INTRODUCTION
Osteoporosis is a common disease characterized by low bone mass and defects in the microarchitecture of bone tissue, which impair bone strength and lead to an increased risk of osteoporotic fractures.[
1] Bone mineral density (BMD), measured by dual energy X-ray absorptiometry (DXA), is often employed to diagnose osteoporosis because bone mass accounts for approximately 70% of bone strength.[
1] Osteoporotic fractures are one of the leading causes of significant morbidity and disability among elderly people and place a substantial economic burden on health care systems.[
2]
BMD is a highly heritable trait, with a heritability ranging between 0.5 and 0.8.[
3] Osteoporotic fracture, as an end-point clinical outcome of osteoporosis, has moderate heritability, of approximately 0.5 to 0.7.[
3] Most other risk factors for osteoporotic fractures such as bone quality (bone loss, ultrasound properties, bone turnover markers, and bone geometry), and non-skeletal factors (cognition and neuromuscular functions), are also moderately heritable traits.[
4] Over the past 6 years, genome-wide association studies (GWASs) and their meta-analyses, assaying hundreds of thousands of single nucleotide polymorphisms (SNPs) in thousands of individuals, have identified over 60 genes/loci associated with variants in BMD and more than 20 genes/loci associated with the risk of osteoporotic fractures. Most GWAS have reported osteoporosis-related variants in Caucasian populations. It is estimated that by 2050, 52% of all hip fractures will occur in Asia, a projected increase from 1990, when 26% of fractures occurred in Asia.[
5] However, there are few studies replicating these variants in East Asian populations. A recent study, the largest GWAS meta-analysis to date in the bone field and the second meta-analysis published by the Genetic Factors of Osteoporosis (GEFOS) consortium—(GEFOS-2)—included 32,961 individuals in the discovery stage and was replicated in 50,933 independent subjects.[
6] In the discovery stage, most of the data were obtained from Caucasian populations, except for one study from Hong Kong with a sample size of 800.[
6] There are ethnic differences resulting from variations in the underlying linkage disequilibrium (LD) structures and in the allele frequencies between Caucasian and East Asian populations.[
7] Because these ethnic differences may also influence the results of association studies, it would be interesting to perform genetic susceptibility studies in East Asian populations.[
8] In this study, we investigated the association between osteoporosis-related traits (BMD, osteoporosis, or fracture) and BMD-related variants previously reported at the discovery stage in GEFOS-2, in the Korean population. We also investigated the association between osteoporosis-related traits and the variants identified in the Korean cohort, and replicated these variants in other East Asian ethnic cohorts (Chinese and Japanese).
RESULTS
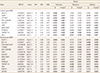
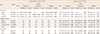
Table 1 shows the baseline characteristics in the study population. Chinese BMD cohorts were younger than the other cohorts were. Non-vertebral fractures in Chinese and Japanese subjects only included hip fractures. Only LS BMD was measured in Japanese subjects.
First, we investigated the association between osteoporosis-related traits (BMD, osteoporosis, or fracture) and 95 SNPs in the Korean cohort (
Tables 2,
3). A total of 17 SNPs from 17 loci were associated with low BMD (β=−0.008 to −0.174,
P=0.001 to 0.048) (
Table 2) in Korean subjects. A total of 9 SNPs from 9 loci were associated with osteoporosis (odd ratios [ORs] 1.20-2.20, 95% confidence intervals [CIs] 1.00–4.64,
P=0.012–0.049] (
Table 3). A total of 6 SNPs from 6 loci were associated with the presence of non-vertebral fractures (ORs 1.40–4.14, 95% CIs 1.00–13.33,
P=0.008–0.048) (
Table 3). A total of 9 SNPs from 9 loci were associated with the presence of vertebral fractures (ORs 1.33–9.98, 95% CIs 1.02–34.96,
P<0.001–0.040) (
Table 3). A total of 5 SNPs from 5 loci were associated with the presence of any fracture (ORs 1.28-8.67, 95% CIs 1.00-29.03,
P<0.001-0.049) (
Table 3). Collectively, 35 out of the 95 SNPs (36.8%) were associated with one or more osteoporosis-related traits in Korean subjects.
