Abstract
A 56-year-old male presented with resting dyspnea and chest discomfort for several years. During transthoracic and transesophageal echocardiography, a spontaneously healed membranous type ventricular septal defect (VSD) with malaligned interventricular septal wall, aneurysmal changes, a subaortic ridge and a double-chambered right ventricle (DCRV) was observed. When combined with DCRV, VSD with malalignment between the outlet and trabecular septa was associated with tetralogy of Fallot. The subaortic ridge was due to turbulent flow caused by the malalignment-type VSD. The VSD with malaligned interventricular septal wall can be developed after aneurismal changes of a perimembranous VSD. We report here in the unusual case of a 56-year-old patient who had a pathology complex comprising DCRV, subaortic ridge, spontaneously healed membranous type VSD with malaligned interventricular septal wall, and survived with surgical treatment.
Double-chambered right ventricle (DCRV) is a cardiac disease of the right ventricular outflow tract, where anomalous muscle bundles or a fibrous band cause obstruction.1-3)
A malaligned interventricular septal wall can develop in patients with aneurismal changes of ventricular septal defect (VSD), the degree of which usually increases with time.4) Furthermore, when combined with DCRV, VSD with malalignment between the outlet and trabecular septa was associated with tetralogy of Fallot. A subaortic ridge in the malalignment-type VSD is caused by turbulent flow.5-7) We describe here in the unusual case of a 56-year-old man who had a spontaneously healed membranous type VSD with malaligned interventricular septal wall, DCRV, subaortic ridge, and survived with surgical treatment.
A 56-year-old male presented with resting dyspnea and chest discomfort for several years. He had no history of any surgical or catheter-based cardiovascular interventions. Physical examination showed a cardiac systolic murmur (grade 4/6) on the left upper sternal border, a systemic blood pressure of 140/75 mmHg, and a heart rate of 110 bpm. Electrocardiography showed sinus tachycardia, right axis deviation and frequent premature ventricular contraction with right ventricular bundle branch block morphology.
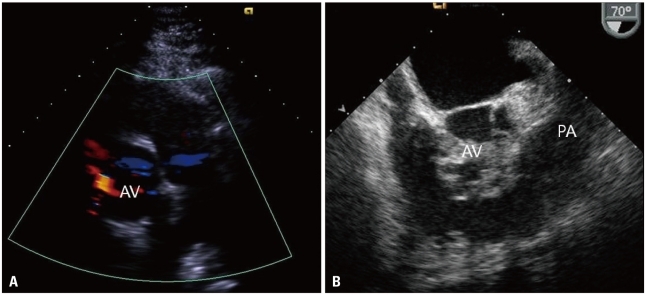
Transthoracic and transesophageal echocardiography revealed a membranous type VSD with anteriorly malaligned interventricular septum, aneurysmal changes, subaortic ridge and DCRV with right ventricular hypertrophy (Fig. 1). Measurement of pressure gradients using a Doppler image was not made because the ultrasound beam could not be made parallel to the outflow tract jet. Right ventriculography confirmed an anomalous obstruction within the right ventricle. Preoperative cardiac catheterization demonstrated a right ventricle-to-pulmonary artery gradient of 89 mmHg (Fig. 2 and 3). Left ventriculography revealed a membranous VSD with anteriorly malaligned interventricular septum, aneurysmal changes. The patient underwent open-heart surgery involving resection of an encircling infundibular fibrous band through right atriotomy. Resection of the subaortic ridge was not carried out because it caused mild aortic regurgitation without pressure gradients in the left ventricular outflow tract. Dyspnea was improved at follow-up. Transthoracic echocardiography taken after surgery revealed that the high-velocity systolic jet in the mid right ventricular outflow tract disappeared and that right ventricular outflow tract diameter was much improved (Fig. 4).
