Abstract
Background
Late complications after Fontan procedure may be due to the absence of pump and pulsatile pulmonary blood flow in this type of palliation. Our aim was to quantify the degree of pulsation by echocardiographic method in patients with extracardiac total cavopulmonary connection (ECTCPC) in comparison with biventricular circulation and few cases of pulsatile Fontan.
Methods
In a case series study, pulsatility index (PI) derived by echocardiographic method were compared between 20 patients with ECTCPC, 6 patients with pulsatile Fontan and 18 normal individual aged 4 to 20 years old. All patients were in New York Heart Association class of I and there was no report of complication.
Results
In patients with ECTCPC pulmonary artery branches Doppler flow study showed lower peak and mean velocities compared to the pulsatile Fontan and normal groups. ECTCPC patients had PI of 0.59 ± 0.14 and 0.59 ± 0.09 for right and left pulmonary arteries (RPA and LPA) respectively. PI was higher in patients with preserved antegrade flow (RPA PI = 0.94 ± 0.26, LPA PI = 0.98 ± 0.27) and in normal individuals (RPA PI = 1.59 ± 0.12, LPA PI = 1.64 ± 0.17) for both branches (p = 0.000).
A low pulmonary vascular resistance remains an important prognostic factor for an optimal functional result after the Fontan operation.1) Nonpulsatile characteristic of extracardiac total cavopulmonary connection (ECTCPC) may lead to an increase in pulmonary arterial pressure and vascular resistance.2) It has also been shown that leaving a pulsatile source of antegrade pulmonary blood flow after bidirectional cavopulmonary connection has potential benefit.3)4)5) Whether similar source of pulsatility could be beneficial for Fontan palliated patients has not been proved. Echocardiographic assessment of pulmonary blood flow for measurement of pulsatility will provide a noninvasive parameter for comparison and follow-up. Here, we report the result of an echocardiographic index of pulsatility in ECTCPC type of Fontan circulation in comparison with biventricular circulation and few cases of pulsatile Fontan.
Twenty one patients with fenestrated ECTCPC, 7 patients with pulsatile Fontan and 18 normal individuals were enrolled the study. Pulsatile Fontan group is composed of a limited group of patients with ECTCPC in our center that a restrictive antegrade flow through the main pulmonary artery has been preserved or adjusted. Patients were excluded if they were not in New York Heart Association (NYHA) class of I, had rhythm other than normal sinus rhythm or had any stenosis in Fontan pathway including pulmonary artery branch stenosis. Doppler flow pattern of both pulmonary arteries was studied and compared between three groups. Cross sectional echocardiography was used to establish the optimal plane for pulsed Doppler sampling of both pulmonary arteries flow. The optimal flow profiles in the right and left pulmonary arteries were obtained usually from the suprasternal view, about one vessel diameter distal to the superior vena cava anastomosis and pulmonary bifurcation respectively, angling the transducer until the best coaxial Doppler-blood flow intercept angle was achieved (Fig. 1). Getting the optimum Doppler flow profiles in Fontan circulation might be difficult especially in older patients and those with multiple previous palliative cardiac surgeries. However checking the apical 4 chamber, parasternal and supraclavicular views in addition to the suprasternal view for the best displayed signal will be helpful. The smallest sample volume, less than one third of the vessel diameter were selected to decrease the effect of translational motion on the signal recording. The traces were digitized using envelope tracing option to obtain the velocity-time integral for the maximum, minimum and mean velocities during a cardiac cycle according to the simultaneous electrocardiographic R-R interval. Pulsatility index (PI) was calculated according to the formula: PI = (maximum flow - minimum flow) / mean flow.6) Flow is equal to velocity times cross sectional area of the vessel. To decrease the operator dependent errors, we assumed that the vessel diameter was constant throughout the cardiac cycle. Hence by canceling the cross sectional area in the above formula we used (maximum velocity - minimum velocity) / mean velocity as the PI. The index was measured in the recordings obtained during quiet inspiration in supine patients. Statistical analysis was performed with SPSS software, version 16.0 (SPSS Inc., Chicago, IL, USA). The one-way analysis of variance (ANOVA) test was used for comparison of means between groups if normality assumption and homogeneity of variance are met. Otherwise Kruskal-Walis or Brown-Forsythe tests were used. After finding statistical significance of less than 0.05 in the ANOVA table tests, we used Tukey's post-hoc test to detect differences between the groups. A p-value of < 0.05 was considered significant. Informed consent was taken from the patients' parents. The research protocol was approved by the Institutional Ethics Review Committee of our center.
