Abstract
Treatment by All-trans retinoic acid (ATRA) followed by anthracycline-AraC chemotherapy has improved the outcome of acute promyelocytic leukemia. ATRA is usually well tolerated, but a few major side effects can be observed. Retinoic acid syndrome (RAS) often occurs during the induction chemotherapy of acute promyelocytic leukemia. A pericardial effusion is a common cardiac manifestation but myocarditis has been rarely documented. Here we reports a very rare case of fully recovered myocarditis as a result of RAS related to ATRA administration during induction treatment of acute promyelocytic leukemia which documented by echocardiographic evidence.
Treatment by All-trans retinoic acid (ATRA) followed by anthracycline-AraC chemotherapy has improved the outcome of acute promyelocytic leukemia.1) ATRA is usually well tolerated, but a few major side effects can be observed.2-4) Retinoic acid syndrome (RAS) often occurs during the induction chemotherapy of acute promyelocytic leukemia. In RAS, myocarditis has been rarely documented. We reports a very rare case of fully recovered myocarditis as a result of RAS related to ATRA administration during induction treatment of acute promyelocytic leukemia which documented by echocardiographic evidence.
A 39-year-old woman was admitted to our hospital due to dyspnea and dizziness. The patient had been well until approximately 8 weeks earlier, when dyspnea and dizziness developed. She was physically active and did not have a history of hypertension, diabetes, hospitalizations, surgical procedures, or allergic reactions to drugs. She was taking no medications at the time of the admission.
On physical examination, she appeared in acute distress. The blood pressure and heart rate were 130/80 mmHg, 84 beats per minute, each other, and the respiratory rate 20 breaths per minute. The physical examination of the head, ears, eyes, nose, and throat were otherwise normal. No lymph node was palpable in the cervical, axillary, and inguinal regions. The lungs and heart were normal on auscultation except functional systolic murmur. The abdomen was softly palpated with normal bowel sounds. There is no hepatosplenomegaly. The genitourinary, cutaneous, and neurologic examinations were normal, as was examination of his arms and legs.
The initial complete blood counts showed hemoglobin of 3.3 g/dL; white blood cell count of 2.16 × 109/L; platelets count of 18 × 109/L. Examination of the peripheral-blood smear revealed pancytopenia and a few immature cells with Auer rods. Examination of the biopsy specimen showed that the bone marrow was hypercellular (> 95%) and replaced by abnormal large cells with Auer rods and cytoplasmic dense large granules. On the smear of the aspirate, 57% of the cells were promyelocytes and 2.6% were myeloblasts. On cytochemical staining, the promyelocytes were positive for myeloperoxidase, Sudan Black B stain and Periodic Acid stain. An abnormal karyotype, t (15;17) (q22;q12), was identified. Real-timepolymerase chain reaction (PCR) revealed a promyelocytic leukemia-retinoic acid receptor α (PML/RARa) rearrangement. She was finally diagnosed with acute promyelocytic leukemia.
She received induction therapy (ATRA 45 mg/m2 from day 1 to complete remission, and idarubicin 12 mg/m2 IV on day 2, 4, 6 and 8) and supportive therapy with platelet and plasma transfusion. Screening echocardiography was performed before induction therapy and showed normal wall motions and 60% of ejection fraction.
