Abstract
Atrial septal defect (ASD) with severe pulmonary arterial hypertension (PAH) is thought to preclude shunt closure. However, there are several reports that vasodilator treatment is associated with good clinical outcome in these patients, recently. We report a case of good clinical outcome in a patient with ASD and severe PAH successfully treated with operative closure of ASD and subsequent use of oral bosentan medication. This case supports that the corrective repair of ASD and an oral bosentan treatment can be one of the treatment options in the selected patients with severe PAH associated with ASD.
Pulmonary arterial hypertension (PAH) associated with atrial septal defect (ASD) is clinically important due to increased morbidity and mortality.1)2) Closure of septal defect is one of the options in the treatment in these patients. If the patient's pulmonary arterial pressure is more than 2/3 the systemic pressure, closure can be done with a net left-to-right shunt of at least 1.5 : 1 or evidence of reversibility of the shunt in the cardiac catheterization.2)
Recently, there are several reports about transient use of pulmonary arterial vasodilators in the successful management of PAH in the perioperative period.3)4) Here, we reports a case of remarkable recovery of severe PAH after ASD closure followed by oral endothelin receptor antagonist, bosentan (Tracleer, Actelion, Allschwil, Switzerland).
A 31-year-old woman was referred to our hospital because of worsening of exertional dyspnea for 3 months. Initially, she felt exertional dyspnea about 18 months ago, just after delivery of her second baby. Her symptom got worse with time and presented with exertional dyspnea of NYHA class III, orthopnea, and paroxysmal nocturnal dyspnea at the time of admission. Initial her vital signs were body temperature 36.4℃, heart rate 60/min, respiratory rate 20/min and blood pressure 90/50 mmHg. There was regular heart beat with wide fixed splitting of S2 at the pulmonic valve area and there was no clubbing of the fingers and nails. On her admission, the chest X-ray showed cardiomegaly and dilated pulmonary trunk. The transthoracic echocardiogram revealed about 1.5 cm sized secundum type ASD with bidirectional shunt (mainly left to right shunt). The right ventricle was markedly dilated with D-shaped left ventricle and severe right ventricular systolic dysfunction (Fig. 1). The estimated systolic pulmonary arterial pressure with maximal tricuspid regurgitation velocity was 98 mmHg (TR Vmax = 4.7 m/sec). Cardiac catheterization was performed to assess the reversibility of PAH and evaluate operability. The pulmonary artery pressure and pulmonary vascular resistance were 83/30 mmHg (mean arterial pressure, 47 mmHg) and 11.3 U/m2 in room air, respectively. After administration of oxygen (5l/min via nasal prong), her pulmonary arterial pressure was slightly decreased to 73/30 mmHg (mean arterial pressure, 45 mmHg). Transient obstruction of septal defect with a sizing balloon decreased her pulmonary arterial pressure to 70/25 mmHg (mean arterial pressure, 40 mmHg). The calculated pulmonary to systemic flow ratio (Qp/Qs) and pulmonary to systemic vascular resistance ratio (Rp/Rs) were 1.5 and 0.33, respectively.
Though the patient had severe resting PAH with partial reversibility, we decided to close ASD because of her young age, relatively small defect size and no clubbing of her fingers. Initially we wanted to control PAH with oral sildenafil treatment preoperatively, the patient did not take medication because of side effect and financial problem. On fifth hospital day, the patient underwent operative closure of ASD with autopericardial patch. Because of markedly increased systolic pulmonary arterial pressure, the operator mad flap-valve shaped patch closure. Immediate postoperatively, her systolic pulmonary arterial pressure was 81 mmHg, whereas systolic arterial pressure was 92 mmHg. She was medicated with oral bosentan (62.5 mg po bid) the day after surgery. On the fifth postoperative day, her systolic pulmonary arterial pressure was dropped to 35 mmHg. Her symptoms were disappeared after the operation and medical management including bosentan.
