Abstract
Background
To compare the effects of low dose and high dose of statin treatment on endothelial function and carotid intima-media thickness (IMT) in patients with variant angina (VAP).
Methods
A total of 70 patients with VAP were divided into two groups; atorvastatin 10 mg treatment group (group I: n = 35, 54.2 ± 12.5 years) versus atorvastatin 40 mg treatment group (group II: n = 35, 52.6 ± 9.8 years). Flow mediated vasodilation (FMD) of the brachial artery and IMT of the carotid artery were compared between the groups after 6 months of statin treatment.
Results
The baseline FMD and carotid IMT were not different between the groups. After 6 months of statin therapy, FMD was significantly improved in both groups (7.7 ± 2.5% to 8.9 ± 2.2% in group I, p = 0.001, 7.9 ± 2.7% to 9.5 ± 2.8% in group II, p < 0.001), but the degree of FMD change and FMD at 6 month were not different between the groups. Carotid IMT were not changed in both groups after 6 months of statin therapy.
Conclusion
The use of statin for 6 months significantly improved endothelial function in patients with VAP, but carotid IMT was not changed. The use of high dose statin did not show significant additional benefit as compared with the use of low dose statin. The present study suggested that statin therapy would be beneficial in the treatment of VAP.
In contrary to other typical types of coronary artery disease which are characterized by atherosclerotic narrowing of epicardial coronary artery, variant angina (VAP) is a disease characterized by generalized or focal significant coronary narrowing due to vasospasm.1) Endothelial dysfunction is known to be associated with vasospasm in patients with VAP2)3) and can be non-invasively measured by measuring flow mediated vasodilation (FMD) of the brachial artery.4)5) Intima-media thickness (IMT) of the carotid artery is an established surrogate marker of atherosclerosis, and the previous studies have shown that the increased carotid IMT is associated with the presence and severity of coronary artery disease. Because VAP is also associated with atherosclerotic process reflected by the presence of atheromatous plaque within coronary arteries,3)6) it is suggested that carotid IMT would be abnormal.
Statin, 3-hydroxy-3-methylglutaryl coenzyme A reductase inhibitor, is a potent lipid lowering agent, and it has been proved that the use of statin can reduce cardiovascular events in various cardiovascular diseases.7-10) These beneficial effects of statin is not only associated with the effects of lipid lowering, but also associated with the pleiotropic effects of statin including plaque stabilization, improvement of endothelial dysfunction, inhibition of platelet aggregation, and decrease of vascular inflammation.11-15) The use of statin can retard the progression or induce the regression of carotid atherosclerosis. Furthermore, the study of Yun et al.16) demonstrated that statin therapy could improve endothelial dysfunction in Korean patients with VAP. However, the impacts of statin dose on endothelial function and carotid IMT in Korean patients with VAP has been poorly evaluated.
Therefore, the aim of the present study was to compare the effects of low dose and high dose of statin therapy on endothelial function as measured by FMD of the brachial artery and IMT of the carotid artery in patients with VAP.
Among 296 patients who confirmed VAP based on typical symptoms or electrocardiographic changes accompanied by positive ergonovine stress test during coronary angiography from 2006 to 2009, a total of 70 patients who agreed to participate in the present study and gave informed consent were enrolled. The patients were divided into two groups with 1 to 1 fashion; atorvastatin 10 mg treatment group (group I: low dose group, n = 35, 54.2 ± 12.5 years, 16 males) versus atorvastatin 40 mg treatment group (group II: high dose group, n = 35, 52.6 ± 9.8 years, 17 males). The study protocol was approved by the Institutional Review Board of our institution and informed consent was obtained from each patient. Exclusion criteria included 1) prior history of coronary intervention or myocardial infarction, 2) significant arrhythmias including atrial fibrillation, 3) combined cardiac diseases including significant valvular heart diseases or cardiomyopathy or heart failure, 4) elevated cardiac enzymes, 5) systolic blood pressure ≥ 160 mmHg or diastolic blood pressure ≥ 100 mmHg, 6) known hepatic dysfunction or renal insufficiency, 7) vasculitis disorders, 8) prior use of statins, 9) major life threatening illness.
FMD of the brachial artery was measured according to the previously described recommendation as a non-invasive parameter of endothelial function.4) Baseline and follow-up FMD studies were done by single well trained registered diagnostic cardiac sonographer in early morning after an overnight fasting in all patients. Baseline FMD study was done before the use of statin, and follow-up FMD study was done after the discontinuation of statin for at least 24 hours. Vasoactive substances were also discontinued for at least 24 hours before FMD study. A 10 MHz high resolution linear vascular ultrasound transducer (Vivid 7, GE, Milwaukee, WI, USA) was used to image the brachial artery longitudinally just above the antecubital fossa. The tourniquet measuring blood pressure was placed on the forearm in order to create shear stress induced by reactive hyperemia. The diameter of the brachial artery was measured at the onset of the R-wave on electrocardiogram. After baseline measurements of the brachial artery diameter, the blood pressure cuff was inflated to at least 50 mmHg above systolic blood pressure to occlude arterial flow for 5 minutes. Subsequent deflation of the cuff induces a brief high flow state through the brachial artery (reactive hyperemia) to accommodate the dilated resistance vessels. The resulting increase in shear stress causes the brachial artery to dilate. The brachial artery was imaged for the first 2 minutes of reactive hyperemia continuously. The flow-mediated dilatory response was used as a measure of endothelium dependent vasodilation. After the 10 minutes of rest to reestablish baseline condition, 0.6 mg of nitroglycerin was administered sublingually. The brachial artery was imaged for 5 minutes continuously to measure peak diameter. The dilatory response to nitroglycerin was used as a measure of endothelium independent vasodilation.