Approximately two-thirds of patients have VSD that is diminished in size by aneurysmal changes with apposition of tricuspid tissue over the VSD.4) In our case, transthoracic and transesophageal echocardiography revealed a membranous type VSD with anteriorly malaligned interventricular septum, aneurysmal changes. The parasternal long axis view is useful for determining the degree of aortic overriding (Fig. 1D). DCRV is an infundibular pulmonary stenosis resulting from discrete fibromuscular narrowing or hypertrophied subvalvular muscle bundles. In many cases, VSD is combined DCRV.1-3) Also, malaligned between the outlet and trabecular septa VSD with DCRV is associated with TOF.6)8)9) In our patient, DCRV was not associated TOF because anteriorly malaligned interventicular septum without malalignment of infudibular septum was combined. VSD was located very close to the right aortic cusp and showed spontaneous closure with aneurysmal formation, which is rare without aortic valve prolapse.9-11)
The subaortic ridge is a fibrous structure from the crest of the ventricular septum to the left ventricular outflow tract. This case had a subaortic ridge caused by increased turbulence adjacent to the area of VSD and enhanced by septal malalignment.6)7) A subaortic ridge may result in progressive subaortic stenosis or aortic valve deformities, and resection is usually recommended. In our case, the patient underwent resection of an encircling infundibular fibrous band through right atriotomy. However, resection of the subaortic ridge was not carried out because it caused mild aortic regurgitation without any pressure gradients in the left ventricular outflow tract.
In summary, the malaligned interventricular septum in membranous type VSD can develop secondary to aneurismal changes of VSD. We reported the unusual case of a patient who had a pathology complex comprising DCRV, subaortic ridge, and VSD with malaligned interventricular septal wall and survived with surgical treatment.
References
1. Maron BJ, Ferrans VJ, White RI Jr. Unusual evolution of acquired infundibular stenosis in patients with ventricular septal defect. Clinical and morphologic observations. Circulation. 1973; 48:1092–1103.
2. Choi YJ, Park SW. Characteristics of double-chambered right ventricle in adult patients. Korean J Intern Med. 2010; 25:147–153. PMID: 20526387.
3. McElhinney DB, Chatterjee KM, Reddy VM. Double-chambered right ventricle presenting in adulthood. Ann Thorac Surg. 2000; 70:124–127. PMID: 10921695.
4. Wu MH, Wu JM, Chang CI, Wang JK, Wu YN, Chien SC, Lue HC. Implication of aneurysmal transformation in isolated perimembranous ventricular septal defect. Am J Cardiol. 1993; 72:596–601. PMID: 8362777.
5. Matina D, van Doesburg NH, Fouron JC, Guérin R, Davignon A. Subxiphoid two-dimensional echocardiographic diagnosis of double-chambered right ventricle. Circulation. 1983; 67:885–888. PMID: 6825244.
6. Wang JK, Wu MH, Chang CI, Chiu IS, Chu SH, Hung CR, Lue HC. Malalignment-type ventricular septal defect in double-chambered right ventricle. Am J Cardiol. 1996; 77:839–842. PMID: 8623736.
7. Zielinsky P, Rossi M, Haertel JC, Vitola D, Lucchese FA, Rodrigues R. Subaortic fibrous ridge and ventricular septal defect: role of septal malalignment. Circulation. 1987; 75:1124–1129. PMID: 3568324.
8. Wu MH, Wang JK, Chang CI, Chiu IS, Lue HC. Implication of anterior septal malalignment in isolated ventricular septal defect. Br Heart J. 1995; 74:180–185. PMID: 7546999.
9. Oppenheimer-Dekker A, Gittenberger-de Groot AC, Bartelings MM, Wenink AC, Moene RJ, van der Harten JJ. Abnormal architecture of the ventricles in hearts with an overriding aortic valve and a perimembranous ventricular septal defect ("Eisenmenger VSD"). Int J Cardiol. 1985; 9:341–355. PMID: 4055151.
10. Vogel M, Smallhorn JF, Freedom RM, Coles J, Williams WG, Trusler GA. An echocardiographic study of the association of ventricular septal defect and right ventricular muscle bundles with a fixed subaortic abnormality. Am J Cardiol. 1988; 61:857–860. PMID: 3354451.
11. Kim CJ, Chai IH, Koh KK, Sohn DW, Lee MM, Park YB, Choi YS, Seo JD, Lee YW. Double chambered right ventricle (DCRV) in adult and adolescence. Korean Circ J. 1990; 20:248–255.
