Abstract
A 68-year-old woman visited the emergency department twice with symptoms of acute heart failure including shortness of breath, general weakness, and abdominal distension. Laboratory findings showed extremely low level of serum hemoglobin at 1.4 g/dL. Echocardiographic examination demonstrated dilated left ventricular cavity with systolic dysfunction and moderate amount of pericardial effusion. In this patient, acute heart failure due to severe iron deficiency anemia was caused by inappropriate habitual bloodletting.
In patients with heart failure (HF), anemia usually develops during the course of the disease and have adverse impact on the long-term clinical outcomes.1
On the other hand, chronic severe anemia itself can cause high cardiac output state leading to adverse left ventricular (LV) remodeling and development of overt HF. Herein, we report a case of recurrent acute decompensated HF due to chronic severe anemia caused by inappropriate habitual bloodletting.
A 68-year-old female visited the emergency department for complaint of shortness of breath, general weakness and abdominal distension which had progressed over the preceding several weeks. The patient looked pale. Blood pressure was 116/80 mm Hg, and her pulse rate was 75/min. On examination, no cardiac murmurs were heard but fine inspiratory crackles were audible in both lower lung fields. Jugular veins were engorged, abdomen was distended, and both lower extremities were swollen. The electrocardiography showed sinus rhythm with right axis deviation and poor R-wave progression (Fig. 1) and the chest radiography revealed marked cardiomegaly, pulmonary edema, and bilateral pleural effusion (Fig. 2). Her venous blood was pinkish. Initial hemoglobin level was 1.4 g/dL, the hematocrit level was 6.3%, the mean corpuscular volume was 60.1 fL, and the red-cell distribution width was 20.0%. Iron studies confirmed iron-deficiency anemia, with an iron level of 6 µg/dL; total iron-binding capacity, 471 µg/dL; percent iron saturation, 1%; and ferritin, 2 ng/mL. Cardiac enzymes were within normal ranges, but N-terminal pro B-type natriuretic peptide was noticeably elevated at 3559 pg/mL. The patient was admitted for evaluation and management of severe anemia and acute HF.
Transthoracic echocardiography was conducted and showed dilated LV cavity with mild systolic dysfunction and moderate functional mitral regurgitation. LV ejection fraction was 44% calculated by biplane Simpson's method. Right ventricular (RV) cavity was also dilated and systolic function was preserved. Pulmonary hypertension was accompanied by moderate tricuspid regurgitation (estimated pulmonary artery systolic pressure of 50 mm Hg). In addition, moderate amount of pericardial effusion was observed (Fig. 3). To rule out bleeding, endoscopy was performed and revealed no source of bleeding in gastrointestinal tract.
In her past medical history, the patient had a mastectomy for the treatment of breast cancer about 30 years before. Several months after surgery, she had a traffic accident which had made her less mobile. Since then, she spent most of her time at home and treat chronic pain by herself with bloodletting called 'Sahyeol' for decades instead of receiving medical treatment. As a result, habitual bloodletting caused severe chronic anemia and HF. During hospitalization, the patient received transfusion with several units of packed red blood cells and received the drug treatment including furosemide, carvedilol, perindopril, and oral iron sulfate. Regarding inappropriate habitual bloodletting, consultation to neuropsychiatry department replied that she was suspected to have schizoid personality disorder, which should be managed with antipsychotics. However, she was lost to follow-up after discharge.
About one year later, she was brought to the emergency department by her sister because the patient suffered worsening general weakness and edema for several weeks. After her last discharge, she returned to her lifestyle and restarted bloodletting using acupuncture. Again, the hemoglobin level was 1.5 g/dL. Echocardiographic examination was performed and demonstrated dilated LV cavity with borderline LV systolic function and mild mitral regurgitation. Ejection fraction was 55%, somewhat improved compared with previous test. Small amount of pericardial effusion was visible. RV was still dilated and pulmonary hypertension persisted with moderate tricuspid regurgitation (estimated pulmonary artery systolic pressure of 50 mm Hg) (Fig. 4). On admission, the patient received a blood transfusion and was treated for acute HF. After medical stabilization, the patient was transferred to the neuropsychiatry ward for further management.
Anemia is common in patients with HF and is associated with worse long-term clinical outcomes.2)
The prevalence of anemia ranged from 15% to 55% among ambulatory HF patients.1) In most cases, anemia develops during the course of HF especially in those with old age, diabetes, chronic kidney disease, and lower exercise capacity. However, chronic severe anemia itself can cause in high cardiac output state and contribute to the development of HF.3)
The mechanisms by which chronic severe anemia cause HF are not well understood. One possible explanation is that low hemoglobin level decreases systemic vascular resistance as the result of reduction in blood viscosity and enhanced vasodilation. 2) Low systemic vascular resistance lowers blood pressure and causes neurohormonal activation, which results in decreased glomerular filtration rate, salt and water retention, and extracellular volume expansion. The expansion of extracellular volume in concert with vasodilation increases the cardiac output, which augments oxygen delivery to tissues. In the long-term, high output state leads to LV remodeling such as LV hypertrophy and dilation, and the development of overt HF. However, iron deficiency itself can cause contractile dysfunction of cardiomyocytes, as iron is essential in cells requiring large amount of energy.4) In our case, the patient was not in high output state and LV ejection fraction was reduced, which implies that chronic iron deficiency is associated in part with LV dysfunction.
The evidences for the management of high output HF is lacking. Generally, treatment should be aimed at correction of the underlying conditions which cause high cardiac output.3) In cases of HF caused by severe anemia, correction of anemia can rapidly reverse high output state and fluid retention, if LV function is normal.5) However, in patients in whom LV dysfunction is present, antagonists against neurohormonal activation such as beta-blockers, angiotensin-converting enzyme inhibitors should be considered along with administration of diuretics and anemia correction,6) as in our case.
In oriental medicine, bloodletting is occasionally conducted at home as well as clinic to relieve nonspecific pain. In this case, a 68-year-old woman had severe chronic anemia due to habitual bloodletting called 'Sahyeol' inappropriately performed by herself for decades. She was obsessed with blood-letting, which implied a psychiatric problem. Therefore, the patient was consulted to the neuropsychiatry department and suspected to have schizoid personality disorder. Although antipsychotic agents were started and she was scheduled to visit the outpatient clinic of psychiatry, she was lost to follow-up after discharge. After one year, she was presented to the emergency department due to repeated episode of acute decompensated HF with severe anemia. On her second admission, she was transferred to the neuropsychiatry ward to correct 'underlying condition' causing severe anemia after medical stabilization.
Sohn et al.7) reported a similar case of bloodletting-induced cardiomyopathy, in which case decreased LV function was completely recovered after successful treatment of HF and anemia. However, the echocardiographic follow-up in this patient showed borderline LV function, which was a modest recovery from the initial exam. The reason for this modest improvement of LV function is uncertain, although initial hemoglobin levels were similar between two admissions. One possible explanation is that LV function might be recovered after anemia correction on her first admission, however, it began to re-deteriorate due to anemia recurrence from bizarre repetitive bloodletting just before her second admission. On the other hand, there was no interval change of RV dilatation and pulmonary hypertension, which implies consequences of volume overload from high output state.
In conclusion, we report here a rare case showing repeated acute decompensated HF owing to severe iron deficiency anemia caused by inappropriate habitual bloodletting. In such cases, the treatment should be focused not only at the management of HF and anemia correction but also at the psychiatric counseling. Considering that bloodletting is performed by individuals in South Korea as a folk remedy, it is of paramount importance to announce that it could actually cause anemia as well as HF.
Figures and Tables
Fig. 1
The 12-lead electrocardiogram showed normal sinus rhythm at a rate of 75 bpm, right axis deviation, and poor R-wave progression.
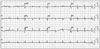
Fig. 2
The initial chest radiography demonstrated marked cardiomegaly and pulmonary edema with bilateral pleural effusion (A). After treatment of acute heart failure and anemia, follow-up radiograph showed a modest regression of cardiomegaly and resolution of pulmonary edema and pleural effusion (B).

