospitals and the No Alarm (i.e., control) group involved no alarm services within 11 university hospitals. The rate of DXA and the initiation rate of anti-osteoporosis medications between both groups were compared at enrollment and at 6 months follow-up.
A χ2 test was used to compare the rates of DXA examination, osteoporosis medication, and 30-days mortality between the 2 groups. All analyses were performed using SPSS software (version 20.0; SPSS Inc., Chicago, IL, USA). A P value of less than 0.05 was considered significant.
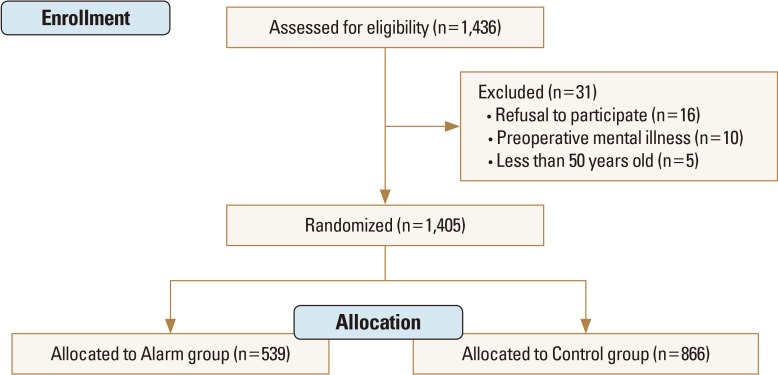
During the study period, 1,436 patients were eligible for the study. Thirty-one patients were excluded: 16 patients refused to participate, 10 patients with mental illness were unable to check DXA, and 5 patients did not meet the age requirement (less than 50 years old). Of the 1,405 patients, 539 patients were assigned to the Alarm group and 866 patients were in the Control group (Fig. 2).
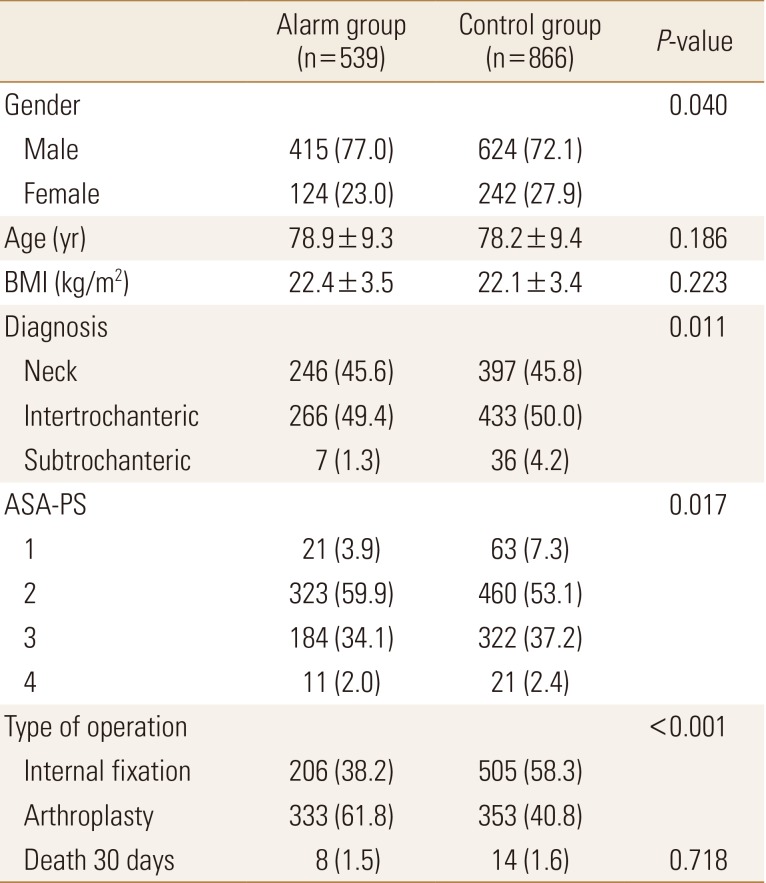
Although age, body mass index, and mortality at 30-days did not differ between the 2 groups, gender (P=0.040), diagnosis (P=0.011), American Society of Anaesthesiologist Physical Status (ASA-PS) (P=0.017), and type of operation (P<0.001) showed a significant difference between the 2 groups (Table 1).
The DXA examination rate and initiation rate of osteoporosis treatment between the Alarm group and the Control group were 484 patients (89.8%) vs. 642 patients (74.1%) (P<0.001) and 355 patients (65.9%) vs. 294 patients (33.9%) (P<0.001), respectively (Table 2). At 6 months follow-up, the rate of anti-osteoporosis management between the 2 groups decreased (57.8% vs. 29.4%; Table 2). Bisphosphonate was prescribed in 447 patients (68.9%), selective estrogen receptor modulator in 131 patients (20.2%), and parathyroid hormone in 71 patients (10.9%). Only 238 patients (36.6%) were prescribed a combinationo fo calcium and vitamin D.
Anti-osteoporosis management is important for FLS programs to prevent subsequent fragility fractures.[9111214] This prospective multicenter observational study dshowed 89.8% and 65.9% of the DXA examination rate and initiation rate of osteoporosis treatment in the Alarm group, which are significantly higher than those in the Control group (74.1% and 33.9%), respectively (P<0.001). At the 6 month follow-up, the rate of anti-osteoporosis management decreased to 57.8% in the Alarm group and 29.4% in the Control group.
Improving physician awareness for osteoporosis treatment is important in order to prevent subsequent fractures. Comparing anti-osteoporosis management in the Control group (33.9%) that in the Alarm goup (65.9%) demonstrated that an alarm service program may be an effective tool for physiciam awareness and may result in an increase anti-osteoporosis management. This finding corresponds with previous studies. Kim et al. [15] examined the effect of pop-up messages (regarding a history of DXA) in the identification and management of soteoporosis in 404 patients with osteoporotic hip or spine fractures, conducting before and after study. They reported that after introducing the pop-up messages, the rate of DXA prescription increased from 35.1% to 57.1% (P<0.001), and the rate of anti-osteoporosis medication increased from 21.1% to 25.2% (P=0.05).[15] Nho et al. [13] performed case control study to determine whether an alarm clock could improve compliance with weekly bisphosphonate in 100 patients with osteoporosis. They reported that the mean medication rates of the Alarm group (0.80±0.33) was higher than that fo the Control group (0.56±0.34) (P<0.001).[13] Therefore, it can be inferred that even though an alarm service is a simple and limited tool, it may be helpful in improving physician and patient awareness. Additionally, findings show an increase in the rate of DXA examniation and an increase in initiation or maintenance of anti-osteoporosis medication.