Fig. 1
Preoperative transthoracic and transesophageal echocardiography. (A) Transthoracic echocardiography reveals a high-velocity systolic jet arising in the mid right ventricular outflow tract. (B) Right ventricular hypertrophy is seen on the parasternal long axis view. Transesophageal echocardiography reveals a subaortic ridge (arrowhead) (C) and aneurysmal changes (arrowhead) of the ventricular septal defect with anterior deviated interventricular septum (D). AV: aortic valve, RV: right ventricle, LV: left ventricle, IVS: interventricular septum.
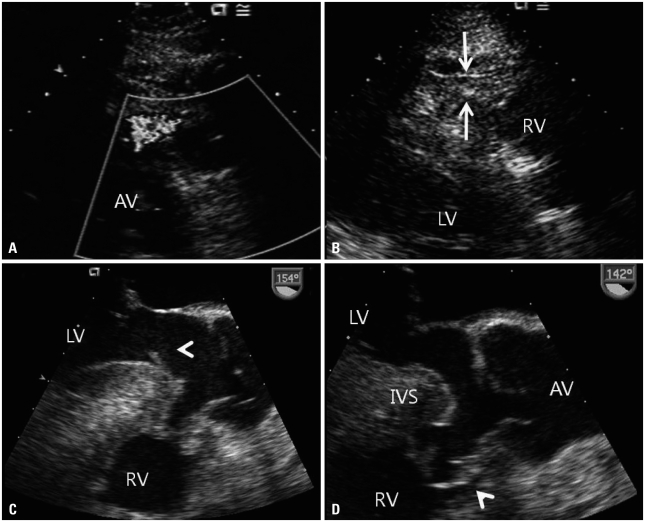
Fig. 2
Preoperative right and left ventriculography. Right ventriculography at end-systole reveals an anomalous muscle bundle dividing the cavity into 2 chambers (A), and left ventriculography shows spontaneous closed malalignmented ventricular septal defect with aneurysmal changes (B). DCRV: double-chambered right ventricle.
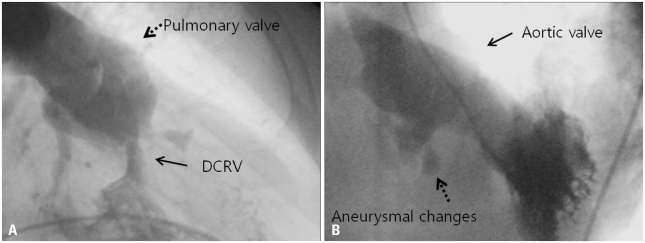
Fig. 3
Preoperative cardiac catheterization demonstrates a right ventricle-to-pulmonary artery gradient of 89 mmHg. There is no significant step-up of O2 saturation in the right ventricular sample that is higher than the highest right atrial sample because of spontaneously closed malalignmented ventricular septal defect. Systolic pressure/diastolic pressure is expressed as a mean pressure and O2 saturation as a percentage. SVC: superior vena cava, RA: right atrium, RV: right ventricle, MPA: main pulmonary artery, RPA: right pulmonary artery, PCWP: pulmonary capillary wedge pressure, LV: left ventricle.
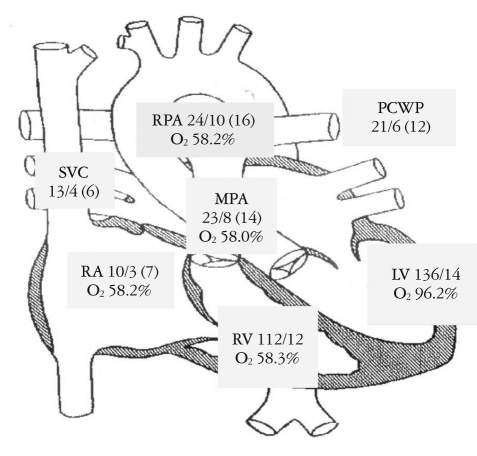
Fig. 4
Postoperative transthoracic and transesophageal echocardiography. A: Transthoracic echocardiography reveals that a high-velocity systolic jet arising in the mid right ventricular outflow tract disappeared after surgery. B: Transesophageal echocardiography reveals much improved right ventricular outflow tract diameter after surgery. AV: aortic valve, PA: pulmonary artery.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download