Twenty one patients (11 boys and 10 girls aged 4 to 20 years) who underwent ECTCPC palliation were enrolled into the study and compared with 7 patients (5 girls and 2 boys aged 5 to 20 years with mean of 2.2 years post operation) of pulsatile Fontan circulation and also with 18 normal individuals (11 boys and 7 girls 5 to 16 years with mean of 2.8 years post operation) (Table 1). Patient anatomic characteristics are summarized in Table 2. Except for one patient in the nonpulsatile ECTCPC group and one patient in the pulsatile group with ascites, pleural effusion and edema all patients were in NYHA class of I and there was no report of complication. Prolonged morbidity in the case palliated with pulsatile Fontan forced us to close the antegrade flow. Both cases were excluded from the study. All included patients had normal sinus rhythm, favorable systolic function as shown by fractional area change in Table 1 and competent atrioventricular valve. Those who had catheterization after Fontan operation (1 in pulsatile and 6 in nonpulsatile group) had pulmonary vascular resistance of less than 3 wood units and mean of pulmonary artery pressure of less than 15 mm Hg. Table 3 shows in detail the Doppler flow velocities and PIs of pulmonary artery branches in our patient groups and normal individual. In patients with nonpulsatile Fontan circulation, pulmonary artery branches Doppler flow study showed lower peak and mean velocities compared to the pulsatile and normal groups. No significant differences were seen in the minimum velocities except for the normal cohort that were reached to the baseline. In patients with persistent antegrade flow, Doppler flow study showed higher peak velocities and augmentation of the systolic forward flow compared to the patients palliated with nonpulsatile Fontan (Fig. 2). Furthermore, the mean of PI for both pulmonary artery branches was higher in the normal group and patients with maintained antegrade flow compared to the nonpulsatile patients: 1.59-1.64 and 0.94-0.98 vs. 0.59 (Table 3). Although systemic venous PIs were lower in the ECTCPC group compared to the normal individual (0.58-0.64 vs. 0.82-1.02), it did not show significant differences with the pulsatile group (0.66-0.72).
The effect and importance of pulsatile flow in both global and microvascular pulmonary circulation has been investigated in several experimental studies.7)8)9)10) It has been proposed that pulsatile flow may reduce pulmonary vascular resistance11)12) and promote the growth of pulmonary artery over time.2) Literature review shows that pulsatility in cavopulmonary connection has been measured with invasive and noninvasive methods. 6)7)13)14) Kurotobi et al.7) by using an invasive Doppler flow wire measured the PI as peak systolic flow velocity divided by the diastolic velocity nadir. Others used the magnetic resonance technique for assessment of pulsatility in different types of Fontan palliation. They defined PI as the maximum flow rate minus the minimum flow rate divided by the mean flow rate.6)13) We used the latter formula, however using Doppler echocardiography instead, for the measurement of PI in our patients with cavopulmonary connection.
In normal physiology, the pulmonary artery curve has an upsurge after the systolic upraise of right ventricle which is simultaneous with aortic pressure. In patients with ECTCPC there is no systolic surge in the pulmonary artery tracing. Late in the diastole there is an acceleration of flow in the pulmonary artery, however not as prominent as the systolic upstroke in normal pulmonary artery curve. This acceleration is related to the passive flow enhanced by a suctioning systemic ventricle.15) Our patients with ECTCPC showed lower peak and mean velocities in the pulmonary artery branches and had the least PI about 0.6 that was 37% of normal PI. The nadir velocities were similar to the pulsatile group. It did not reach to the baseline compared to the normal group. In contrast our patients with pulsatile Fontan showed an augmented systolic forward flow with higher PI about 1.0 (67% of normal PI) that makes it more similar to the normal physiologic pattern of pulmonary blood flow. The systemic venous PI (superior vena cava and inferior vena cava) was low in both groups of pulsatile and nonpulsatile Fontan.