Although FLS programs in other developed countries are based on coordinator-based system,[616] reimbursement of coordination costs is not possible in South Korea. Due to computerization of hospital systems in South Korea, all hospital and clinics are operating on an electronic chart system, such as OCS. Therefore, an alarm service model developed for increasing anti-osteoporosis medication is one of the important factors of FLS in South Korea. Although the alarm service system in this model was shown to be successful in comparison to the Control group, it might be difficult to generalize and substitute a coordinator for the FLS system. The role of the coordinator is to not only recommend anti-osteoporosis medication, but to also provide education on nutrition, exercise, and other medical problems.
According to the Korean National Health Insurance reimbursement guidelines, bone mineral density was evaluated in cases that might require osteoporosis treatment. This is cause the cost of calcium and vitamin D supplements was reimbursed if the DXA T-score was lower than −1.0, and the cost of osteoporosis medication was reimbursed if the DXA T-score was lower than −2.5.[15] Since May 2015, patients with an osteoporotic fracture received reimbursement for anti-osteoporosis medication for 3 years regardless of T-score.[17] The reimbursement guidelines are possible due to the success of the alarm service program and assure the FLS model in South Korea.
This study has several limitations. First, although this multicenter study was prospectively designed, random assignment and blindness were not possible. In addition, he alarm service was not available in all of the hospitals due to different situations in individual hospitals. Therefore, only 5 hospitals were able to implement an alarm service using OCS. Second, the duration of a 6-month follow-up period might not confirm compliance with anti-osteoporosis medication. However, this alarm service was designed to conform the initiation of DXA examination and anti-osteoporosis medication in patients with hip fractures. Finally, the alarm service model only improved awareness among physicians, but not among patients. Therefore, an education program for patients might be mandatory.
Nevertheless, this prospective multicenter study demonstrates that an alarm service may improve physician awareness and have significantly higher rates for examination of DXA and initiation of anti-osteoporosis medication. Therefore, as a simple and effective tool for increasing anti-osteoporosis management, an alarm service may be part of the FLS in South Korea.
Acknowledgments
This research was supported by a grant of the Korea Health Technology R&D Project through the Korea Health Industry Development Institute (KHIDI), funded by the Ministry of Health & Welfare, Korea (grant number : HC15C1189).
Notes
References
1. NIH Consensus Development Conference. NIH consensus development panel on osteoporosis prevention, diagnosis, and therapy, March 7–29, 2000: highlights of the conference. South Med J. 2001; 94:569–573. PMID: 11440324.
2. Choi YJ, Oh HJ, Kim DJ, et al. The prevalence of osteoporosis in Korean adults aged 50 years or older and the higher diagnosis rates in women who were beneficiaries of a national screening program: the Korea National Health and Nutrition Examination Survey 2008–2009. J Bone Miner Res. 2012; 27:1879–1886. PMID: 22532494.

