II. Materials and Methods
Of the 262 patients who underwent cyst enucleation between September 2005 and April 2014 after being diagnosed with mandibular cystic or cystic-appearing lesions at the Department of Oral and Maxillofacial Surgery in Gangnam Severance Hospital, 81 patients with obvious cystic lesions involving IMTM on panoramic radiographs were selected for the present study. Of these 81 subjects, 53 patients were male, 28 patients were female, and their mean age was 40.3 years. All 81 patients underwent preoperative panoramic radiographs (Promax; Planmeca, Helsinki, Finland), and 63 patients underwent CT imaging (Somatom Sensation 64 scanner; Siemens, Erlangen, Germany). Using the panoramic radiographs and CT findings of the mandibular cystic lesions, the relationships between the lesion growth patterns and adjacent teeth were investigated based on their relationship with and displacement of IMTM. Institutional review board approval was granted at the institutional review board of Yonsei University Gangnam Severance Hospital (IRB #3-2014-0085).
1. Displacement of the IMTM
Using panoramic radiographs and CT images, the position and displacement of the IMTM was assessed. The positional relationship between the cystic lesion and IMTM was determined as follows:
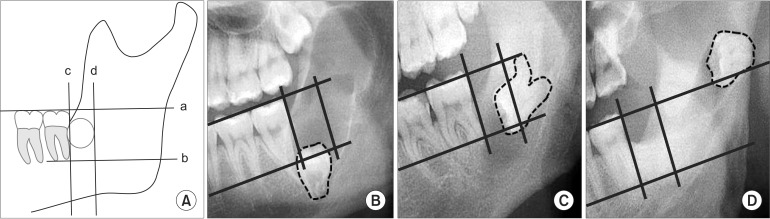
1) Mesio-distal (MD) displacement and direction of IMTM
Displacement of the IMTM was categorized by direction as diagnosed on panoramic radiographs. If the center of the third molar was positioned below the line passing through the root tips of the adjacent normal erupted second molar, then the displacement was categorized as downward. If the center of the third molar was positioned above the extended line of the occlusal plane, then the displacement was categorized as upward. When the third molar was displaced beyond the MD width of the adjacent second molar towards the distal side of the second molar, then the displacement was categorized as backward. In cases of missing, root resorption, or ectopic displacement of the mesially positioned molar teeth, the region was measured assuming normal posterior tooth eruption. Any position that did not deviate from these standards was considered normal.(
Fig. 1)
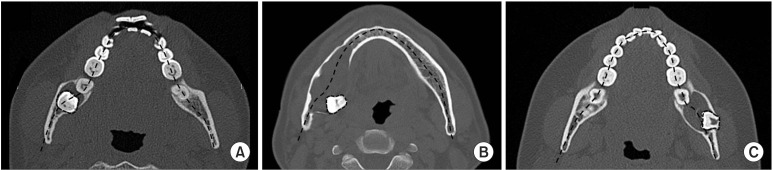
2) Bucco-lingual (BL) displacement of the IMTM
If the CT axial view showed that the center of the third molar was positioned on the arch curvature, then it was determined that no displacement occurred. When the center of the third molar deviated from the arch curvature, the displacement of the third molar was categorized as buccal or lingual displacement.(
Fig. 2)
2. Calculation of lesion size
In the CT axial view, the largest MD width of the lesion was selected and the largest BL width perpendicular to the MD width was measured accordingly. The ratio between the BL width to the MD width was then calculated
5.
