Abstract
Leaflet escape of prosthetic valve is rare but potentially life threatening. It is essential to make timely diagnosis in order to avoid mortality. Transesophageal echocardiography and cinefluoroscopy is usually diagnostic and the location of the missing leaflet can be identified by computed tomography (CT). Emergent surgical correction is mandatory. We report a case of fractured escape of Edward-Duromedics mitral valve 27 years after the surgery. The patient presented with symptoms of acute decompensated heart failure and cardiogenic shock. She was instantly intubated and mechanically ventilated. After prompt evaluation including transthoracic echocardiography and CT, the escape of the leaflet was confirmed. The patient underwent emergent surgery for replacement of the damaged prosthetic valves immediately. Eleven days after the surgery, the dislodged leaflet in iliac artery was removed safely and the patient recovered well.
Possible causes of mechanical prosthetic valve dysfunctions include obstruction due to valvular thrombosis or pannus formation or regurgitation of valvular or paravalvular origin. In case of regurgitation, major concern is paravalvular leakage, because mechanical prosthetic valves are proven to be durable and valvular regurgitation due to structural valve deterioration is extremely rare. However, once it happens, it can be potentially life threatening. We report a sudden leaflet dislocation of a Edward-Duromedics mitral valve (Baxter Healthcare Corp., Cleveland, MS, USA) corrected by the prompt diagnosis followed by an emergency operation.
A 72-year-old woman visited emergency department as she suddenly experienced chest pain with resting dyspnea [New York Heart Association (NYHA) functional class IV] while washing dishes at home. She underwent mitral valve replacement 27 years ago, at the age of 45, due to mitral stenosis. Mitral valve replacement was done with Edwards-Duromedics 29 mm mitral valve (Baxter Healthcare Corp., Cleveland, MS, USA). Apart from valvular heart disease, the patient was on medication for diabetes mellitus and hypertension as well as paroxysmal atrial fibrillation. She remained to be the status of NYHA functional class II and anticoagulation with coumadin was appropriately done (international normalized ratio 2-2.5). The recent transthoracic echocardiography (TTE) done 4 month ago confirmed normal left ventricular systolic function [ejection fraction (EF): 69%] and well functioning of prosthetic mitral valve with mild pulmonary hypertension [right ventricle systolic pressure (RVSP) = 35 mmHg] and mild tricuspid regurgitation. On physical examination, she was acutely ill looking, diaphoretic and tachypneic. Her vital signs were as follows; blood pressure 69/51 mmHg, pulse rate 130/min, body temperature 36.7 with respiratory rate 35 breath/min. Her jugular vein was prominently engorged. On auscultation, audible mitral valve click with grade 4/6 pansystolic murmur was noted. Her electrocardiogram showed atrial fibrillation with rate of 130-140 beats/min. Chest X-ray revealed acute pulmonary edema with aggravated cardiomegaly (Fig. 1). Complete blood count showed white blood cell count of 9820/µL, hemoglobin of 9.8 g/dL, and platelet of 386000/µL. Other labs showed elevated creatinine (1.12 mg/dL, estimated glomerular filtration rate 50 mL/min/1.73) and slightly elevated cardiac enzymes (Creatine Kinase 555 IU/L, Creatine Kinase-MB 22.29 IU/L, Troponin T 0.016 ng/mL) with elevated N-terminal prohormone of brain natriuretic peptide level of 832 pg/mL. C-reactive protein level remained in normal range of 1.13 mg/L. Prothrombin time was 1.92. Arterial blood gas analysis showed oxygen pressure of 97 mmHg, carbon dioxide pressure of 27.4 mmHg, with pH of 7.353 with oxygen mask of 10 L.
After central line through right jugular vein was inserted, central venous pressure was 1 mmHg. Dobutamine and dopamine infusion were started 10 µg/kg/min respectively. The patient was intubated as she became intolerably tachypneic and progressively hypoxic.
To evaluate the cause of the shock and acute decompensated heart failure, bed side TTE was performed and revealed normal sized left ventricle (end diastolic dimension: 44 mm) and hyperdynamic left ventricular systolic function (EF: 80%) without regional wall motion abnormality. Moderate tricuspid regurgitation (Grade III) and severe pulmonary hypertension (right ventricular systolic pressure 75 mmHg) with plethora of inferior vena cava were demonstrated. On two-dimensional (2D) echocardiogram, there was suspicious finding of single prosthetic mitral leaflet, but details of the mitral leaflet morphology and Color Doppler were not sufficient for evaluating the prosthetic mitral valve function due to tachycardia and poor echo window. However, elevated mean diastolic pressure gradient (10 mmHg) across the prosthetic mitral valve without prolongation of pressure half time (54 ms) and low velocity of mitral regurgitation (MR, 4 m/s), and rapid declined in MR velocity suggested existence of severe MR (Fig. 2).
