Abstract
Preservation of the subvalvular apparatus has the merits of postoperative outcomes during mitral valve replacement for mitral regurgitation. We performed mitral valve replacement with anterior and posterior leaflet chordal preservation in a 65-year-old woman. On the 2nd postoperative day, routine postoperative trans-thoracic echocardiography showed an unknown aortic subvalvular mobile mass. We report a case of a remnant mitral subvalvular apparatus detected by echocardiography after chordal preserving mitral valve replacement which was confused with postoperative aortic valve vegetation.
A recent epidemiological study showed that the incidence of mitral regurgitation (MR) has been increasing.1) In addition, the prognosis of severe MR is known to be very poor2) and the only treatment modality is surgical correction.3) As the conventional mitral valve replacement (MVR) might cause loss of annulo-ventricular continuity, chordal preserving MVR is recently most common method for the patients who require mitral valve (MV) surgery.4)5) However, there are some disadvantages of leaving the subvalvular apparatus intact during MVR like confusion chordal remnants with valve vegetation or thrombus and left ventricular outflow tract obstruction. Here, we report a case of a remnant mitral subvalvular apparatus detected after chordal preserving MVR, which was confused with postoperative
aortic valve vegetation.
A 64-year-old woman was admitted to the hospital due to heart with progressive dyspnea. Preoperative trans-esophageal echocardiography revealed severe MR and mitral leaflet prolapsed (Fig. 1, Supplementary movie 1, 2). The degree of aortic regurgitation and tricuspid regurgitation were trivial. End-diastolic diameter was 69 mm, end-systolic diameter was 48 mm and estimated ejection fraction was 56%. Estimated systolic pulmonary artery pressure from tricuspid regurgitation was 47 mmHg. There was no intra-cardiac mass, thrombi or pericardial effusion. Coronary catheterization revealed normal coronary arteries. Her past medical history included hypercholesterolemia and hypertension. Five years ago, there was no proven arrhythmia, but atrial fibrillation was newly detected on the day of this admission. Laboratory examinations were as follows: hemoglobin, 14.2 g/dL; glucose, 100 mg/dL; urea, 17 mg/dL; creatinine, 0.9 mg/dL; serum cholesterol, 117 mg/dL; triglycerides, 171 mg/dL; Pro-BNP, 2381 pg/mL and thyroid function was within normal range. The patient underwent MV repair with annuloplasty and maze operation.6) However, the intraoperative trans-esophageal echocardiography performed at the end of the procedure revealed remained moderate MR. We decided to convert MV repair to MVR with a 29-mm bileaflet mechanical prosthesis. During MVR, anterior and posterior leaflet chordae were preserved and reaffixed to the mitral ring near the both commissures as Okita et al.7) had introduced. The central portion of the anterior mitral valve leaflet, which was not supported by chordae, was excised and the remnant anterior leaflet was divided into anterior and posterior. The divided segments were shifted and reattached to the mitral ring of the respective commissural areas and then the prosthetic valve was implanted; the ventricular side of the remnant leaflet was in contact with the prosthetic sewing ring. After completion of the valve replacement, the patient's hemodynamic condition was stable. Routine trans-thoracic echocardiography (TTE) performed on the 2nd postoperative day showed a normal functioning mitral prosthesis and slightly decreased ventricular function. However, TTE showed an abnormal aortic valve mass which had not been found in any previous examination (size: 0.3 × 0.6 cm by TTE) (Fig. 2, Supplementary movie 3, 4). Since infective endocarditis and aortic valve vegetation could not be ruled out, empirical intravenous administration of antibiotics (vancomycin and ceftriaxone) were started. Even though, she had not shown any symptoms of infective endocarditis, we performed serial TTE examinations and blood cultures for 2 weeks. Fig. 3 and Supplementary movie 5-8. showed serial TTE from the day before surgery to postoperative 21st day. Reevaluation on the 7th and the 14th postoperative day with TTE showed a normal functioning mitral prosthesis and no significant change in mass size around the aortic valve. The mobile mass was hanging at the continuous margin of the mechanical valve and it had high echogenicity rather than low echogenicity which is a typical finding of acute vegetation. That area revealed very high pressure below the aortic valve and moved along in the cardiac cycle. There were no microorganisms growing in serial blood cultures and postoperative white blood cell counts decreased from 22720/µL on 2nd postoperative day to 11500/µL on 8th postoperative day, and then 3910/µL on 14th postoperative day. The inflammation marker, C-reactive protein also decreased from 5.76 mg/dL on the day of surgery to 2.37 mg/dL on the 14th postoperative day. Judging from the serial echocardiographic and clinical findings, the subaortic valve mass was finally defined as not the vegetation but the remnant mitral subvalvular apparatus which was attached to the anterior leaflet segment, sandwiched between the mitral annulus and the sewing ring of the mechanical valve. The remnant mitral subvalvular apparatus adrift was thought to be composed of separated papillary muscle tip and its subjected chordae. The TTE appearance of the functioning prosthesis 21 days after surgery was good, and left ventricular function improved slightly (visually 45-50%).