A 10 MHz high resolution linear vascular ultrasound transducer (Vivid 7, GE, Milwaukee, WI, USA) was used to image carotid artery. Images were interpreted of the one last centimeters of the common carotid artery prior to the carotid bulb consisted first to describe the presence or absence of plaques of atheroma, defined as a focal widening relative to adjacent segments, protruding the lumen of more than 1.5 mm, with or without calcifications. On a longitudinal two-dimensional ultrasound image of the carotid artery, the anterior (near) and posterior (far) walls of the carotid artery appear as two bright white lines separated by a hypoechogenic space. End-diastolic images were frozen, and the far wall IMT was identified as the region between the lumen-intima interface and the media-adventitia interface. By using automatic border detection method, mean carotid IMT were measured at distal 1 cm of each common carotid artery, and the average value of right and left mean carotid IMT were used as the carotid IMT in the present study.
Diltiazem (Herben®, Seoul, Korea) was given in all patients 2 times in a day at the time of discharge, and nitrate was given at the physician's discretion. The patients were randomly assigned to either atorvastatin 10 mg or 40 mg group in 1 : 1 ratio, regardless of the cholesterol level. Angiotensin converting enzyme inhibitors or receptor blockers were not used to minimize the impacts on endothelial function of these drugs. Clinical and echocardiographic follow-up for 6 months was possible in all patients. FMD and carotid IMT were measured at 6 months after 24 hour cessation of vasoactive drugs including diltiazem and nitrate.
Statistical analysis was performed using commercially available software (SPSS for Windows, Version 19.0, IBM, Chicago, IL, USA). All parameters were expressed as the mean ± standard deviation. Categorical variables were evaluated using chi-square test. Differences in the mean values between the 2 groups were evaluated using unpaired t-test and changes in the mean values using paired t-test. Numerical correlations were established by a Pearson correlation. Intraobserver and interobserver variability for the repeated measurement of the brachial artery diameter and carotid IMT of our laboratory were described in the previous study of the authors.4) A p value of less than 0.05 was considered to be statistically significant.
Baseline clinical characteristics were summarized in the Table 1. Baseline characteristics including age, sex, risk factors, and prescribed medications were not different between the groups.
The changes of the lipid profiles were summarized in the Table 2. The levels of total cholesterol, low density lipoprotein (LDL)-cholesterol, and triglyceride were significantly reduced in both groups. The level of high density lipoprotein-cholesterol, however, was not changed significantly in both groups. The decrease of total cholesterol was significantly greater in group II than in group I, but the decrease of LDL-cholesterol was not significantly different between the groups (Fig. 1).
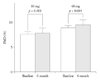
FMD of the brachial artery was 7.7 ± 2.5% in group I and 7.9 ± 2.7% in group II at baseline, and the baseline FMD was not different between the groups. After 6 months of statin therapy, FMD was significantly improved in both groups (from 7.7 ± 2.5% to 8.9 ± 2.2% in group I, p = 0.001, from 7.9 ± 2.7% to 9.5 ± 2.8% in group II, p < 0.001) (Fig. 2), but the FMD at 6 month and the degree of FMD change were not different between the groups.
Nitroglycerin-mediated dilation (NMD) of the brachial artery was 19.4 ± 5.2% in group I and 20.5 ± 5.5% in group II at baseline, and the baseline NMD was not different between the groups. After 6 months of statin therapy, NMD was not changed in both groups (from 19.4 ± 5.2% to 19.5 ± 4.9% in group I, from 20.5 ± 5.5% to 21.0 ± 5.4% in group II, p = ns).
Carotid IMT was 0.61 ± 0.06 mm in group I and 0.60 ± 0.06 mm in group II at baseline, and the baseline carotid IMT was not different between the groups. The carotid IMT was not changed in both groups despite of 6 months of statin therapy (from 0.61 ± 0.06 mm to 0.61 ± 0.06 mm in group I, from 0.60 ± 0.06 mm to 0.60 ± 0.06 mm in group II, p = ns).
Carotid plaque was identified 16 patients in group I and 18 patients in group II. The presence of carotid plaque was not different between the groups and was not changed after 6 months of statin therapy.
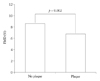
The brachial FMD did not show significant correlation with the carotid IMT (r = -0.189, p = ns). However, the FMD of the brachial artery was significantly decreased in patients with carotid plaque than in patients without carotid plaque (Fig. 3).
In the present study, the authors compared the effects of statin therapy (low dose vs. high dose) on endothelial function and carotid IMT in patients with VAP. The main finding of the present study was that the use of statin could improve endothelial function as measured by FMD of the brachial artery in patients with VAP. However, the additive role of high dose statin therapy on endothelial function as compared with low dose statin therapy and improvement of carotid IMT after statin therapy was not demonstrated in the present study. Considering the pathophysiologic mechanism of VAP, nevertheless, the result of the present study suggested that the use of statin, regardless of baseline lipid level, would be beneficial in the treatment of VAP.