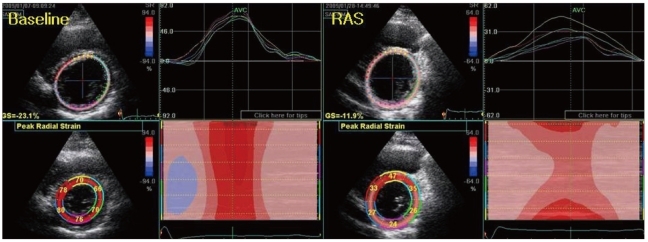
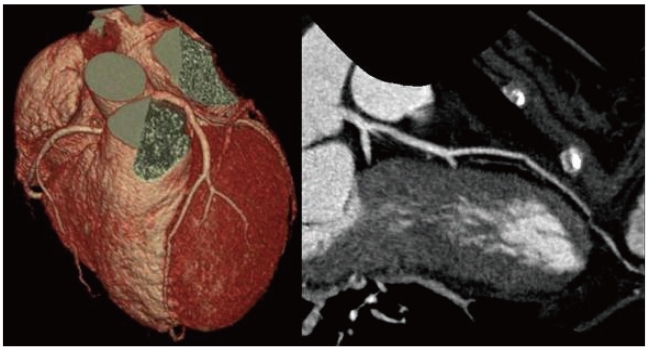
No complication was observed until 17 day from the start of induction therapy. However, the patient complained mild chest pain and dyspnea on day 18 and febrile sense on day 20. Blood pressure was 110/70 mmHg and pulse rate was 120 beats per minute. But body temperature was 40.2℃. Physical examination showed no abnormalities except mild pretibial pitting edema. The electrocardiogram revealed low QRS amplitudes without newly developed Q wave or ST segment change. Laboratory findings showed a white blood cell count of 1.06 × 109/L, a creatine kinase of 52 IU/L (21-232), CK-MB of 2.5 ng/mL (0.0-5.0), a brain natriuretic peptide of 1430 pg/mL (0-100), Troponin-I of 2.39 ng/mL (0.0-0.05), and positive Troponin-T 0.14 ng/mL (0.0-0.03). The echocardiography revealed decreased LV systolic function (left ventricular ejection fraction 38%) with mildly enlarged LV chamber size (56/43 mm), increased left atrial volume index (36.9 mL/m2) and moderate mitral and tricuspid regurgitation (grade II). Diastolic property was restrictive LV filling pattern (mitral E velocity 1.07 m/s, mitral A velocity 0.42 m/s, deceleration time,125 ms, EA ratio; 2.59) and E/Em was elevated (13.4) (Fig. 1). The anterior base to mid segment of left ventricular wall showed severe hypokinetic motion. LV apex and lateral and inferior wall thickening were normal. Comparing baseline LV global radial strain, global radial strain was decreased -19.2% into -14.5% and color-coded strain pattern form anterior to lateral segmental at mid LV wall was decreased (Fig. 2). 64-channel Multidetector CT-coronary Angiography for exclusion of ischemic coronary artery disease revealed that there was no significant obstructive epicardial coronary artery disease or anatomic variances (Fig. 3).
All blood, sputum, urine cultures were negative. A diagnosis of RAS was made on day 22 because of pretibial pitting edema, mild chest pain with dyspnea and unexplained fever (40.2℃). ATRA was discontinued while dexamethasone and diuretics were administered. In the following days, fever was disappeared and the patient symptoms were disappeared. Echocardiography repeated on day 37 (when the patient was fully recovered) revealed normalized chamber size of left ventricle and left atrium. LV systolic function and diastolic function was normalized without wall motion abnormality. ATRA was reintroduced in the following three cycles of consolidation chemotherapy without complication. The patient achieved molecular complete remission after induction therapy, which was sustained through the consolidation therapy.
ATRA has a central role in the treatment of acute promyelocytic leukemia because addition of ATRA to anthracyclines has been shown to improve disease-free survival and overall survival compared to chemotherapy alone.1) Since the promyelocytic leukemia-retinoic acid receptor fusion gene product that is resulted from the balanced translocation t (15;17), characteristic for acute promyelocytic leukemia, has a unique sensitivity to ATRA, ATRA induces the differentiation of leukemic promyelocytes into mature cells.
Though ATRA therapy is considered to be safe and cause mild adverse effects, it can be complicated severely by the RAS, which was first documented by Frankel et al.2) RAS occurs in up to 25% of patients treated with ATRA.1)3)
The RAS is characterized by development of fever, pulmonary infiltrates and effusions, pericardial effusions, hypotension, dyspnea, and renal dysfunction. The morbidity and mortality of RAS is significant and reported mortality rate was as high as 9%.
The diagnosis of RAS is by at least three of the followings: weight gain, respiratory distress, unexplained fever, interstitial pulmonary infiltrates, pleural or pericardial effusions. In patient described above, she was diagnosed as RAS because of pretibial pitting edema, mild chest pain and dyspnea and unexplained fever (40.2℃). And the patient's clinical symptoms and signs ware disappeared after discontinuation of ATRA and there was no recurrence of symptoms after ATRA resuming. The stress induced cardiomyopathy was ruled out because of there were no evidence of newly developed electrocardiographic abnormalities despite transient left ventricular wall motion abnormalities and absence of obstructive coronary artery disease.
The pathogenesis of the ATRA syndrome is not yet fully understood, but it is thought to be due to leukocyte infiltration and cytokine release causing endothelial damage and extravasation of APL cells upon maturation induction by ATRA treatment.4) Common cardiac manifestation of RAS is pericardial effusion (19%) and fatal pericardial tamponade may be occur.5)6) But myocarditis is rare complication. To our knowledge, only four cases of ATRA-induced generalized myocarditis with cardiac involvement has been reported.7-10) In our case, patient had symptoms of myocarditis with laboratory evidence of elevated b-type natriuretic peptide level and transient cardiac troponin after induction of ATRA treatment. The evidence for myocarditis-transient reversible LV dysfunction was also documented by echocardiogram.
