Abstract
A 59-year-old man with multifocal cerebral infarction was found to have the large obstructive mitral valvular mass. Although benign tumor was under suspicion before surgery, he was finally diagnosed as chronic infective endocarditis by microscopic evaluation. The precise diagnosis and the proper management of a cardiac mass are very important since even the benign tumor may cause fatal complications. However, primary cardiac mass has the broad spectrum from pseudo-tumor to malignancy and the differential diagnosis using non-invasive methods is not easy even with the currently available imaging techniques.
Cardiac tumors are rare but the spectrum of tumors is very broad including benign mass, malignancy and pseudo-tumor. The differential diagnosis is not easy although various imaging modalities have become available for the evaluation of the mass.1) However, even the benign mass can cause the significant clinical event with hemodynamic changes or embolic complications. 2) Therefore, the precise diagnosis and the proper management of the cardiac mass are crucial. This is the case of a patient with cardioembolic cerebral infarction caused by the large obstructive mitral valvular mass which was unexpectedly diagnosed as chronic infective endocarditis.
A 59-year-old male came to the emergency room for dysarthria and confused mentality. He had no history of any cardiovascular disease but smoking history of 20 pack-year. His vital sign was stable without fever. Laboratory findings including cardiac enzyme and inflammatory markers were within normal limits (white blood cell 5400/µL, high sensitivity C-reactive protein 1.94 mg/L, erythrocyte sedimentation rate 6 mL/hr). Brain magnetic resonance (MR) imaging showed the multifocal diffusion restrictions implying acute cerebral infarction. Cerebrovascular angiography and thrombectomy were performed, and red thrombi with whitish amorphous materials were acquired from the procedure.
With the strong suspicion of cardioembolic cerebral infarction, echocardiography was performed. Severe mitral stenosis was diagnosed with large echogenic mass on lateral mitral commissure. On transesophageal echocardiograph, 19.9 × 14.4 mm2 sized round mass obstructing lateral portion of mitral valve was observed with the oscillating strands and tags on its atrial surface (Fig. 1). However, medial portion of the anterior and posterior mitral leaflets were relatively spared. On cardiac MR, the mass showed the low signal intensity in early perfusion image and the high signal intensity in delayed enhancement image (Fig. 2). Avascular, non-inflammatory fibrotic lesion such as fibroma, myxoma or degenerative change in lateral commissure of mitral leaflets was suggested.1)
For the strong concern of recurrent embolic event, the patient underwent the mass removal and mitral valve replacement. When left atriotomy was performed, the firm and round mass-like material was found. The round and well demarcated but irregularly surfaced orifice was presented on the atrial side. The hard and greyish surface was observed with filthy, amorphous oscillating structures on it. However, the medial portion of mitral apparatus was grossly normal (Fig. 3). On microscopic exam, there were extensively thickened valvular leaflets with organizing thrombus which was filled with plenty of lymphocytes and plasma cells (Fig. 4). Retrospectively, laboratory findings were reviewed to rule out possible diagnosis of nonbacterial thrombotic endocarditis. However serologic markers including FANA, ANCA and anti-phospholipid antibody were all negative3) and there was no evidence of hidden malignancy. Finally, the patient was diagnosed as chronic infective endocarditis, and was treated with Ampicillin-Sulbactam for four weeks although the result of tissue culture was negative.
Recently, the advanced non-invasive evaluation of the cardiac mass has become available including the tissue characterization with cardiac MR imaging. Cardiac MR imaging basically shows the water and fat content of the tissue using T1 and T2 image. In addition, contrast enhancement image presents vascularity and the presence of fibrosis of the mass. The analysis of signal intensities of each image helps more accurate diagnosis. With the idea of the mass location, the spectrum of the mass for the differential diagnosis may become much narrower because commonly developing masses are different by their location.2) Therefore, more exact prediction of the diagnosis and following proper management is expected. However, as presented in the case, differential diagnosis of the cardiac mass is still not easy even when various imaging modalities are incorporated.
The patient in the case was misdiagnosed at first because imaging studies showed far localized large obstructive mass on the lateral mitral commissure but with intact both leaflets. No one had the suspicion of infective endocarditis with the mass although the most popular valvular mass is the pseudotumor diagnosed with vegetation in infective endocarditis and cardioembolic infarction is one of the most common findings of infective endocarditis. Instead, avascular, fibrotic valvular mass such as fibroma was suggested from the findings of cardiac MR imaging.
MR findings of the vegetation presented in infective endocarditis are not typical. Although vegetative mass is not commonly enhanced in early perfusion image, the signal intensity of delayed contrast enhancement image does not show consistency, and propagation of the infection is detected with delayed contrast enhancement on the endothelial lining sometimes.4) Therefore, the clinical condition of the patient is the most important factor for the differential diagnosis. The fact that up to 90% of the infective endocarditis patients experience fever and other signs of systemic infection and even patients with the subacute or chronic stage of infective endocarditis show at least malaise and increased inflammatory markers such as C-reactive protein or erythrocyte sediment rate5) made the differential diagnosis more difficult in this case.
However, the relatively filthy appearance of atrial side compared to ventricular surface of the mass filled with inflammatory cells and organizing thrombus is the conclusive evidence of the infective endocarditis. Not neutrophil but lymphocytes, plasma cells and giant cells without visible microorganism suggest the subacute to chronic phase of the infective endocarditis.6) Therefore, his case can be re-diagnosed as chronic infective endocarditis with cardioembolic event due to the mitral valvular vegetation. There was no symptom or sign of infection because of its chronic stage and cardiac MR findings might be compatible to chronic infective endocarditis with the vegetative mass which showed low signal intensity at early perfusion image due to the chronic inflammatory change and the high signal intensity at delayed contrast enhancement due to the fibrosis. A large vegetative thrombus can be presented as a valvular mass when it has chronic and fibrotic inflammatory tissues with relatively intact surrounding structures.
Figures and Tables
Fig. 1
Transthoracic (A) and transesophageal (B) echocardiographic images of the mitral valvular mass. The mass was located on lateral mitral commissure, which made severe mitral stenosis. The surface of mass had several irregular with oscillating strands and tags.