3. Growth pattern of mandibular cystic lesions
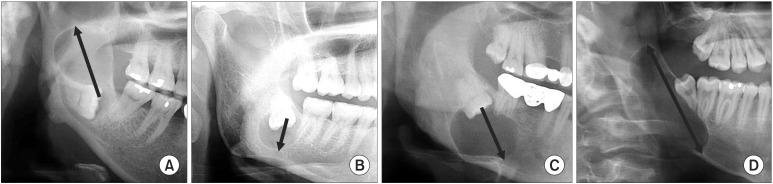
1) Anterior-posterior growth pattern
Assuming that a cystic lesion occurred in the normal position of the third molar behind the second molar, the growth pattern of the cystic lesion was categorized as back-upward when the lesion exhibited growth towards the condylar head of the mandible. When the lesion exhibited growth towards the mandibular border, the growth pattern was categorized as downward. Finally, when the lesion growth was downward towards the second molar, the growth pattern was categorized as down-forward.(
Fig. 3)
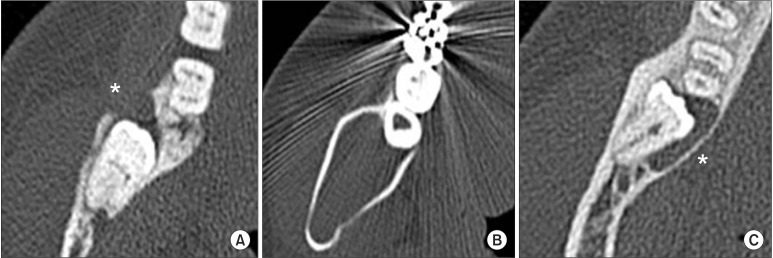
2) BL growth pattern
Buccal and lingual growth was determined by analyzing the CT axial view.(
Fig. 4)
4. Occurrence of cortical bone expansion and loss of bony continuity
The occurrence of cortical bone expansion and loss of bony continuity on the cystic lesions were determined by analyzing the CT scans.
5. Root resorption
Root resorption of adjacent tooth was assessed only when the lesion involved the root of the adjacent tooth.
6. Statistical analysis
Data were analyzed using the PASW Statistics 18.0 (IBM Co., Armonk, NY, USA). Lesions were classified into either the DC group or non-DC group. The non-DC group included OKC and AB. Because paradental cysts and glandular odontogenic cysts were very rare, we did not consider them in the statistical analysis. Fisher's exact test was used to analyze MD and BL displacement of the IMTM, cortical bone expansion of the lesion and root resorption of the adjacent tooth. Chi-square test was used to analyze the loss of bone continuity around the lesion, and the Mann-Whitney test was used to analyze the BL/MD ratio of lesions.
III. Results
The present study investigated 81 cases of cystic and cystic-appearing lesions involving the IMTM by performing a comparative analysis of the panoramic radiographs and CT scans of the respective lesions and obtained the following results.