Although long-term prognosis of the patients with VAP is generally known to be better than traditional angina pectoris or acute coronary syndromes caused by significant atherosclerotic coronary stenosis, the occurrence of cardiac death or myocardial infarction or disabling intractable spasm is not uncommon.17) Vasodilating agents including calcium channel blocker or nitrate has been a mainstay of treatment in patients with VAP to relieve of symptoms caused by coronary vasospasm. Because endothelial dysfunction plays an important role in the development of VAP,2)3) the drugs which improve endothelial dysfunction would be a reasonable therapeutic option in VAP. The previous studied have shown that angiotensin converting enzyme inhibitors or angiotensin receptor blockers can improve endothelial function in patients with coronary artery disease.18-20) It has also been proved that the use of statin is associated with the improvement of endothelial function in various cardiovascular diseases and diabetes.14)21-24) The study of Yun et al.,16) furthermore, demonstrated that 10 mg of rosuvastatin could improve endothelial function as assessed by FMD and endothelial progenitor cell counts in patients with VAP. The result of the present study was similar to the study of Yun et al.16) except for the type of the used statin. Both atorvastatin 10 mg and 40 mg could improve FMD after 6 months of therapy in the present study. The authors also want to investigate whether high dose statin therapy would have additive effects on endothelial function as compared with low dose, but in vain. Although the absolute value of FMD improvement of higher in high dose group than in low dose group, but it did not reach statistical significance. The reason why atorvastatin 40 mg did not show additive benefits on endothelial function as compared with low dose is unclear. One possible explanation is that 40 mg of atorvastatin is not sufficient to get additive beneficial effects on endothelial function, and thus further study using higher dose of atorvastatin such as 80 mg will be needed. The small number of the study population might also affect the result of statistical analysis, and thus further study with sufficient study population will be needed to elucidate this issue.
Carotid IMT and the presence of carotid plaque are well known surrogate markers of the presence of atherosclerotic cardiovascular disease or future cardiovascular events. The previous studies have demonstrated that conventional statin therapy can retard the progression of carotid atherosclerosis as assessed by carotid IMT, and aggressive lipid lowering by high dose statin therapy can reverse the progression of carotid IMT.25-28) Because VAP is also associated with atherosclerotic process reflected by the presence of atheromatous plaque within coronary arteries3)6) or increased carotid IMT, it is hypothesized that the use of high dose atorvastatin would have better effects on carotid IMT than in low dose atorvastatin. However, the carotid IMT was not changed despite of 6 months of atorvastatin either low dose or high dose in the present study. Because statin was used more than 2 years in most of the previous studies which showed favorable results on the progression of carotid atherosclerosis,25-28) relatively short duration of statin use would be a possible explanation for the negative results on carotid IMT progression in the present study. Based on these findings, it is suggested that statin should be used for sufficiently long duration to retard or regress the progression of atherosclerosis. The brachial FMD was significantly decreased in patients with carotid plaque than in patients without plaque in the present study. The brachial FMD was significantly decreased in patients with carotid plaque than in patients without plaque in the present study, the results of the present study also support the previous observations that endothelial dysfunction is associated with atherosclerosis and involves in every stages of the progression of atherosclerosis.29)30)
There are several limitations in the present study. Firstly, the main limitation of this study was the relatively small sample size which could affect the results of statistical analysis and the study was not performed in blinded fashion. Selection bias associated with small sample size could present inevitably, and thus the results of the present study cannot be generalized. Secondly, although the prescribed medications such as calcium channel blocker and nitrate were not different between the groups and discontinued 24 hour before follow-up echocardiographic study, these drugs also could affect diversely on the results of the brachial FMD. Thirdly, because the present study has no control group, the effect of diltiazem or nitrate on the improvement of FMD could not be completely excluded. Considering the previous study of Yun et al.16) which showed the use of statin significantly improves FMD regardless of the use of calcium channel blocker or nitrate, the use of statin would be a major factor for the improvement of FMD in the present study.
In conclusion, the use of statin improves endothelial function significantly in patients with VAP, but carotid IMT was not changed. Statin therapy would be beneficial in the treatment of VAP.
Figures and Tables
Fig. 1
Changes of the cholesterol level after 6 months of statin therapy.TC: total cholesterol, LDL-C: low density lipoprotein-cholesterol, 10 mg: atorvastatin 10 mg, 40 mg: atorvastatin 40 mg.
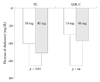
Fig. 2
Changes of the flow-mediated dilation (FMD) of the brachial artery after 6 months of statin therapy. 10 mg: atorvastatin 10 mg, 40 mg: atorvastatin 40 mg.
Acknowledgements
The present study was supported from the research grant of the Research Institute of Medical Sciences of Chonnam National University.
References
1. Yasue H, Nakagawa H, Itoh T, Harada E, Mizuno Y. Coronary artery spasm--clinical features, diagnosis, pathogenesis, and treatment. J Cardiol. 2008; 51:2–17.