Fig. 2
Early perfusion image (A) and late gadolinium enhance image (B) of the mitral valve (arrow). At early perfusion image, the mass showed low signal intensity whereas high signal intensity was detected on late gadolinium enhance image.
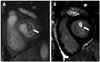
Fig. 3
Gross image of the mitral valve apparatus shows well demarcated mass with greyish surface and filthy, amorphous oscillating structures on it in atrial side (A), but grossly normal valvular surface in ventricular side (B).

Fig. 4
Microscopic finding (hematoxylin and eosin, × 100) of the mitral valvular mass were composed of extensively thickened valvular leaflets with organizing thrombus. On valvular structure, plenty of lymphocytes and plasma cells on atrial surface and myxoid degeneration in ventricular side were presented.

References
1. Motwani M, Kidambi A, Herzog BA, Uddin A, Greenwood JP, Plein S. MR imaging of cardiac tumors and masses: a review of methods and clinical applications. Radiology. 2013; 268:26–43.
2. Shapiro LM. Cardiac tumours: diagnosis and management. Heart. 2001; 85:218–222.
3. Joffe II, Jacobs LE, Owen AN, Ioli A, Kotler MN. Noninfective valvular masses: review of the literature with emphasis on imaging techniques and management. Am Heart J. 1996; 131:1175–1183.
4. Dursun M, Yılmaz S, Yılmaz E, Yılmaz R, Onur İ, Oflaz H, Dindar A. The utility of cardiac MRI in diagnosis of infective endocarditis: preliminary results. Diagn Interv Radiol. 2015; 21:28–33.
5. Habib G, Lancellotti P, Antunes MJ, Bongiorni MG, Casalta JP, Del Zotti F, Dulgheru R, El Khoury G, Erba PA, Iung B, Miro JM, Mulder BJ, Plonska-Gosciniak E, Price S, Roos-Hesselink J, Snygg-Martin U, Thuny F, Tornos Mas P, Vilacosta I, Zamorano JL, Erol Ç, Nihoyannopoulos P, Aboyans V, Agewall S, Athanassopoulos G, Aytekin S, Benzer W, Bueno H, Broekhuizen L, Carerj S, Cosyns B, De Backer J, De Bonis M, Dimopoulos K, Donal E, Drexel H, Flachskampf FA, Hall R, Halvorsen S, Hoen B, Kirchhof P, Lainscak M, Leite-Moreira AF, Lip GY, Mestres CA, Piepoli MF, Punjabi PP, Rapezzi C, Rosenhek R, Siebens K, Tamargo J, Walker DM. Authors/Task Force Members. Document Reviewers. 2015 ESC Guidelines for the management of infective endocarditis: The Task Force for the Management of Infective Endocarditis of the European Society of Cardiology (ESC)Endorsed by: European Association for Cardio-Thoracic Surgery (EACTS), the European Association of Nuclear Medicine (EANM). Eur Heart J. 2015; 36:3075–3128.
6. Thiene G, Basso C. Pathology and pathogenesis of infective endocarditis in native heart valves. Cardiovasc Pathol. 2006; 15:256–263.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download