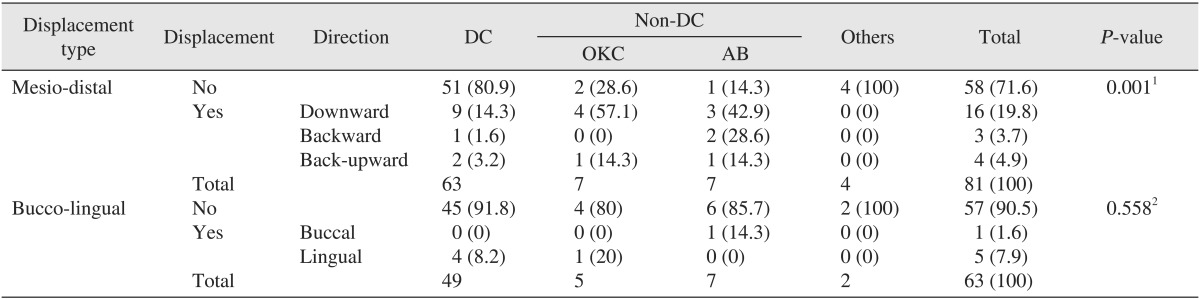
Of the 81 cystic lesions, DC was the most common type at 77.8% (63/81 cases), followed by OKC and AB at 8.6% (7/81 cases) each. The others included 3 paradental cysts and 1 glandular odontogenic cyst. The mean patient age of the three major groups was 42.5, 33.9, and 22.9 years in the DC, OKC, and AB group, respectively.(
Table 1)
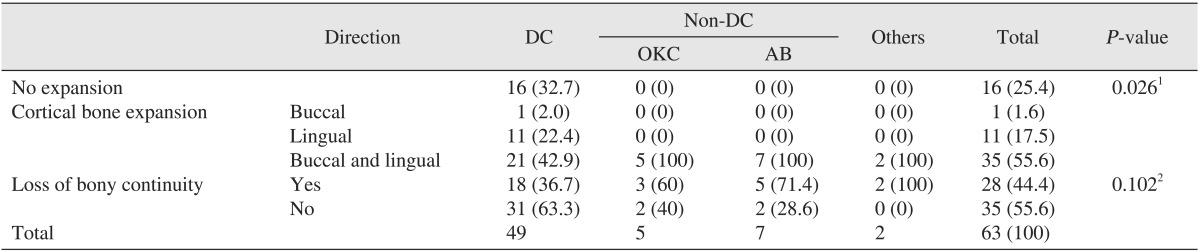
The panoramic radiographs revealed a MD displacement incidence of the third molars of 28.4% (23/81 cases) and an incidence rate according to lesion type of 19.1% (12/63 cases), 71.4% (5/7 cases), and 85.7% (6/7 cases) for the DC, OKC, and AB group, respectively. The incidence of MD displacement in the DC group was significantly lower than that of the non-DC group, and the odds ratio of the IMTM was 15.6 (95% confidence interval, 3.8 to 64.7). The direction of MD displacement was typically downward, accounting for 69.6% (16/23 cases) of the lesions exhibiting displacement. Other lesion types showed no evidence of tooth displacement. When BL displacement of the third molar was observed on the CT axial view, the tooth was most commonly aligned on the arch curvature in 90.5% (57/63) of cases; in contrast, only 7.9% (5/63) of cases exhibited lingual displacement, and 1.6% (1/63) of cases exhibited buccal displacement.(
Table 2)
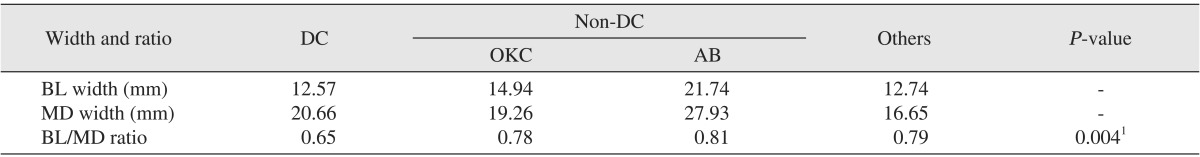
The ratios of BL to MD width (BL/MD ratio) of the OKC and AB group were 0.78 and 0.81, respectively, which were significantly greater than the BL/MD ratio of the DC group (0.65).(
Table 3)
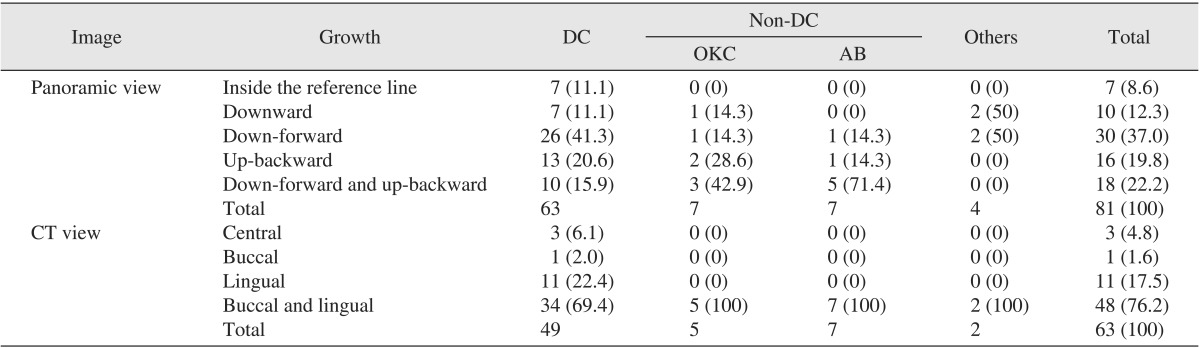
When the MD growth pattern of the lesions was investigated, the DC group most commonly exhibited down-forward growth alone in 41.3% (26/63) of cases. In the AB and OKC group, the majority of lesions exhibited both down-forward and back-upward growth simultaneously, in 42.9% (3/7) of cases and 71.4% (5/7) of cases, respectively, higher than 15.9% (10/63) of cases in the DC group.