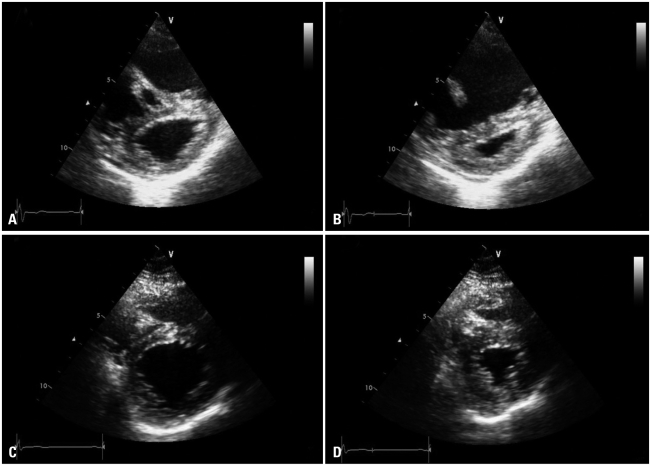
Four months after the closure, transthoracic echocardiogram showed remarkable reduction of right ventricular size and marked reduction of PAH (TR Vmax = 3.3 m/sec). The patient was not medicated any medication after 4 months. The follow-up echocardiogram after 7 months demonstrated normal pulmonary arterial pressure (TR Vmax = 2.5 m/sec) with normal right ventricular size and function. At last assessment (31 months after the surgery), the patient had no symptom and the follow-up echocardiogram confirmed normal right ventricular contractility without PAH (Fig. 2).
In this report, we presented a case with severe PAH associated with secundum type ASD who was successfully treated with operation and transient use of oral bosentan.
ASD is most common congenital heart disease in adults. PAH can occur as a result of chronic exposure of the pulmonary vessels to increased blood flow through the shunt.1) Histologic changes in the intima and media of the pulmonary vessels can be resulted in the luminal narrowing and subsequent development of PAH.5) According to previous studies, the prevalence of PAH is 6-17% of patients with ASD.6)7) The presence of PAH is associated with poor prognosis in the patients with ASD.1)2) Increased pulmonary arterial pressure can be lowered with septal closure. Balint et al.8) reported successful outcomes after transcatheter closure in selected patients with secundum ASD and PAH. Initial pulmonary vasodilator therapy may be beneficial in patients with irreversible anatomic changes of pulmonary vessels in the previously published data.3)4)9)10) Schwerzmann et al.4) described a 38-year-old woman with ASD and severe PAH, who showed significant symptomatic and hemodynamic improvement after 1 year of treatment with intravenous prostacyclin. The ASD was closed percutaneously after the pulmonary vasodilator therapy. Kim et al.3) reported a 41-year-old woman with Eisenmenger syndrome who was initially managed with oral sildenafil for 2 years and ASD was successfully closed. In our case, we successfully managed severe PAH with the surgical repair of ASD and subsequent use of oral bosentan therapy.
Although decision of operative closure in this patient was difficult, we decided to operate the ASD on the basis of clinical situation and the result of cardiac catheterization. Several reports already showed that the hemodynamic determination of operability in patients with ASD and severe PAH was problematic.5)9)11) However, there are reported cases with transient use of vasodilator therapy was associated with good result in the management of PAH associated with ASD. There is a report that younger age was associated with good prognosis in the surgical correction of ASD.2)
In conclusion, we experienced a case of dramatic improvement of severe PAH and right ventricular dysfunction after ASD closure followed by an oral bosentan treatment. Our case suggests that the operability in patients with ASD and severe PAH should be decided with discretion on a case by case. The corrective repair of ASD and subsequent oral bosentan treatment can be an option in the treatment of selected patients with severe PAH and right ventricular dysfunction.
References
1. Steele PM, Fuster V, Cohen M, Ritter DG, McGoon DC. Isolated atrial septal defect with pulmonary vascular obstructive disease--long-term follow-up and prediction of outcome after surgical correction. Circulation. 1987; 76:1037–1042. PMID: 3664992.
2. Murphy JG, Gersh BJ, McGoon MD, Mair DD, Porter CJ, Ilstrup DM, McGoon DC, Puga FJ, Kirklin JW, Danielson GK. Long-term outcome after surgical repair of isolated atrial septal defect. Follow-up at 27 to 32 years. N Engl J Med. 1990; 323:1645–1650. PMID: 2233961.
3. Kim YH, Yu JJ, Yun TJ, Lee Y, Kim YB, Choi HS, Jhang WK, Shin HJ, Park JJ, Seo DM, Ko JK, Park IS. Repair of atrial septal defect with Eisenmenger syndrome after long-term sildenafil therapy. Ann Thorac Surg. 2010; 89:1629–1630. PMID: 20417794.