2. Teragawa H, Kato M, Kurokawa J, Yamagata T, Matsuura H, Chayama K. Endothelial dysfunction is an independent factor responsible for vasospastic angina. Clin Sci (Lond). 2001; 101:707–713.

3. Cho SH, Jeong MH, Park IH, Choi JS, Yoon HJ, Kim KH, Hong YJ, Park HW, Kim JH, Ahn Y, Cho JG, Park JC, Kang JC. Endothelial dysfunction, increased carotid artery intima-media thickness and pulse wave velocity, and increased level of inflammatory markers are associated with variant angina. J Cardiol. 2009; 54:183–191.

4. Corretti MC, Anderson TJ, Benjamin EJ, Celermajer D, Charbonneau F, Creager MA, Deanfield J, Drexler H, Gerhard-Herman M, Herrington D, Vallance P, Vita J, Vogel R. International Brachial Artery Reactivity Task Force. Guidelines for the ultrasound assessment of endothelial-dependent flow-mediated vasodilation of the brachial artery: a report of the International Brachial Artery Reactivity Task Force. J Am Coll Cardiol. 2002; 39:257–265.

5. Nam CW, Kim GS, Lee SJ, Lee IG. Evaluation of endothelial function using high-resolution ultrasound in normal subjects: endothelial function according to aging. J Korean Soc Echocardiogr. 2000; 8:71–77.

6. Yamagishi M, Miyatake K, Tamai J, Nakatani S, Koyama J, Nissen SE. Intravascular ultrasound detection of atherosclerosis at the site of focal vasospasm in angiographically normal or minimally narrowed coronary segments. J Am Coll Cardiol. 1994; 23:352–357.

7. Randomised trial of cholesterol lowering in 4444 patients with coronary heart disease: the Scandinavian Simvastatin Survival Study (4S). Lancet. 1994; 344:1383–1389.
8. Downs JR, Clearfield M, Weis S, Whitney E, Shapiro DR, Beere PA, Langendorfer A, Stein EA, Kruyer W, Gotto AM Jr. Primary prevention of acute coronary events with lovastatin in men and women with average cholesterol levels: results of AFCAPS/TexCAPS. Air Force/Texas Coronary Atherosclerosis Prevention Study. JAMA. 1998; 279:1615–1622.

