Abstract
Purpose
The purpose of this study was to assess chemotherapy induced peripheral neuropathy (CIPN) and to examine the relationship between CIPN and depression.
Methods
A purposive sample of 105 patients treated with chemotherapy were recruited in the cross-sectional survey design. Data were collected using self-report questionnaires. The instruments used were the Chemotherapy Induced Peripheral Neuropathy Assessment Tool (CIPNAT) and Hospital Anxiety Depression Scale (HADS).
Results
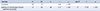
The most frequent suffering symptom of CIPN was 'tingling feeling in the hand and foot'. Of the motor symptoms, 'muscle weakness' was the most frequent symptom and 'muscle or joint aches' was the strongest suffering symptom of CIPN. The mean score for suffering of CIPN was 4.1. The mean score was 1.04 for depression and the prevalence was 48.5%. CIPN was significantly positively correlated with depression (r=.38, p<.001). The result of simple regression analysis revealed that CIPN was predictive of depression (R2=.136, p<.001).
Figures and Tables
Table 1
General Characteristics of the Subject (N=105)

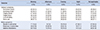
Table 2
Frequency, Suffering, and Experience of Chemotherapy-induced Peripheral Neuropathy (N=105)
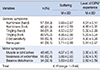
Table 3
Severe Time and Frequency of Chemotherapy-induced Peripheral Neuropathy (N=105)
References
1. Wolf S, Barton D, Kottschade L, Grothey A, Loprinzi C. Chemotherapy-induced peripheral neuropathy: prevention and treatment strategies. Eur J Cancer. 2008; 44(11):1507–1515.

2. Argyriou AA, Bruna J, Marmiroli P, Cavaletti G. Chemotherapy-induced peripheral neurotoxicity (CIPN): An update. Crit Rev Oncol Hemat. 2012; 82(1):51–77. DOI: 10.1016/j.critrevonc.2011.04.012.

3. Hausheer FH, Schilsky RL, Bain S, Berghorn EJ, Lieberman F. Diagnosis, management, and evaluation of chemotherapy-induced peripheral neuropathy. Semin Oncol. 2006; 33(1):15–49.

4. Tofthagen CS, McMillan SC, Kip KE. Development and psychometric evaluation of the chemotherapy-induced peripheral neuropathy assessment tool. Cancer Nurs. 2011; 34(4):E10–E20.

5. Windebank AJ, Grisold W. Chemotherapy-induced neuropathy. J Peripher Nerv Syst. 2008; 13(1):27–46.

6. Rosson GD. Chemotherapy-induced neuropathy. Clin Podiatr Med Surg. 2006; 23(3):637–649. DOI: 10.1016/j.cpm.2006.04.009.

7. Kim JH, Lee KM, Jeon MJ, Seol ME, Lee SH, Park JY. Symptom and interference of activities of daily living of chemotherapy-induced peripheral neuropathy in patients receiving taxanes and platinums. Asian Oncol Nurs. 2013; 13(3):145–151.

8. Hwang WH. Assessment using CIPNAT for peripheral neuropathy in cancer patients undergoing chemotherapy [master's thesis]. Busan: Kosin Univ.;2013.
9. Kwak MK, Kim EJ, Lee ER, Kwon IG, Hwang MS. Characteristics and quality of life in patients with chemotherapy-induced peripheral neuropathy. J Korean Oncol Nurs. 2010; 10(2):231–239.

10. Kim HY, Kang JH, Song JE, Youn HJ. Chemotherapy-induced peripheral neuropathy and quality of life in breast cancer patients. Asian Oncol Nurs. 2013; 13(4):222–230.

11. Montgomery GH, Borbjerg DH. Pre-surgery distress and specific response expectancies predict post-surgery outcomes in surgery patients confronting breast cancer. Health Psychol. 2004; 23(4):381–387.

12. Lee SY, Ham YH, Ok ON, Kim EJ, Kwon IG, Hwang MS, et al. The effects of foot reflexology on peripheral neuropathy, symptom distress, anxiety and depression in cancer patients treated with oxaliplatin. Asian Oncol Nurs. 2012; 12(4):305–313.

13. Faul F, Erdfelder E, Lang AG, Buchner A. G*Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav Res Methods. 2007; 39(2):175–191.

14. Tofthagen CS, McMillan SC, Kip KE. Development and psychometric evaluation of the chemotherapy-induced peripheral neuropathy assessment tool. Cancer Nurs. 2011; 34(4):E10–E20.

15. Oh SM, Min KJ, Park DB. A comparison of normal, depressed and anxious groups: A study on the standardization of the hospital anxiety and depressed scale for Koreans. J Korean Neuropsychiatr Assoc. 1999; 38(2):289–296.
16. Kwak MK, Kim EJ, Lee ER, Kwon IG, Hwang MS. Characteristics and quality of life in patients with chemotherapy-induced peripheral neuropathy. J Korean Oncol Nurs. 2010; 10(2):231–239.

17. Kim HM. Symptoms and relief therapy related to chemotherapy induced peripheral neuropathy in patients with cancer. Daegu: Keimyung Univ.;2012.
18. Park AR, Kim SJ, Bang JS, La HO. Oxaliplatin-induced Peripheral Neuropathy in Patients with advanced or metastatic gastric cancer. Korean J Clin Pharm. 2009; 19(1):18–22.
19. Speck RM, DeMichele A, Farrar JT, Hennessy S, Mao JJ, Stineman MG, et al. Scope of symptoms and self-management strategies for chemotherapy-induced peripheral neuropathy in breast cancer patients. Support Care Cancer. 2012; 20(10):2433–2439.

20. Visovsky C, Collins M, Abbott L, Aschenbrenner J, Hart C. Putting evidence into practice: evidence-based interventions for chemotherapy-induced peripheral neuropathy. Clin J Oncol Nurs. 2007; 11(6):901–913.

21. Pietrangeli A, Leandri M, Terzoli E, Jandolo B, Garufi C. Persistence of high-dose oxaliplatin-induced neuropathy at long-term follow-up. Eur Neurol. 2006; 56(1):13–16.

22. Ostchega Y, Donohue M, Fox N. High-dose cisplatin-related peripheral neuropathy. Cancer Nurs. 1988; 11(1):23–32.

23. Lee IH. Easy Flow regression analysis. Seoul: Hannarae;2014. p. 313–316.
24. Cohen J. Statistical power analysis for the behavioral sciences. Hillsdale, NJ: Erlbaum;1988.
25. Cappiello M, Cunningham RS, Knobf MT, Erdos D. Breast cancer survivors. Clin Nurs Res. 2007; 16(4):278–293.

26. Baek YA. The correlation among symptoms, anxiety, depression and quality of life in patients with colorectal cancer undergoing chemotherapy [master's thesis]. Seoul: Seoul Univ.;2013.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download