Abstract
Background
Anemia is associated with worse long term outcomes in heart failure. However, there is little evidence on the effect of low hemoglobin level to the left ventricular (LV) structure and diastolic function in hypertensive patients. This study assessed the relationship of hemoglobin level to LV filling pressure in elderly hypertensive patients.
Methods
From January 2005 to January 2009, 200 newly diagnosed hypertensive patients over 50 years old (mean age 60 ± 6 years, 116 women) were analyzed. The clinical parameters and comprehensive echocardiographic data were obtained. The patients with and without anemia were compared.
Results
There were significant differences between the anemic and non-anemic groups in the LV mass index (115.27 ± 34.95 vs. 103.75 ± 28.21 g/m2), left atrial (LA) volume index (29.31 ± 10.74 vs. 24.99 ± 7.43 mL/m2), and E/E' (11.92 ± 4.34 vs. 9.37 ± 2.51). Chronic renal failure was more prevalent in anemic group. On multivariate logistic analysis, anemia was significantly correlated with high LV filling pressure, reflected by E/E', even after controlling for LV mass index and LA volume index. Furthermore, E/E' was significantly correlated with the hemoglobin level (R2 = 0.093, p < 0.001).
Approximately 50% of heart failure patients are known to have normal left ventricular ejection fraction. Individuals with heart failure with normal ejection fraction are typically older and more likely to be women and more likely to have hypertension, obesity, renal failure, anemia, or atrial fibrillation.1) Diastolic dysfunction plays an important role in heart failure with normal ejection fraction, but there is still much controversy about the underlying pathophysiology.
Anemia reduces oxygen delivery to tissues and causes a compensatory cardiovascular response. Chronic anemia is usually accompanied by increased cardiac mass and left ventricular eccentric hypertrophy.2)3) Diastolic dysfunction has been found to be common in patients with hypertension even before left ventricular hypertrophy is demonstrable, and recent studies have shown that isolated diastolic dysfunction accompanies hypertensive heart disease.4)5)
Several studies in patients with diabetes, chronic kidney disease, or coronary artery disease have supported an association between anemia and left ventricular (LV) diastolic dysfunction,6-8) but there is no previous data on the effect of low hemoglobin level on LV diastolic function and cardiac structure in hypertensive patients.
The purpose of the present study was to seek whether low hemoglobin level is related to LV structure and LV filling pressure in elderly hypertensive patients over 50 years old.
Patients were eligible to participate if they were newly diagnosed to have hypertension at the outpatient clinic in Ewha Womans University Mok-dong Hospital from January 2005 to January 2009. Hypertension was defined as follows; resting systolic blood pressure ≥ 140 mmHg or resting diastolic blood pressure ≥ 90 mmHg on measurements performed twice within a 5-minute interval in a quiet room. Patients who had established cardiovascular diseases such as ischemic heart disease, stroke, valvular heart disease, or arrhythmia, patients younger than 50 years of age, and patients who had already been anti-hypertensive medication were excluded.
Two hundred hypertensive patients were included retrospectively. All patients underwent echocardiography at the time of hypertension diagnosis. Systolic and diastolic blood pressures were measured with a standard sphygmomanometer. Body mass index was calculated by measured body weight and height. Serum blood urea nitrogen, creatinine, and sodium were assayed.
Venous blood samples were drawn into the tube that contained ethylene-diamine-tetraacetic acid (EDTA). Hemoglobin values were obtained with the Sysmex XE-2100 (TOA Medical Electronics, Kobe, Japan). Laboratory technicians who measured these values were blinded from the result of the echocardiogram. Anemia was defined as Hb < 13 g/dL in men and Hb < 12 g/dL in women based on cut-off point of World Health Organization.9)
Transthoracic echocardiography was performed using a commercially available imaging ultrasound system (Sonos 5500, Hewlett-Packard Co., Palo Alto, CA, USA) with harmonic imaging. All examinations were carried out by experienced sonographers and were analyzed by two experienced observers who were blinded to clinical data. Quantification of the chamber areas was performed according to the recommendations of the American Society of Echocardiography.10) The LV internal diameter, septal thickness, and LV posterior wall thickness were measured at the end-diastole, as defined by the onset of the QRS complex.