Type of palliation in Fontan circulation has an impact on the degree of pulsation. It has been shown that atriopulmonary connection has the greatest PI, however with more loss of energy and progressive right atrial enlargement.14) Some pulsatility is persevered in the form of lateral tunnel palliation because of contraction in the remaining part of atrial musculature.13) The least pulsation in the ECTCPC is a drawback for this type of Fontan palliation.
Recently we showed in a computational fluid dynamics simulation that keeping the antegrade flow increases PI in both pulmonary artery branches however at the expense of energy loss in the total cavopulmonary connection region.16) Although flow Doppler study of pulmonary artery in patients with pulsatile Fontan may resemble more to the normal physiology, long term outcome of this modification need to be seen. Because of the limited sample volume and the short period of follow up in this study we did not focus on the clinical impact of pulsatility on the long term fate of Fontan palliated patients such as protein losing enteropathy, elevation of pulmonary vascular resistance and prolonged pleural effusion.
We also had some limitations in obtaining the optimal echocardiographic views due to the previous surgery, alignment of the sample volume across the pulmonary artery branches and the effect of respiratory translational motion on the signal recording. Using only transducer angulation in an effort to achieve a coaxial Doppler-blood flow intercept angle means that only underestimation can occur. Moreover we were obliged to make a number of approximations to the real total cavopulmonary connection fluid dynamics to allow for simple calculation. If flow is pulsatile (implying variations in the pressure difference driving flow), then one would anticipate vessel pulsations, with expansion when distending pressure was higher, and recoil when distending pressure was lower. Hence the cross sectional area of the vessel is not constant when flow is pulsatile. We wonder how much the assumption that pulmonary arterial cross-sectional area is constant in our patients with pulsatile flow is confounding.
Despite of the aforementioned limitations, Doppler echocardiography could be considered as a decisive technique for measurement of pulmonary artery pulsation in Fontan palliated population. Noninvasive characteristic and easier access are the advantages of this technique in the assessment of pulsatility. However a larger number of patients and longer follow up time to validate our conclusion deems to be in order. Moreover an assessment of test-retest reproducibility seems to be necessary.
Figures and Tables
Fig. 1
Schematic illustration for the position of sample volume and angling the transducer for getting the optimal flow profiles in the RPA and LPA. The arrow shows the pulsatile flow in cases of pulsatile Fontan group. RPA: right pulmonary arteries, LPA: left pulmonary arteries.
Fig. 2
Doppler flow pattern of pulmonary artery in a patient with extracardiac total cavopulmonary connection Fontan (A), pulsatile Fontan (B), and a healthy child (C). Compared to the nonpulsatile Fontan, patients with maintained antegrade flow showed higher velocity and pulsatility index (PI) with augmented forward systolic pulmonary flow. The arrows show the maximum (Max) and minimum (Min) velocities. PI was calculated according to the formula: PI = (Max velocity - Min velocity) / mean velocity. The measured PIs were 0.5, 1.02, and 1.78, respectively.

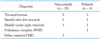
Table 3
Doppler flow velocities and pulsatility indices of pulmonary artery branches and systemic veins in patients with ECTCPC, pulsatile Fontan and normal groups

p values are between ECTCPC and pulsatile Fontan group. *Significant difference between all groups, †Significant difference between the normal and pulsatile Fontan groups, ‡No significant difference between the patients groups. IVC: inferior vena cava, LPA: left pulmonary artery, LSVC: left-sided superior vena cava, PI: pulsatility index, QI: quiet inspiration, RPA: right pulmonary artery, RSVC: right-sided superior vena cava, V: velocity, VTI: velocity-time integral, ECTCPC: extracardiac total cavopulmonary connection
References
1. Kaulitz R, Ziemer G, Luhmer I, Kallfelz HC. Modified Fontan operation in functionally univentricular hearts: preoperative risk factors and intermediate results. J Thorac Cardiovasc Surg. 1996; 112:658–664.