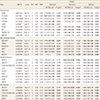
Second, we investigated the association between osteoporosis-related traits and 35 variants in the other East Asian ethnic cohorts, the Chinese and Japanese cohorts (
Tables 4,
5). A total of 12 SNPs from 12 loci were associated with low BMD (β=−0.009 to −0.041,
P=0.002–0.049) (
Table 4) in Chinese and Japanese subjects. A total of 3 SNPs from 3 loci were associated with hip fractures (ORs 1.26–1.78, 95% CIs 1.02–2.70,
P=0.006–0.036) (
Table 5). A total of 4 SNPs from 4 loci were associated with the presence vertebral fractures (ORs 1.44–2.10, 95% CIs 1.01–4.27,
P=0.019–0.043) (
Table 5). A total of 2 SNPs from 2 loci were associated with the presence of any fracture (ORs 1.30–2.37, 95% CIs 1.01–4.99,
P=0.020–0.044) (
Table 5). Finally, 19 SNPs (54.3%) out of 35 SNPs were associated with one or more osteoporosis-related traits in East Asian ethnic populations.
DISCUSSION
In the present study, 35 out of the 95 SNPs (36.8%), previously identified in largely Caucasian populations, were associated with one or more osteoporosis-related traits in Korean subjects. Furthermore, 19 out of the 35 SNPs (54.3%) were also associated with one or more osteoporosis-related traits in the 4,414 East Asian ethnic populations (Chinese, Japanese, and Korean, combined). Therefore, these 19 SNPs were common variants of osteoporosis-related traits in both Caucasian and East Asian populations.
Among Korean subjects, 35 SNPs from 34 loci were associated with one or more osteoporosis-related traits. Some of these genes are known to play a critical role in several biological pathways influencing osteoporosis and fracture susceptibility. First, some genes including
AXIN1,
CTNNB1,
DKK1,
LRP5,
WLS,
WNT4,
WNT5B, and
WNT16, participated in the Wnt/β-catenin signaling pathway. Second,
SOX9 and
SP7 were involved in mesenchymal stem cell differentiation and endochondral ossification. Third,
CLCN7 and
LRP5 were associated with rare monogenic forms of osteoporosis and/ or high bone mass. Finally,
TNFRSF11A (encoding the receptor activator of nuclear factor-kappa B [RANK]) and
TNFRSF11B [encoding the osteoprotegerin (OPG)] were involved in the RANK ligand (RANKL)/RANK/OPG pathway. Out of 14 loci which were significantly associated with any type of fracture at Bonferroni-corrected level of significance (
P=5×10
−4) in the previous GWASs meta-analysis (GEFOS-2), 4 SNPs from 4 loci, including
C18orf19/FAM 210A (rs4796995, 18p11.21),
DCDC5 (rs163879, 11p14.1),
WNT16 (rs3801387, 7q31.31) and
WNT4 (rs7521902, 1p36.12), were also associated with fractures.[
6]
Of the 64 BMD-related SNPs from 56 loci at genome-wide significance (
P<5×10
−8) in the largest previous GWASs meta-analysis (GEFOS-2), 29 SNPs (45.3%) from 28 loci were associated with osteoporosis-related traits among Korean subjects.[
6] Out of the rest 31 SNPs which did not reach the genome-wide significance in the previous study (GEFOS-2), 6 SNPs (19.4%) were associated with osteoporosis-related traits in Korean, as follows:
AKAP11 (rs7326472, 13q14.11),
ANAPC1 (rs17040773, 2q13),
BCL11A (rs730402, 2p16.1),
CYP19A1 (rs2118784, 15q21.2),
NAB1 (rs11675051, 2q32.2), and
PLVAP (rs7257450, 19p 13.11).[
6] The differences in results between the this study in Korean and the discovery stage analysis of the previous study (GEFOS-2) in Caucasian may be explained by ethnic differences, such as differences in allele frequencies and underlying LD structures and by the small sample size of this study (n=1,269).[
320] Another possible explanation for the differences in results between this study and the previous study (GEFOS-2) could be the heterogeneity of the study design including differences in the phenotype (osteoporosis, BMD, BMD site, fracture, and fracture type), in the adjusted covariates (age, weight, and height), and in the genetic model differences (additive, dominant, and recessive models). Considering the replication rate of BMD phenotype, 17 (17.7%) of the 96 BMD-related SNPs were associated with BMD in the Korean cohort. Associations of some SNPs in this study were only showed in the recessive models, so heterogeneity of genetic models between this study (additive, dominant, and recessive models) and the previous study (additive model) might be the differences in results.[
6]
To compare the replication rate of 95 SNPs in Korean women, we checked the replication rate of the previous Korean study involving 1,586 unrelated Korean women from a population-based cohort.[
