Abstract
Cardiac conduction system impairment is a rare clinical manifestation of Behçet's disease. We report a patient who showed 1st degree atrioventricular block at first presentation, and showed aggravated finding of 3rd degree atrioventricular block on five months later. His cardiac manifestation finally developed to acute severe aortic regurgitation on six months later from his first cardiac manifestation. We observed this rapid progression during 6 months and successfully improved symptom and disease severity of the patient with treatment targeting Behçet's disease.
Behçet's disease is an inflammatory disorder that usually involves multiple-organ.1) According to the International Study Group for Behçet's disease, the diagnostic criteria of Behçet's disease are recurrent oral ulceration plus 2 of the followings: recurrent genital ulceration, skin lesions, uveitis, and positive pathergy test.2) Various systemic manifestations can be occurred including arthritis, gastrointestinal symptoms, and neurologic complications.3) Behçet's disease that involve the heart or aorta, such as aortitis and aortic valve regurgitation (AR), is usually less than 2%4) based on case reports but is frequently associated with significant mortality and morbidity. Also, Behçet's disease can affect conduction system, and atrioventricular (AV) conduction impairment is one of the rare manifestation of cardiac involvement.5)6) Surgical intervention in this inflammatory condition carries a high risk of postoperative morbidity because of the fragilities of aortic structures and tissue inflammation.7) We report a patient of Behçet's disease, whose first manifestations were rapidly aggravated AV conduction impairment, and then acutely developed severe AR that successfully treated with bridging immunosuppressant and homograft of ascending aorta and aortic root and aortic valve replacement surgery.
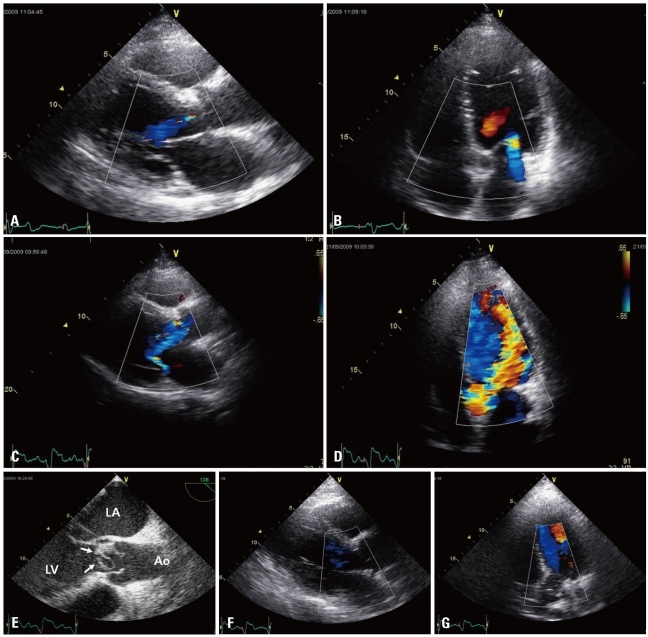
A 50-year-old man visited emergency room for acute onset of New York Heart Association class IV dyspnea for 1 day. He had past medical history of essential hypertension for 10 years and of minimal coronary artery disease on coronary angiography (CAG) undertaken 6 months ago for evaluation of nonspecific chest pain. On that time, electrocardiogram (ECG) showed his rhythm was 1st degree AV block (Fig. 1A) and the transthoracic echocardiography (TTE) showed mild left ventricular (LV) hypertrophy (LV mass = 98 g/m2) without any valvular dysfunctions. Because there was no significant findings in 24 hours holter monitoring, he was discharged without any treatment. After 5 months later, he revisited out-patient clinic for syncope twice during playing golf. The ECG showed complete AV block (Fig. 1B) and after electrophysiologic study of AV node, DDD type permanent pacemaker was implanted. On the TTE examination of 2nd admission, mild LV hypertrophy was still noted without interval change but mild degree of AR was noted (Fig. 2A and B).