In conclusion, we present a case of ATRA-induced, myocarditis that was diagnosed by serologic and echocardiographic evidence. The patient recovered completely without sequale and was subsequently retreated with ATRA without recurrence of the myocarditis.
References
1. Tallman MS, Andersen JW, Schiffer CA, Appelbaum FR, Feusner JH, Ogden A, Shepherd L, Willman C, Bloomfield CD, Rowe JM, Wiernik PH. All-trans-retinoic acid in acute promyelocytic leukemia. N Engl J Med. 1997; 337:1021–1028. PMID: 9321529.
2. Frankel SR, Eardley A, Lauwers G, Weiss M, Warrell RP Jr. The "retinoic acid syndrome" in acute promyelocytic leukemia. Ann Intern Med. 1992; 117:292–296. PMID: 1637024.
3. Patatanian E, Thompson DF. Retinoic acid syndrome: a review. J Clin Pharm Ther. 2008; 33:331–338. PMID: 18613850.
4. Fenaux P, De Botton S. Retinoic acid syndrome. Recognition, prevention and management. Drug Saf. 1998; 18:273–279. PMID: 9565738.
5. Larrea L, de la Rubia J, Jiménez C, Martín G, Sanz MA. Cardiac tamponade and cardiogenic shock as a manifestation of all-trans retinoic acid syndrome: an association not previously reported. Haematologica. 1997; 82:463–464. PMID: 9299864.
6. Leelasiri A, Numbenjapol T, Prayoonwiwat W, Mongkolsritrakul W, Srisawat C. Successful treatment of retinoic acid syndrome with dexamethasone: a case report. J Med Assoc Thai. 2005; 88(Suppl 3):S302–S310. PMID: 16858973.
7. Fabbiano F, Magrin S, Cangialosi C, Felice R, Mirto S, Pitrolo F. All-trans retinoic acid induced cardiac and skeletal myositis in induction therapy of acute promyelocytic leukaemia. Br J Haematol. 2005; 129:444–445. PMID: 15842672.
8. Klein SK, Biemond BJ, van Oers MH. Two cases of isolated symptomatic myocarditis induced by all-trans retinoic acid (ATRA). Ann Hematol. 2007; 86:917–918. PMID: 17619879.
9. Manna A, Cadenotti L, Motto A, Ballo P. Reversible cardiac dysfunction without myocytolysis related to all-trans retinoic acid administration during induction therapy of acute promyelocytic leukemia. Ann Hematol. 2009; 88:91–92. PMID: 18633613.
10. van Rijssel RH, Wegman J, Oud ME, Pals ST, van Oers MH. A case of ATRA-induced isolated myocarditis in the absence of circulating malignant cells: demonstration of the t(15;17) translocation in the inflammatory infiltrate by in situ hybridisation. Leuk Res. 2010; 34:e142–e144. PMID: 20060166.
Fig. 1
Left ventricular (LV) systolic and diastolic dysfunction at retinoic acid syndrome attack. A: Decreased LV systolic function (LV ejection fraction 38%) by LV M-mode. B: Abnormal LV diastolic function (E/Em 13.4) - restrictive LV ventricular filling. LVEDD: LV end systolic diameter, LVESD: LV end systolic diameter, LVEF: left ventricular ejection fraction, E: early diastolic mitral inflow velocity, Em: early diastolic mitral tissue Doppler velocity.
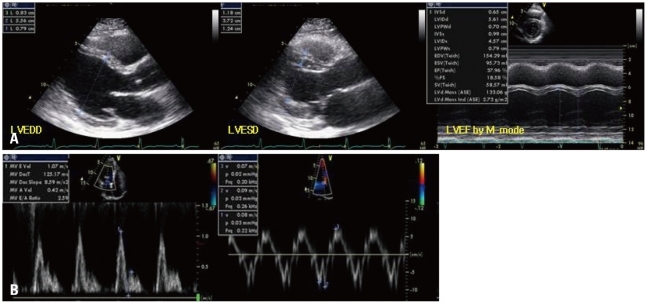
Fig. 2
The change of left ventricular (LV) global radial strain at LV mid wall. Comparing baseline LV global radial strain, global radial strain at RAS was decreased -19.2% to -14.5% and color-coded strain pattern form anterior to lateral segmental at mid LV wall was decreased. RAS: retinoic acid syndrome.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download