The diagnosis of acute severe MR due to escape of prosthetic valve leaflet with embolization was made and the patient immediately went through emergency operation to surgically correct dysfunctions of previously replaced mitral valve. The incision was made along the previous operation scar. When mitral valve was exposed, there was one leaflet missing without evidence of paravalvular dehiscence and pannus or thrombus formation (Fig. 3). The previous mechanical valve was removed and replaced with a 29 mm St. Jude Epic tissue valve (St. Jude Medical, St. Paul, MN, USA). After five hours of the surgery, her vital signs were stabilized. TTE after the surgery demonstrated well functioning bioprosthetic mitral valve with decreased tricuspid regurgitation (Grade I) and resolution of pulmonary hypertension (RVSP 39 mmHg).
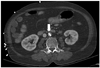
In an attempt to localize the missing leaflet, computed tomography (CT) was done, and a plate like metallic density in infra-renal abdominal aorta was noted (Fig. 4). The remaining fragment of leaflet in infra renal abdominal artery was removed 11 days after bioprosthetic valve replacement. It was placed 2 cm above common iliac artery bifurcation. The abdominal aorta was vertically dissected 7 cm, and the fragment was safely removed (Fig. 5). The patient developed mild fever after the surgery but recovered well and was discharged 37 days after the surgery.
One of the main concerns for prosthetic valve is its durability for lifelong time. Leaflet escape of bi-leaflet mechanical prosthesis has been reported (Tekna and Duromedics) to be extremely rare.1-5)
The leaflet escape is reported to happen more frequently in mitral than aortic positions. A few factors have been reported to account for material deterioration.6) The cavitation, which is the rapid formation of vaporous microbubbles in a fluid by a local reduction of pressure below the vapor pressure7) is recognized as the most contributing factor to the series of valve failure in Edward-Duromedics prosthesis. The damages by cavitation may lead to pitting and microcracking. Other factors identified are asymmetric closure with local stresses, inadequate compliance of calcified sewing ring, clustered microporosity of the pyrolytic carbon and surgical mishandling.6) The time of leaflet escape varies from 19 days6) to 12 years8) after the implantation of the mitral valve.
The clinical presentation is usually acute pulmonary edema with cardiogenic shock as the result of acute valvular incompetence.1-5) Other causes of the clinical symptoms, such as myocardiac infarction, para-valvular leak, thrombosis of the prosthetic valves, malignant arrhythmia and pulmonary embolism should be considered.
TTE is usually not helpful for the diagnosed as it may be mis-interpretated as obstructed closure of the prosthetic valve, paravalvular leak or thrombosis.9) Transesophageal echocardiography (TEE) is diagnostic most of times. Cineflouroscopy may role as non invasive diagnostic tool to determine leaflet escape from valve thrombosis.9)10)
It is acknowledged that timely diagnosis and emergent surgical replacement of the prosthetic valve is most important.11) There are a few cases of mitral leaflet escape reported in Korea.12-14) As a patient deteriorates with symptoms of acute heart failure with unstable vital signs, in most of the reported cases, an emergent operation is performed with TTE finding of acute valvular dysfunction. Therefore, an exact diagnosis of leaflet escape is made during the surgery, except there was a case reported by Kim et al.13) which the diagnosis of a leaflet escape was made before an emergency operation by using fluoroscopy.
In our case, although the images of TTE were not sufficient for evaluating the exact mitral valve morphology and function, a single mitral leaflet was suspicious on 2D echocardiogram. In addition to the ambigious 2D images of single mitral leaflet, elevated mean diastolic pressure gradient with low velocity of mitral regurgitation, we could make diagnosis of acute severe MR by comprehensive interpretation of TTE without performing TEE. Intraop TEE finding confirmed our presumptions.
The location of the missing leaflet can be difficult to identify in case the leaflet embolized to distal aorta or its branches. CT is the best tool to locate the missing leaflet. Plain X-rays are not helpful because of lack of radio-opacity of the prosthetic valves. Removing dislocated leaflet is recommended as it may cause arterial wall damage leading to erosions, infections, and further migrations.
This case is notable that the patient who presented with severe cardiogenic shock after the prosthetic valve implanted 27 years ago suddenly dislodged, recovered from the debilitating condition owing to the prompt diagnosis based on TTE and immediate surgical correction. Although rare, when a patient with previous history of prosthetic valve replacement presents with symptoms of acute decompensated heart failure, possibility of leaflet and escape of the valve leaflet should be contemplated. In cases of the leaflet escape, the urgent diagnosis and emergent surgical replacement is mandatory to prevent the mortality.
Figures and Tables
Fig. 2
A: Apical four chamber zoom Doppler: no significant mitral regurgitant jet flow is demonstrated, however, mitral regurgitation is suspected despite poor echo window due to posterior acoustic shadowing and tachycardia. B: Continuous wave Doppler demonstrating pressure gradient across prosthetic mitral valve was elevated (mean diastolic pressure gradient 10 mmHg) without prolongation of pressure half time (54 ms). This finding favors regurgitation rather than obstruction. C: Continuous wave Doppler indicating low peak velocity and rapid decline in velocity in late systole, suggesting acute severe mitral regurgitation.