On this time, his blood pressure was 110/70 mm Hg and pulse rate was 88 beats per minute. On physical examination, there were grade IV/VI diastolic murmur at the left middle sternal border and rale at both lung fields. Chest X-ray showed pulmonary congestion on both lower lung fields. ECG showed right ventricle pacing beats of P wave tracing by permanent pacemaker (Fig. 1C). On the TTE examination, newly developed severe AR (Fig. 2C and D) was noted and transesophageal echocardiography revealed non-coronary cusp of aortic valve billowing and prolapsing (Fig. 2E) with aortic root dilatation (4.0 cm). In the laboratory examinations, cardiac enzymes were normal, white blood count was 15,900/mm3, erythrocyte sedimentation rate was 31 mm/hr and C-reactive protein was 3.94 mg/dL. We performed blood culture, although there was no fever, and found out that the blood culture was negative. And the patients had no concurrent symptoms suggestive of infective endocarditis. Considering rapidly progressing (during 5 months) conduction disorder and worsening of valvular regurgitation (during 1 month), we suspected of cardiac involvement of systemic inflammatory disease. On history taking, the patient had recurrent oral ulcer without arthritis, genital ulcer or uveitis. Pathergy test was negative. Even though the patient's clinical finding did not fulfill the diagnostic criteria of Behçet's disease, patient's clinical history and echocardiography findings was enough to suspect of cardiac involvement of Behçet's disease. The patient was treated with steroid (prednisolone 80 mg once daily) and immunosuppressants (azathioprine 175 mg once daily) for 3 months and showed good clinical responses without symptom aggravations. After bridging immunosuppressive therapy, open heart surgery for homograft of ascending aorta and aortic root and aortic valve replacement with bioprosthesis (bovine pericardium, #25 mm) was performed. On the pathologic examination of surgical specimen, there were no evidence of infection such as endothelialitis or abscess formation. The gross finding of resected aortic valve and aorta showed light white colored tender leaflet and aorta wall without calcification. The microscopic finding showed fibromyxoid valvulopathy and myxoid change of aorta wall. The follow-up transthoracic echocardiogam on 1 year after open heart surgery with maintenance of azathioprine showed no AR or aortic dilatation with normal LV function and dimension (Fig. 2F and G).
Behçet's disease affects multi-organ and there were well known diagnostic criteria of this disease.1)2) Cardiac manifestations of Behçet's disease are myocarditis, AV block, pericarditis, coronary and valvular involvement, particularly of the aortic valve, and intracardiac thrombosis (right atrial and ventricular thrombosis).8)9) Behçet's disease was found to be the cause of AR in 7 of 153 consecutive patients requiring aortic surgery in a Korean series10) which suggestive of underdiagnosis of Behçet's disease as an etiology of AR in current clinical practice. One of the reason for this underdiagnosis is that preoperative diagnosis of Behçet's disease mainly depends on history and the identification of its typical clinical manifestations due to absence of characteristic pathognomic findings.11) In one study, of the 15 patients with AR and Behçet's disease, only 4 patients were completely fulfilled the current criteria of Behçet's disease. These show that the usefulness of current diagnostic criteria is limited in terms of identifying Behçet's disease as the underlying etiology of AR.12) Severe and symptomatic AR is usually required surgical intervention. However, because of tissue fragility, surgical treatment for AR in Behçet's disease is commonly associated with recurrent regurgitation due to paravalvular leakage, valvular detachment, hemorrhage, and pseudoaneurysm formation.4)13) Also, the management of inflammatory vasculitis required immunosuppressive therapy to prevent postoperative complications.4) Therefore, an early and correct diagnosis of aortic valve involvement by Behçet's disease is required to decide an appropriate treatment strategy. And there has been a concern that current diagnostic criteria may delay the diagnosis of Behçet's disease.12) In our case, the patient's clinical history of recurrent oral ulcer was the only finding that match with the current diagnostic criteria of Behçet's disease, and the diagnosis of Behçet's disease was not made till development of manifest aortic valvulitis with severe AR. Although our patient failed to meet the diagnostic criteria, we suspected Behçet's aortic valvulitis with patient's clinical and echocardiographic findings. And then, we started immunosuppressive therapy.
Behçet's disease firstly manifested by conduction system impairment is seldom founded.5)6) In our case, there was no other possible etiology of complete AV block other than Behçet's disease. Coronary arterial disease and coronary angiitis were excluded by normal CAG. Therefore, we conclude that the complete AV block was related with Behçet's disease involving conduction system. Although the etiology of the conduction impairment in Behçet's disease is not exactly known, inflammation of AV node and surrounding conduction system has been suggested as causes of the impairment of conduction.14) In conclusion, this case report is about rare clinical manifestation of Behçet's disease with rapidly progressive AV conduction delay first, and then rapidly deteriorating aortic valve function to severe regurgitation. We observed this rapid progression within 6 months and under the impression of Behçet's disease, we performed bridging immunosuppressive therapy with open heart surgery and maintenance immunosuppressive therapy for 1 year as treatment. As a result, the patient is doing well without any aggravation of cardiac manifestations so far.
References
1. James DG. Behcet's syndrome. N Engl J Med. 1979; 301:431–432. PMID: 460347.
2. International Study Group for Behcet's Disease. Criteria for diagnosis of Behcet's disease. Lancet. 1990; 335:1078–1080. PMID: 1970380.