21] Out of the 717 SNPs, there were 89 SNPs which were included in this study. The replication rate in this study (36.8%; 35 out of 95 SNPs) was comparable to that of a previous study (30.3%; 27 out of 89 SNPs).[
21] The differences in replicated SNPs among Korean subjects may be due to the use of different phenotypes between this study (BMD, osteoporosis, or fracture) and the previous study (only BMD). Another possible explanation for the differences in replicated SNPs could be the lack of statistical power due to the small sample size of both this study (n=1,269) and the previous study (n=1,586). The 14 replicated SNPs in both Korean studies were as follows:
AKAP11 (rs9533090, 13q14.11),
CTNNB1 (rs87938, 3p22.1),
DNM3 (rs479336, 1q24.3),
FOXL1 (rs10048146, 16q24.1),
GALNT3 (rs1346004, 16q24.1),
LEKR1 (rs344081, 3q25.31),
RPS6KA5 (rs1286077, 14q32.12),
TNFRSF11B (rs2062377, 8q24.12),
WLS (rs12407028, 1p31.3),
WNT16 (rs3801387, 7q31.31),
WNT4 (rs7521902, 1p36.12),
ZBTB40 (rs6426749, 1p36.12),
BCL11A (rs730402, 2p16.1), and
PLVAP (rs7257450, 19p13.11). Therefore, these 14 SNPS may represent true osteoporosis-related genetic markers in the Korean population.
Of the 35 SNPs associated with the osteoporosis-related traits in Korean subjects, 19 SNPs (54.3%) were associated with one or more osteoporosis-related traits in the other East Asian ethnic populations (Chinese and Japanese). Therefore, these 19 SNPs,
AKAP11 (rs9533090 and rs7326472),
ARHGAP1 (rs7932354),
AXIN1 (rs9921222),
C16orf38 (rs13336428),
C17orf53 (rs227584),
C18orf19 (rs4796995),
CTNNB1 (rs87938),
CYLD (rs1564981),
CYP19A1 (rs2118784),
GALNT3 (rs1346004),
KIAA2018 (rs1026364),
LRP5 (rs3736228),
MPP7 (rs3905706),
RPS6KA5 (rs1286077),
WLS (rs12407028),
WNT16 (rs3801387),
WNT4 (rs7521902), and
ZBTB40 (rs642674), may represent true osteoporosis-related genetic markers, regardless of ethnicity. Furthermore,
WNT16 (rs3801387) may represent true osteoporotic fracture-related genetic markers regardless of ethnicity. The replication failure was also reported in East-Asian populations. Heterogeneity, including different phenotype (measured site of BMD and type of fracture) and other confounding factors (age, sex, weight, and height) among the three East Asian ethnic populations, may have affected the association analyses in our study.[
3] Previous genetic studies showed sex and site specificity underlying BMD variation.[
6] The proportions of cortical and trabecular bone differ at the different sites (e.g., hip, spine and wrist). Furthermore, each type of fracture has its own unique risk factors.[
22] For instance, falls are a major risk factor for hip and wrist fractures; however, they contribute little to the risk of vertebral fractures. Epidemiology data also show that the prevalence of fractures at different sites is different according to age, sex, and ethnicity.[
22]
Our study has several limitations. First, the associations of the selected risk alleles were marginally significant [α (significance level of Bonferroni correction for multiple testing <
P<0.05; α=0.05/35 SNPs/three genetic models=0.00048). Therefore, there was the possibility of false positive results because multiple tests were performed. In addition, the lower replication rate of the SNPs which did not reach did not reach the genome-wide significance (19.4%) than that of the SNPs at genome-wide significance (45.3%) may suggest that some of 96 SNPs were candidate SNPs with considerable risk of false positivity. However, 35 SNPs were associated at
P<5×10
−6 in the discovery set of the GWAS and were tested for replication of association here.[
6] Second, there were some heterogeneity and other confounding factors among the three East Asian ethnic populations. Although we adjusted for age, sex, weight, and height, these confounding factors may have affected the results of the association analyses. Meta-analyses with less between-sample heterogeneity and other confounding factors, which may increase the power of study, were needed. Third, the design of our study was cross-sectional.
In summary, our results showed the common variants of osteoporosis-related traits in both Caucasian and East Asian populations. The possibility that these SNPs may represent true osteoporosis-related genetic markers should be further investigated.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download