References
1. Deuvaert FE, Devriendt J, Massaut J, Van Nooten G, De Paepe J, Primo G. Leaflet escape of a mitral Duromedics prosthesis. Case report. Acta Chir Belg. 1989; 89:15–18.
2. Klepetko W, Moritz A, Mlczoch J, Schurawitzki H, Domanig E, Wolner E. Leaflet fracture in Edwards-Duromedics bileaflet valves. J Thorac Cardiovasc Surg. 1989; 97:90–94.

3. Alvarez J, Deal CW. Leaflet escape from a Duromedics valve. J Thorac Cardiovasc Surg. 1990; 99:372.

4. Kumar N, Balasundaram S, Rickard M, al Halees Z, Duran CM. Leaflet embolisation from Duromedics valves: a report of two cases. Thorac Cardiovasc Surg. 1991; 39:382–383.

5. Tatou E, Saleh M, Eicher C, Brenot R, David M. Fracture-embolization of duromedics valve prosthesis and microscopic uncommon lesions. Ann Thorac Surg. 2001; 71:1366–1369.

6. Baudet E, Roques X, McBride J, Panès F, Grimaud JP. A 8-year follow-up of the Edwards-Duromedics bileaflet prosthesis. J Cardiovasc Surg (Torino). 1995; 36:437–442.
7. Eichler MJ, Reul HM. Mechanical heart valve cavitation: valve specific parameters. Int J Artif Organs. 2004; 27:855–867.

8. Fragoulis S, Palatianos GM. Fractured prosthetic valve leaflet. Eur J Cardiothorac Surg. 2008; 34:907.

9. Devbhandari MP, Woo EB, Hooper TL. Long-term event-free survival with an embolised prosthetic valve leaflet in the thoracic aorta. J Cardiothorac Surg. 2008; 3:34.

10. Vogel W, Stoll HP, Bay W, Fröhlig G, Schieffer H. Cineradiography for determination of normal and abnormal function in mechanical heart valves. Am J Cardiol. 1993; 71:225–232.

11. Bottio T, Casarotto D, Thiene G, Caprili L, Angelini A, Gerosa G. Leaflet escape in a new bileaflet mechanical valve: TRI technologies. Circulation. 2003; 107:2303–2306.
12. Lee SY, Choi JB. Escape of mechanical valve: a case report. Korean J Thorac Cardiovasc Surg. 2007; 40:63–65.
13. Kim JH, Oh SS, Na CY, Baek MJ, Seo HJ, Kim CW. Leaflet escape of edwards duromedics mechanical heart valve: report of 1 case. Korean J Thorac Cardiovasc Surg. 2004; 37:373–375.
14. Youn YN, Yoo KJ. Valve leaflet escape of edwards duromedics mechanical valve. Korean J Thorac Cardiovasc Surg. 2002; 35:60–63.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download