3. Ghate JV, Jorizzo JL. Behçet's disease and complex aphthosis. J Am Acad Dermatol. 1999; 40:1–18. quiz 19-20. PMID: 9922007.
4. Akar H, Konuralp C, Akpolat T. Cardiovascular involvement in Behçet's disease. Anadolu Kardiyol Derg. 2003; 3:261–265. PMID: 12967895.
5. Eryol NK, Topsakal R, Abaci A, Oğuzhan A. A case of atrioventricular complete block due to Behçet's disease. Jpn Heart J. 2002; 43:697–701. PMID: 12558133.
6. Unger P, de Cannière D, Preumont N, Fesler P, Cogan E. Subaortic obstruction and complete atrioventricular block in Behçet's disease. Eur J Echocardiogr. 2006; 7:250–252. PMID: 15927536.
7. Esdaile J, Hawkins D, Gold P, Freedman SO, Duguid WP. Vascular involvement in relapsing polychondritis. Can Med Assoc J. 1977; 116:1019–1022. PMID: 870159.
8. Sakane T, Takeno M, Suzuki N, Inaba G. Behçet's disease. N Engl J Med. 1999; 341:1284–1291. PMID: 10528040.
9. Kural-Seyahi E, Fresko I, Seyahi N, Ozyazgan Y, Mat C, Hamuryudan V, Yurdakul S, Yazici H. The long-term mortality and morbidity of Behçet syndrome: a 2-decade outcome survey of 387 patients followed at a dedicated center. Medicine (Baltimore). 2003; 82:60–76. PMID: 12544711.
10. Song JK, Jeong YH, Kang DH, Song JM, Song H, Choo SJ, Lee JW, Song MG. Echocardiographic and clinical characteristics of aortic regurgitation because of systemic vasculitis. J Am Soc Echocardiogr. 2003; 16:850–857. PMID: 12878994.
11. Lee S. Diagnostic criteria of Behçet's disease: problems and suggestions. Yonsei Med J. 1997; 38:365–369. PMID: 9509905.
12. Lee I, Park S, Hwang I, Kim MJ, Nah SS, Yoo B, Song JK. Cardiac Behçet disease presenting as aortic valvulitis/aortitis or right heart inflammatory mass: a clinicopathologic study of 12 cases. Am J Surg Pathol. 2008; 32:390–398. PMID: 18300812.
13. Ando M, Kosakai Y, Okita Y, Nakano K, Kitamura S. Surgical treatment of Behçet's disease involving aortic regurgitation. Ann Thorac Surg. 1999; 68:2136–2140. PMID: 10616990.
14. Nojiri C, Endo M, Koyanagi H. Conduction disturbance in Behçet's disease. Association with ruptured aneurysm of the sinus of valsalva into the left ventricular cavity. Chest. 1984; 86:636–638. PMID: 6478907.
Fig. 1
A: ECG finding of 1st admission on 6 months ago when patient complaint of chest pain shows 1st degree AV block. B: ECG finding of 1 month ago when patient complaint of 2 times of syncope shows complete AV block. C: ECG finding when patients was complaint severe dyspnea on emergency room shows 74 beat per minute of well functioning pacemaker with ventricular pacing beats of P wave tracing. ECG: electrocardiogram, AV: atrioventricular.
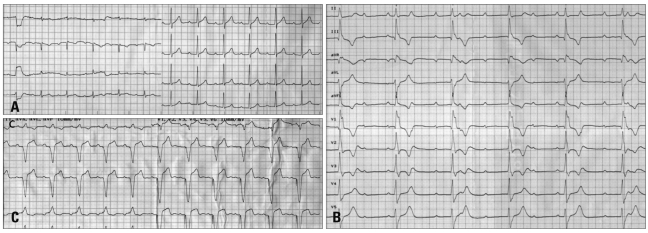
Fig. 2
A and B: TTE findings of 1 month ago when patient complaint of 2 times of syncope in parasternal long axis (A) and apical 5 chamber view (B) show aortic valve regurgitation of mild degree. C and D: On the TTE findings when patients was complaint severe dyspnea on emergency room shows severe aortic valve regurgitation in parasternal long axis (C) and apical 5 chamber view (D). E: On TEE examination, aortic valve thickening and billowing with redundant cusp (white arrows) is noted. F and G: The follow-up TTE on 1 year after open heart surgery showed no AR or aortic dilatation with normal LV function and dimension in parasternal long axis (F) and apical 5 chamber view (G). TTE: transthoracic echocardiography, TEE: transesophageal echocardiography, AR: aortic valve regurgitation, LA: left atrium, LV: left ventricle, Ao: Aorta.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download