Severe MR is associated with significant morbidity and mortality. Mitral valve repair (MVRe) or MVR is recommended for symptomatic patients with or without signs of left ventricular dysfunction, and in asymptomatic patients with left ventricular enlargement, systolic dysfunction, pulmonary hypertension, or new atrial fibrillation. MVRe may offer survival benefit over MVR and should be considered the procedure of choice for patients who require intervention. However, the patients require MVR when repair is not feasible. Intra-operative trans-esophageal echocardiography plays an important in surgical intervention for MR, in the aspect of decision to progress valve replacement.
Following conventional MVR, we are concerned about loss of annulo-ventricular continuity and preservation of left ventricular function, thus favoring an operative technique for MVR with preservation of the chordae tendineae. This operative technique improves cardiac index, left ventricular end-systolic volume index and left ventricular ejection fraction.7) In addition, it has the merits of reduction of operative mortality and ventricular rupture as well as improves early and long term survival.8) However, possible disadvantages of leaving the subvalvular apparatus intact during MVR are left ventricular outflow tract obstruction3) and prosthetic leaflet immobilization. There have been also reports of disc or poppet entrapment by surgically divided chordal remnants, long suture ends, or overhanging knots.2) Rupture of a papillary muscle caused by hemorrhagic necrosis, with entrapment of the disc of the prosthetic valve has been reported.9) Spontaneous rupture of a papillary muscle after chordal sparing MVR has also been noted.2)4) In our case, the remnant mitral subvalvular apparatus was confused with aortic valve vegetation.
The clinical diagnosis of infective endocarditis is based upon a combination of features such as positive blood cultures, new valvular regurgitation and fever as specified in the modified Duke criteria.10) Typical vegetations of aortic valve endocarditis are characterized by fine fluttering in the left ventricular outflow tract in diastole, which were continuous with similar echo patterns in the aortic root and the appearance of the abnormal echo patterns showing coarse systolic fluttering in the aorta.11) The vegetative growth appears as thickening and irregularity of the normally smooth contour of the sewing ring12) and shows low echogenicity. When abnormal echo patterns in the left ventricular outflow tract are observed, two diagnostic possibilities should be considered:11) the flail valve leaflets and highly mobile, large aortic valve vegetations. One should observe the size, mobility and degree of organization, and lack of homogeneity of the vegetations themselves. However, it should be emphasized that echocardiography alone does not distinguish these two entities. In our case, we could defined the mass around the aortic valve as the remnant subvalvular apparatus of the mitral valve according to serial echocardiographic findings and the patient's clinical signs and symptoms. We also communicated with the surgeon about the method of operation. In addition, great attention should be paid to remnant chordae or leaflet tissues when the anterior leaflet chorda-saving procedure is performed. If there remains a remnant tissue after reattachment of leaflet chordae to the anterior mitral annulus, it should be meticulously trimmed.
In conclusion, we emphasize the importance of performing serial postoperative echocardiography and observing the patient's clinical findings as well as communicating with the surgeon during postoperative management about hardly distinguishable valvular mass that newly appeared after surgery.
Figures and Tables
Fig. 1
A: Preoperative transesophageal echocardiography demonstrating severe mitral regurgitation with the prolapse of the anterior leaflet of the mitral valve. B: Showing color doppler across the mitral valve with severe regurgitation jet. Ao: aorta, LA: left atrium, LV: left ventricle.
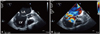
Fig. 2
A: Postoperative transthoracic echocardiography parasternal long axis view showing a mobile mass (arrow) around the aortic valve and normal function of the mechanical valve. B: Doppler image shows that there is no leakage and a well-functioning mechanical mitral valve. LA: left atrium, LV: left ventricle.