Fig. 3
The transthoracic echocardiography revealed dilated left ventricular (LV) cavity (LV end-diastolic dimension = 63 mm) with mild LV dysfunction, eccentric LV hypertrophy, left atrial enlargement and moderate amount of pericardial effusion (A and B). Right sided chambers were also enlarged and moderate mitral regurgitation was observed (C and D).

Fig. 4
The follow-up transthoracic echocardiography showed dilated left ventricular (LV) cavity (LV end-diastolic dimension = 56 mm) with low-normal LV function and small amount of pericardial effusion (A and B). Right sided chambers were still dilated and mitral regurgitation was reduced to mild degree (C and D).

References
1. Tang YD, Katz SD. The prevalence of anemia in chronic heart failure and its impact on the clinical outcomes. Heart Fail Rev. 2008; 13:387–392.
2. Anand IS. Anemia and chronic heart failure implications and treatment options. J Am Coll Cardiol. 2008; 52:501–511.
3. Mehta PA, Dubrey SW. High output heart failure. QJM. 2009; 102:235–241.
4. Cohen-Solal A, Leclercq C, Deray G, Lasocki S, Zambrowski JJ, Mebazaa A, de Groote P, Damy T, Galinier M. Iron deficiency: an emerging therapeutic target in heart failure. Heart. 2014; 100:1414–1420.
5. Anand IS, Chandrashekhar Y, Wander GS, Chawla LS. Endothelium-derived relaxing factor is important in mediating the high output state in chronic severe anemia. J Am Coll Cardiol. 1995; 25:1402–1407.
6. Hegde N, Rich MW, Gayomali C. The cardiomyopathy of iron deficiency. Tex Heart Inst J. 2006; 33:340–344.
7. Sohn IS, Jin ES, Cho JM, Kim CJ, Bae JH, Moon JY, Lee SH, Kim MJ. Bloodletting-induced cardiomyopathy: reversible cardiac hypertrophy in severe chronic anaemia from long-term bloodletting with cupping. Eur J Echocardiogr. 2008; 9:585–586.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download