In the lesions exhibiting a buccal or lingual growth pattern, 69.4% (34/49 cases) of the DC group exhibited simultaneous buccal and lingual growth, whereas, all of the AB and OKC groups (5/5 and 7/7 cases, respectively) exhibited simultaneous growth in the buccal and lingual directions.(
Table 4)
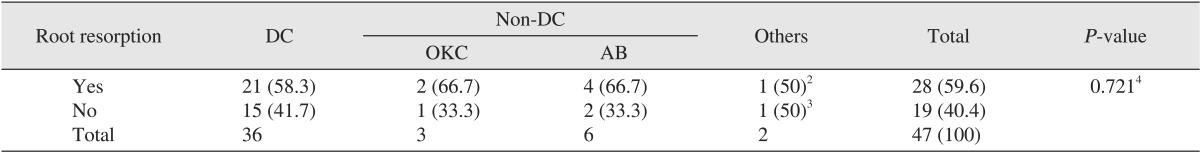
Cortical bone expansion was observed in 67.3% (33/49 cases) of cases in the DC group. Both the OKC and AB groups exhibited cortical bone expansion in 100% of cases (5/5 and 7/7 cases, respectively). A loss of bone continuity was observed in 36.7% (18/49) of cases in the DC group, 60% (3/5) of cases in the OKC group, and 71.4% (5/7) of cases in the AB group.(
Table 5)
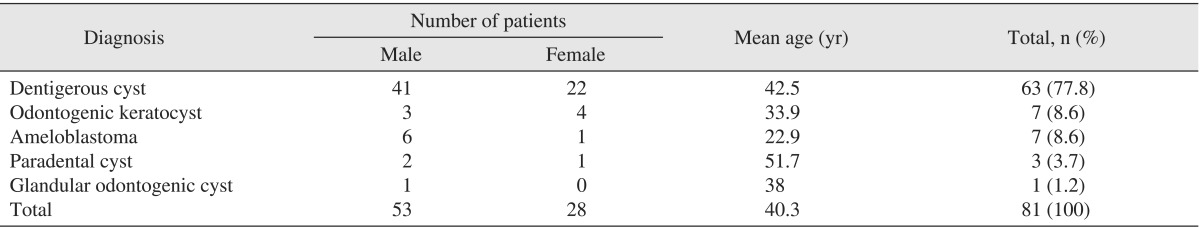
Root resorption in the adjacent second molar was found in 58.3% (21/36) of cases in the DC group, 66.7% (2/3) of cases in the OKC group, and 67.7% (4/6) of cases in the AB group.(
Table 6)
IV. Discussion
The most common clinical symptom of a mandibular cystic lesion is pain, sometimes accompanied by swelling. Other clinical symptoms include paresthesia, tooth displacement, and tooth mobility. However, the presence or absence of clinical symptoms does not always aid the differential diagnosis. Furthermore, early lesions are often asymptomatic, and in most cases, lesions are detected on routine dental radiographs, such as panoramic radiographs, prior to a patient being aware of them
3. In such situations, the dentist should inform patients about the discovered lesions.
Radiologic differential diagnosis of cystic lesions is performed by considering the morphologic findings and the relationship to adjacent structures. Even lesions exhibiting identical histopathologic findings can show varying radiologic features depending on their position, size, and growth stage. Conversely, distinct histopathologic lesions may exhibit similar radiologic features, thus posing difficulties in differential diagnosis
4.
Although cystic lesions can be confirmed by preoperative biopsy in some cases, it is impractical to perform a biopsy for every lesion. Therefore, preoperative clinical and radiologic differential diagnoses are performed in many cases. Consequently, the postoperative histopathologic findings after biopsy may differ from the preoperatively predicted results
3.
The majority of mandibular cystic lesions are benign, but certain lesions can be show aggressive or destructive growth
3. The differing histopathologic characteristics of the lesions can influence prognosis, including the postoperative recurrence rate. As such, a more accurate initial differential diagnosis would aid surgeons
4. For instance, patients should be warned of the aggressive growth potential and likelihood of recurrence preoperatively; further treatment such as curettage, grinding or even radical resection might be considered when OKC or AB is suspected based on the radiographic examinations.
DCs, OKC, and AB lesions exhibit morphologic differences due to their varying internal compositions and border patterns. When OKC and DC are compared, the histopathologic patterns, particularly the presence of keratin, determine the lesion morphology
5. When the CT findings of AB and DC lesions are compared, the former exhibits a more aggressive growth pattern than the latter
6. In addition, the anatomic position, growth period, and lesion size can lead to differences in lesion morphology, and the different growth patterns of the lesions can influence displacement of the impacted tooth
7. Consequently, the present study sought to identify the characteristic findings of these different lesions by investigating the growth patterns of mandibular cystic lesions and the displacement of the IMTM.