Fig. 3
A: Preoperative TTE demonstrating AV without abnormal structure. B: On the 7th postoperative day. C: On the 14th postoperative day. D: On the 21st postoperative day. The transthoracic echocardiography showed 0.3 × 0.6 cm remnant leaflet (arrow) of the mitral valve and no significant change in mass size. AV: aortic valve, Ao: aorta, LA: left atrium, LV: left ventricle, TTE: trans-thoracic echocardiography.

References
1. Nkomo VT, Gardin JM, Skelton TN, Gottdiener JS, Scott CG, Enriquez-Sarano M. Burden of valvular heart diseases: a population-based study. Lancet. 2006. 368:1005–1011.

2. Enriquez-Sarano M, Avierinos JF, Messika-Zeitoun D, Detaint D, Capps M, Nkomo V, Scott C, Schaff HV, Tajik AJ. Quantitative determinants of the outcome of asymptomatic mitral regurgitation. N Engl J Med. 2005. 352:875–883.

3. Ling LH, Enriquez-Sarano M, Seward JB, Tajik AJ, Schaff HV, Bailey KR, Frye RL. Clinical outcome of mitral regurgitation due to flail leaflet. N Engl J Med. 1996. 335:1417–1423.

4. Jokinen JJ, Hippeläinen MJ, Pitkänen OA, Hartikainen JE. Mitral valve replacement versus repair: propensity-adjusted survival and quality-of-life analysis. Ann Thorac Surg. 2007. 84:451–458.

5. David TE, Burns RJ, Bacchus CM, Druck MN. Mitral valve replacement for mitral regurgitation with and without preservation of chordae tendineae. J Thorac Cardiovasc Surg. 1984. 88:718–725.

7. Okita Y, Miki S, Ueda Y, Tahata T, Sakai T, Matsuyama K. Mitral valve replacement with maintenance of mitral annulopapillary muscle continuity in patients with mitral stenosis. J Thorac Cardiovasc Surg. 1994. 108:42–51.

8. Hetzer R, Bougioukas G, Franz M, Borst HG. Mitral valve replacement with preservation of papillary muscles and chordae tendineae - revival of a seemingly forgotten concept. I. Preliminary clinical report. Thorac Cardiovasc Surg. 1983. 31:291–296.

9. Talwar S, Jayanthkumar HV, Kumar AS. Chordal preservation during mitral valve replacement: basis, techniques and results. Indian J Thorac Cardiovasc Surg. 2005. 21:45–52.

10. Li JS, Sexton DJ, Mick N, Nettles R, Fowler VG Jr, Ryan T, Bashore T, Corey GR. Proposed modifications to the Duke criteria for the diagnosis of infective endocarditis. Clin Infect Dis. 2000. 30:633–638.

Supplementary movie legends
Movie 1. Preoperative transesophageal echocardiography demonstrating severe mitral regurgitation with the prolapse of the anterior leaflet of the mitral valve.
Movie 3. TTE parasternal long axis view showing a mobile mass around the aortic valve and normal function of the mechanical valve.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download