1. Faggiano P, Antonini-Canterin F, Baldessin F, Lorusso R, D'Aloia A, Cas LD. Epidemiology and cardiovascular risk factors of aortic stenosis. Cardiovasc Ultrasound. 2006; 4:27. PMID:
16813661.
2. Lindroos M, Kupari M, Heikkilä J, Tilvis R. Prevalence of aortic valve abnormalities in the elderly: an echocardiographic study of a random population sample. J Am Coll Cardiol. 1993; 21:1220–1225. PMID:
8459080.
3. Chambers J. Can high blood pressure mask severe aortic stenosis? J Heart Valve Dis. 1999; 8:277–278. PMID:
10399660.
4. Hachicha Z, Dumesnil JG, Bogaty P, Pibarot P. Paradoxical low-flow, low-gradient severe aortic stenosis despite preserved ejection fraction is associated with higher afterload and reduced survival. Circulation. 2007; 115:2856–2864. PMID:
17533183.
5. Antonini-Canterin F, Huang G, Cervesato E, Faggiano P, Pavan D, Piazza R, Nicolosi GL. Symptomatic aortic stenosis: does systemic hypertension play an additional role? Hypertension. 2003; 41:1268–1272. PMID:
12707297.
6. Park HE, Chang SA, Kim HK, Shin DH, Kim JH, Seo MK, Kim YJ, Cho GY, Sohn DW, Oh BH, Park YB. Impact of loading condition on the 2D speckle tracking-derived left ventricular dyssynchrony index in nonischemic dilated cardiomyopathy. Circ Cardiovasc Imaging. 2010; 3:272–281. PMID:
20190282.
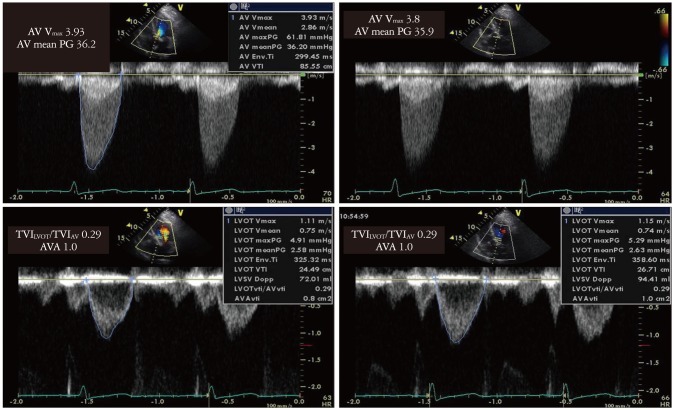
7. Otto CM, Pearlman AS, Comess KA, Reamer RP, Janko CL, Huntsman LL. Determination of the stenotic aortic valve area in adults using Doppler echocardiography. J Am Coll Cardiol. 1986; 7:509–517. PMID:
3950230.
8. Ihlen H, Amlie JP, Dale J, Forfang K, Nitter-Hauge S, Otterstad JE, Simonsen S, Myhre E. Determination of cardiac output by Doppler echocardiography. Br Heart J. 1984; 51:54–60. PMID:
6689921.
9. Mascherbauer J, Fuchs C, Stoiber M, Schima H, Pernicka E, Maurer G, Baumgartner H. Systemic pressure does not directly affect pressure gradient and valve area estimates in aortic stenosis in vitro. Eur Heart J. 2008; 29:2049–2057. PMID:
18502739.
10. Thubrikar M, Bosher LP, Nolan SP. The mechanism of opening of the aortic valve. J Thorac Cardiovasc Surg. 1979; 77:863–870. PMID:
439922.
11. Higashidate M, Tamiya K, Beppu T, Imai Y. Regulation of the aortic valve opening. In vivo dynamic measurement of aortic valve orifice area. J Thorac Cardiovasc Surg. 1995; 110:496–503. PMID:
7637367.
12. Little SH, Chan KL, Burwash IG. Impact of blood pressure on the Doppler echocardiographic assessment of severity of aortic stenosis. Heart. 2007; 93:848–855. PMID:
17135222.
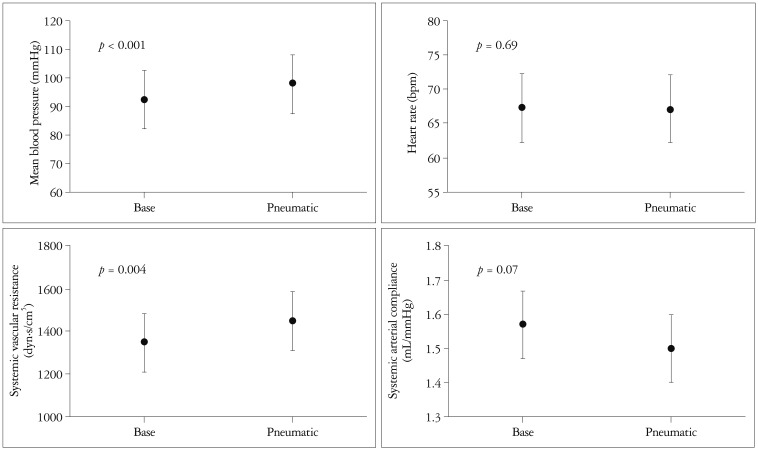
13. Rubal BJ, Geer MR, Bickell WH. Effects of pneumatic antishock garment inflation in normovolemic subjects. J Appl Physiol. 1989; 67:339–345. PMID:
2759962.
14. Abbas AE, Fortuin FD, Patel B, Moreno CA, Schiller NB, Lester SJ. Noninvasive measurement of systemic vascular resistance using Doppler echocardiography. J Am Soc Echocardiogr. 2004; 17:834–838. PMID:
15282486.
15. Chemla D, Hébert JL, Coirault C, Zamani K, Suard I, Colin P, Lecarpentier Y. Total arterial compliance estimated by stroke volume-to-aortic pulse pressure ratio in humans. Am J Physiol. 1998; 274(2 Pt 2):H500–H505. PMID:
9486253.