9. The Long-Term Intervention with Pravastatin in Ischaemic Disease (LIPID) Study Group. Prevention of cardiovascular events and death with pravastatin in patients with coronary heart disease and a broad range of initial cholesterol levels. N Engl J Med. 1998; 339:1349–1357.
10. Heart Protection Study Collaborative Group. MRC/BHF Heart Protection Study of cholesterol lowering with simvastatin in 20,536 high-risk individuals: a randomised placebo-controlled trial. Lancet. 2002; 360:7–22.
11. Merten M, Dong JF, Lopez JA, Thiagarajan P. Cholesterol sulfate: a new adhesive molecule for platelets. Circulation. 2001; 103:2032–2034.
12. Lacoste L, Lam JY, Hung J, Letchacovski G, Solymoss CB, Waters D. Hyperlipidemia and coronary disease. Correction of the increased thrombogenic potential with cholesterol reduction. Circulation. 1995; 92:3172–3177.
13. Ridker PM, Rifai N, Pfeffer MA, Sacks FM, Moye LA, Goldman S, Flaker GC, Braunwald E. Cholesterol and Recurrent Events (CARE) Investigators. Inflammation, pravastatin, and the risk of coronary events after myocardial infarction in patients with average cholesterol levels. Circulation. 1998; 98:839–844.

14. Dupuis J, Tardif JC, Cernacek P, Théroux P. Cholesterol reduction rapidly improves endothelial function after acute coronary syndromes. The RECIFE (reduction of cholesterol in ischemia and function of the endothelium) trial. Circulation. 1999; 99:3227–3233.

15. Strandberg TE, Vanhanen H, Tikkanen MJ. Effect of statins on C-reactive protein in patients with coronary artery disease. Lancet. 1999; 353:118–119.

16. Yun KH, Shin IS, Park EM, Rhee SJ, Lee EM, Yoo NJ, Kim NH, Oh SK, Jeong JW. Effect of additional statin therapy on endothelial function and prognosis in patients with vasospastic angina. Korean Circ J. 2008; 38:638–643.

17. Walling A, Waters DD, Miller DD, Roy D, Pelletier GB, Théroux P. Long-term prognosis of patients with variant angina. Circulation. 1987; 76:990–997.

18. Mancini GB, Henry GC, Macaya C, O'Neill BJ, Pucillo AL, Carere RG, Wargovich TJ, Mudra H, Lüscher TF, Klibaner MI, Haber HE, Uprichard AC, Pepine CJ, Pitt B. Angiotensin-converting enzyme inhibition with quinapril improves endothelial vasomotor dysfunction in patients with coronary artery disease. The TREND (Trial on Reversing ENdothelial Dysfunction) Study. Circulation. 1996; 94:258–265.

19. Anderson TJ, Elstein E, Haber H, Charbonneau F. Comparative study of ACE-inhibition, angiotensin II antagonism, and calcium channel blockade on flow-mediated vasodilation in patients with coronary disease (BANFF study). J Am Coll Cardiol. 2000; 35:60–66.

20. Kim KH, Jeong MH, Cho SH, Moon JY, Hong YJ, Park HW, Kim JH, Ahn Y, Cho JG, Park JC, Kang JC. Clinical effects of calcium channel blocker and Angiotensin converting enzyme inhibitor on endothelial function and arterial stiffness in patients with angina pectoris. J Korean Med Sci. 2009; 24:223–231.

21. Lee YS, Kim KS. The short-term effect of atorvastatin on flow-mediated vasodilation, pulse wave velocity and carotid intima-media thickness in patients with moderate cholesterolemia. Korean Circ J. 2008; 38:144–151.

22. Reriani MK, Dunlay SM, Gupta B, West CP, Rihal CS, Lerman LO, Lerman A. Effects of statins on coronary and peripheral endothelial function in humans: a systematic review and meta-analysis of randomized controlled trials. Eur J Cardiovasc Prev Rehabil. 2011; 18:704–716.

23. Liu B, Zhang JY, Cao HM, Wang Q, Wang HB. Effect of rosuvastatin on ROCK activity, endothelial function, and inflammation in Asian patients with atherosclerosis. Intern Med. 2012; 51:1177–1182.

24. Zhang L, Gong D, Li S, Zhou X. Meta-analysis of the effects of statin therapy on endothelial function in patients with diabetes mellitus. Atherosclerosis. 2012; 223:78–85.

25. Ubels FL, Muntinga JH, van Doormaal JJ, Reitsma WD, Smit AJ. Effects of initial and long-term lipid-lowering therapy on vascular wall characteristics. Atherosclerosis. 2001; 154:155–161.

26. Kastelein JJ, Wiegman A, de Groot E. Surrogate markers of atherosclerosis: impact of statins. Atheroscler Suppl. 2003; 4:31–36.

27. Kang S, Wu Y, Li X. Effects of statin therapy on the progression of carotid atherosclerosis: a systematic review and meta-analysis. Atherosclerosis. 2004; 177:433–442.

28. Kastelein JJ, de Groot E, Sankatsing R. Atherosclerosis measured by B-mode ultrasonography: effect of statin therapy on disease progression. Am J Med. 2004; 116:Suppl 6A. 31S–36S.





 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download