3. Jung Y, Ko Y, Kim HY, et al. Gender differences in anti-osteoporosis drug treatment after osteoporotic fractures. J Bone Miner Metab. 2019; 37:134–141. PMID: 29536198.

4. Lee YK, Ha YC, Choi HJ, et al. Bisphosphonate use and subsequent hip fracture in South Korea. Osteoporos Int. 2013; 24:2887–2892. PMID: 23681088.

5. Lee YK, Ha YC, Yoon BH, et al. Incidence of second hip fracture and compliant use of bisphosphonate. Osteoporos Int. 2013; 24:2099–2104. PMID: 23247329.

6. Merlijn T, Swart KM, van Schoor NM, et al. The effect of a screening and treatment program for the prevention of fractures in older women: A randomized pragmatic trial. J Bone Miner Res. 2019; 34:1993–2000. PMID: 31220365.

7. Curtis JR, Silverman SL. Commentary: the five Ws of a Fracture Liaison Service: why, who, what, where, and how? In osteoporosis, we reap what we sow. Curr Osteoporos Rep. 2013; 11:365–368. PMID: 24104520.

8. Wu CH, Tu ST, Chang YF, et al. Fracture liaison services improve outcomes of patients with osteoporosis-related fractures: A systematic literature review and meta-analysis. Bone. 2018; 111:92–100. PMID: 29555309.

9. Leal J, Gray AM, Hawley S, et al. Cost-effectiveness of orthogeriatric and fracture liaison service models of care for hip fracture patients: A population-based study. J Bone Miner Res. 2017; 32:203–211. PMID: 27632945.

10. Yong JH, Masucci L, Hoch JS, et al. Cost-effectiveness of a fracture liaison service--a real-world evaluation after 6 years of service provision. Osteoporos Int. 2016; 27:231–240. PMID: 26275439.
11. Chadha M, Shingare A, Prasanth A, et al. Fracture liaison service: Prevention by coordination. Indian J Endocrinol Metab. 2018; 22:719–721. PMID: 30766806.

12. Bogoch ER, Elliot-Gibson V, Beaton D, et al. Fracture prevention in the orthopaedic environment: Outcomes of a coordinator-based fracture liaison service. J Bone Joint Surg Am. 2017; 99:820–831. PMID: 28509822.

13. Nho JH, Lee YK, Ha YC, et al. Can alarming improve compliance with weekly bisphosphonate in patients with osteoporosis? J Bone Metab. 2016; 23:51–54. PMID: 27294076.

14. Mugnier B, Daumas A, Couderc AL, et al. Clinical effectiveness of osteoporosis treatment in older patients: A fracture liaison service-based prospective study. J Women Aging. 2019; 31:553–565. PMID: 30295566.

15. Kim JY, Yoo JH, Kim JW, et al. Pop-up messages in order communication systems can increase awareness of osteoporosis among physicians and improve osteoporosis treatment. J Eval Clin Pract. 2016; 22:887–891. PMID: 27151774.

16. Judge A, Javaid MK, Leal J, et al. Models of care for the delivery of secondary fracture prevention after hip fracture: a health service cost,clinical outcomes and cost-effectiveness study within a region of England. Health Serv Deliv Res. 2016; DOI: 10.3310/hsdr04280.
17. Yoo JH, Moon SH, Ha YC, et al. Osteoporotic fracture: 2015 Position statement of the Korean society for bone and mineral research. J Bone Metab. 2015; 22:175–181. PMID: 26713308.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download