2. Ovroutski S, Ewert P, Alexi-Meskishvili V, Hölscher K, Miera O, Peters B, Hetzer R, Berger F. Absence of pulmonary artery growth after Fontan operation and its possible impact on late outcome. Ann Thorac Surg. 2009; 87:826–831.
3. Yoshida M, Yamaguchi M, Yoshimura N, Murakami H, Matsuhisa H, Okita Y. Appropriate additional pulmonary blood flow at the bidirectional Glenn procedure is useful for completion of total cavopulmonary connection. Ann Thorac Surg. 2005; 80:976–981.
4. Gray RG, Altmann K, Mosca RS, Prakash A, Williams IA, Quaegebeur JM, Chen JM. Persistent antegrade pulmonary blood flow post-Glenn does not alter early post-Fontan outcomes in single-ventricle patients. Ann Thorac Surg. 2007; 84:888–893. discussion 893.
5. Berdat PA, Belli E, Lacour-Gayet F, Planché C, Serraf A. Additional pulmonary blood flow has no adverse effect on outcome after bidirectional cavopulmonary anastomosis. Ann Thorac Surg. 2005; 79:29–36. discussion 36-7.
6. Klimes K, Abdul-Khaliq H, Ovroutski S, Hui W, Alexi-Meskishvili V, Spors B, Hetzer R, Felix R, Lange PE, Berger F, Gutberlet M. Pulmonary and caval blood flow patterns in patients with intracardiac and extracardiac Fontan: a magnetic resonance study. Clin Res Cardiol. 2007; 96:160–167.
7. Kurotobi S, Sano T, Kogaki S, Matsushita T, Miwatani T, Takeuchi M, Matsuda H, Okada S. Bidirectional cavopulmonary shunt with right ventricular outflow patency: the impact of pulsatility on pulmonary endothelial function. J Thorac Cardiovasc Surg. 2001; 121:1161–1168.
8. Tamaki S, Kawazoe K, Yagihara T, Abe T. A model to simulate the haemodynamic effects of right heart pulsatile flow after modified Fontan procedure. Br Heart J. 1992; 67:177–179.
9. Myers CD, Boyd JH, Presson RG Jr, Vijay P, Coats AC, Brown JW, Rodefeld MD. Neonatal cavopulmonary assist: pulsatile versus steady-flow pulmonary perfusion. Ann Thorac Surg. 2006; 81:257–263.
10. Sakaki M, Taenaka Y, Tatsumi E, Nakatani T, Takano H. Influences of nonpulsatile pulmonary flow on pulmonary function. Evaluation in a chronic animal model. J Thorac Cardiovasc Surg. 1994; 108:495–502.
11. Raj JU, Kaapa P, Anderson J. Effect of pulsatile flow on microvascular resistance in adult rabbit lungs. J Appl Physiol (1985). 1992; 72:73–81.
12. Presson RG Jr, Baumgartner WA Jr, Peterson AJ, Glenny RW, Wagner WW Jr. Pulmonary capillaries are recruited during pulsatile flow. J Appl Physiol (1985). 2002; 92:1183–1190.
13. Houlind K, Stenbøg EV, Sørensen KE, Emmertsen K, Hansen OK, Rybro L, Hjortdal VE. Pulmonary and caval flow dynamics after total cavopulmonary connection. Heart. 1999; 81:67–72.
14. Kaulitz R, Bergman P, Luhmer I, Paul T, Hausdorf G. Instantaneous pressure-flow velocity relations of systemic venous return in patients with univentricular circulation. Heart. 1999; 82:294–299.
15. Hager A, Fratz S, Schwaiger M, Lange R, Hess J, Stern H. Pulmonary blood flow patterns in patients with Fontan circulation. Ann Thorac Surg. 2008; 85:186–191.
16. Ghoreyshi M, Saidi MS, Navabi MA, Firoozabadi BD, Shabanian R. Numerical investigation of antegrade flow effects on flow pulsations in Fontan operation. Int J Biomed Eng Technol. 2012; 10:221–238.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download