The most common type of odontogenic cyst, DC, is present in 46%
8 to 53%
9 of impacted third molars
10. OKC is also closely associated with an impacted tooth and is the second most common odontogenic cyst
11. In a study investigating the prevalence of tumors and cystic lesions associated with 9,994 impacted third molars, cystic lesions were more commonly observed (2.31%; n=231) than tumorous lesions. Among tumors, AB was the most commonly observed (0.41%, n=41)
12 and was identified as the most common odontogenic tumor
4,
12,
13,
14. Among the 81 cystic lesions investigated in this study, DCs were the most common, representing 77.8% of cases, followed by OKC and AB in 8.6% of cases each. When a cystic lesion involving an IMTM appears on panoramic radiographs, there is a high probability that the cystic lesion is a DC.
DCs are known to occur more frequently in patients aged 20 years or older
8,
9; the mean age of the DC group in this study was 42.5 years. OKC generally occurs in patients between ages 20 to 50 years
15; the mean age of the OKC group in this study was 33.3 years. AB most typically occurs in patients between the age of 20 to 40 years
10,
13; the mean age of the AB group in this study was 22.9 years.
Third molars involved in cystic lesions exhibit more severe impaction patterns than those uninvolved in cystic lesions
16. Tsukamoto et al.
7 reported that aggressive proliferation of a lesion is unlikely to cause tooth displacement, ascribing this observation to the rapid growth of these lesions, which provides insufficient time for the third molar to become displaced. However, the incidence of MD displacement was the lowest in the DC group in this study. This result may reflect the focus of the present study; rather than examining the correlation between lesion size and displacement severity, this study focused on the absence or presence of tooth displacement. Due to focusing only on the presence of tooth displacement, there was a high probability that a cystic lesion was OKC or AB when MD displacement was observed.
When BL displacement of the third molar was observed on the CT axial view, there was a higher incidence of lingual displacement compared to buccal displacement, presumably because the cortical bone is relatively thinner lingually, which favors third molar displacement towards the lingual side. However, the difference in the incidence of BL displacement between the DC and non-DC group was not statistically significant.
Compared to maxillary lesions, mandibular lesions have limited space for growth owing to buccal and lingual firm cortical bone, and thus, grow mesio-distally in a long oval shape
6. Because of the elevated internal pressure induced by keratin deposition at the epithelium of the cyst and the strong osteoclast activity of prostaglandins generated by the epithelial cells, OKC exhibits a faster growth pattern. AB is also known to be relatively invasive and aggressive
14. In this study, OKC and AB showed a high BL/MD ratio, presumably because of their faster growth rate and more destructive tendency compared to DC. Therefore, these two lesions precipitate buccal and lingual cortical bone expansion, further accelerating BL growth of the lesion. Consequently, the cystic lesions caused by these two etiologies have a more circular shape on the CT axial view compared to the oval shaped lesions of the DC group. In this study, as well, the BL/MD ratio was significantly higher in the OKC and AB group than in the DC group.
The growth direction of the lesion is also presumably associated with the growth pattern of the lesion. When MD growth of the lesion was observed, the DC group, which has relatively slow growing lesions, predominantly exhibited unilateral growth. When BL growth of the lesion was observed, a relatively high proportion of DCs (22.4%) exhibited unilateral growth towards the lingual side. In contrast, 100% of the AB and OKC cases exhibited simultaneous buccal and lingual growth.
As lesions grow, large lesions may cause cortical bone expansion, loss of bony continuity and root resorption of the adjacent tooth
14. The fact that cortical bone expansion and loss of bony continuity was greater in the OKC and AB groups than the DC group demonstrates the different growth rates and aggressiveness among the different lesions
17.
Notably, when root resorption rates were investigated in cases where a lesion involved the root of the adjacent second molar, the OKC and AB group each exhibited a 66.7% root resorption rate. DCs also exhibited a relatively high root resorption rate of 58.3%, thus demonstrating that root resorption alone is not useful for differential diagnosis.
Further research based on a greater number cases including other types of cystic lesions is needed for future studies.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download