4. Schwerzmann M, Zafar M, McLaughlin PR, Chamberlain DW, Webb G, Granton J. Atrial septal defect closure in a patient with "irreversible" pulmonary hypertensive arteriopathy. Int J Cardiol. 2006; 110:104–107. PMID: 15992947.
5. Sachweh JS, Daebritz SH, Hermanns B, Fausten B, Jockenhoevel S, Handt S, Messmer BJ. Hypertensive pulmonary vascular disease in adults with secundum or sinus venosus atrial septal defect. Ann Thorac Surg. 2006; 81:207–213. PMID: 16368366.
6. Cherian G, Uthaman CB, Durairaj M, Sukumar IP, Krishnaswami S, Jairaj PS, John S, Krishnaswami H, Bhaktaviziam A. Pulmonary hypertension in isolated secundum atrial septal defect: high frequency in young patients. Am Heart J. 1983; 105:952–957. PMID: 6858843.
7. Craig RJ, Selzer A. Natural history and prognosis of atrial septal defect. Circulation. 1968; 37:805–815. PMID: 5646864.
8. Balint OH, Samman A, Haberer K, Tobe L, McLaughlin P, Siu SC, Horlick E, Granton J, Silversides CK. Outcomes in patients with pulmonary hypertension undergoing percutaneous atrial septal defect closure. Heart. 2008; 94:1189–1193. PMID: 17932093.
9. Yamauchi H, Yamaki S, Fujii M, Iwaki H, Tanaka S. Reduction in recalcitrant pulmonary hypertension after operation for atrial septal defect. Ann Thorac Surg. 2001; 72:905–906. discussion 906-7. PMID: 11565678.
10. Galiè N, Beghetti M, Gatzoulis MA, Granton J, Berger RM, Lauer A, Chiossi E, Landzberg M. Bosentan Randomized Trial of Endothelin Antagonist Therapy-5 (BREATHE-5) Investigators. Bosentan therapy in patients with Eisenmenger syndrome: a multicenter, double-blind, randomized, placebo-controlled study. Circulation. 2006; 114:48–54. PMID: 16801459.
11. Yamaki S, Horiuchi T, Miura M, Haneda K, Ishizawa E, Suzuki Y. Secundum atrial septal defect with severe pulmonary hypertension. Open lung biopsy diagnosis of operative indication. Chest. 1987; 91:33–38. PMID: 3792083.
Fig. 1
The transthoracic echocardiogram shows markedly dilated right ventricle and dysfunction (A) end-diastole, and (B) end-systole. There is significant shunt between left and right atria through the septal defect and the measured defect size was 1.5 cm (arrows, C). The measured maximal tricuspid regurgitation velocity is 4.7 m/sec suggesting severe pulmonary arterial hypertension (estimated pulmonary arterial systolic pressure is 98 mmHg, D).
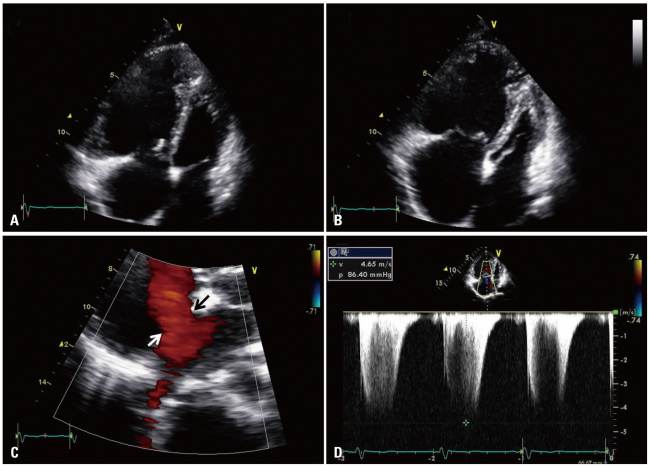
Fig. 2
The initial echocardiography reveals D-shaped left ventricle (A) end-diastole, and (B) end-systole. The follow-up transthoracic echocardiogram taken 31 months after the surgery demonstrates markedly decreased right ventricular size and disappeared right ventricular dysfunction (C) end-diastole, and (D) end-systole.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download