The LV mass was calculated using the following formula:11)
0.80×1.04×[(LVEDD+LVST+PWT)3-(LVEDD)3]+0.6
LVEDD is the LV end-diastolic diameter, LVST is the LV septal thickness, and PWT is the posterior wall thickness. The LV mass was indexed for the body surface area to obtain the LV mass index.
The left atrial (LA) diameter was measured by two-dimensional guided M-mode echocardiography obtained from the parasternal short-axis view at the base of the heart.12) The LA volume was calculated using the formula for the biplane area-length method,13) and the LA volume index was obtained by calculating the LA volume-to-body surface area ratio.
Mitral inflow velocities were obtained by pulsed-wave Doppler in the apical four-chamber view with a 1-2 mm sample volume placed at the tips of the mitral valve leaflets. Mitral early (E) and late (A) inflow velocities and the deceleration time (DT) of the E velocity were measured. Using the pulsed-wave tissue Doppler image, early (E') and late (A') diastolic mitral annular velocities were obtained at the septal and lateral mitral annulus level in the apical four-chamber view with septal annulus movement aligned with the sample volume line. The ratio of early transmitral inflow to septal diastolic velocity of the mitral annulus (E/E') was calculated.
The LV outflow tract (LVOT) area was calculated from the LVOT diameter assuming a circular orifice. The stroke volume was calculated as the product of the LVOT area and the time velocity integral of LVOT. Cardiac output was indexed for body surface area to obtain cardiac index.
Data were analyzed using SPSS 15.0 software (SPSS, Chicago, IL, USA). Continuous variables are expressed as means ± standard deviation, and categorical variables as numbers and proportions (%). To compare anemic with non-anemic groups, independent student's t-test was applied to the continuous variables, and Chi-square test to the categorical variables. To prove the relation between anemia and echocardiographic parameters, binary logistic regression was used. A p-value of < 0.05 was considered statistically significant.
Clinical characteristics and intergroup comparison of the study groups are demonstrated in Table 1. The mean of value hemoglobin in the anemic group was 10.85 ± 1.38 g/dL and 14.19 ± 1.24 g/dL in the non-anemic group. Age, gender, body mass index (BMI), systolic blood pressure, and heart rate were largely comparable between the groups. Chronic renal failure (CRF) was more prevalent (5.4% vs. 37.2%, p < 0.001) and diastolic blood pressure (BP) was higher in anemia patients (86.63 ± 12.25 mmHg vs. 89.85 ± 11.34 mmHg).
The echocardiographic measurements are shown in Table 2. LV mass index (115.27 ± 34.95 vs. 103.75 ± 28.21 g/m2, p = 0.033) and LA volume index were (29.31 ± 10.74 vs. 24.99 ± 7.43 mL/m2, p = 0.020) significantly larger in the anemic group. LV dimensions and ejection fraction did not differ between the two groups. E velocity and E/E' (11.92 ± 4.34 vs. 9.37 ± 2.51) were higher in the anemic group than in the non-anemic group (p < 0.001). There were no significant differences in peak E' velocity, E/A ratio, deceleration time, peak E' velocity, or peak A' velocity. Stroke volume and cardiac index did not differ between the groups.
To determine the associated factors with anemia, binary logistic regression analysis was performed (Table 3). On multivariate logistic analysis, anemia was significantly correlated with the presence of CRF and LV filling pressure, reflected by E/E', even after controlling LV mass index and LA volume index. Furthermore, E/E' was significantly correlated with hemoglobin level (R2 = 0.093, p < 0.001) (Fig. 1).
The principal findings of this study are; in hypertensive patients over 50 year-old, (1) the presence of anemia was associated with elevation in E/E', which reflects the increase of LV filling pressure and (2) E/E' was negatively correlated with hemoglobin level.
Anemia is highly prevalent in heart failure patients and is strongly associated with systolic dysfunction.14) Anemia is a known to be a risk factor for cardiovascular disease, even in the low-risk population.8) Nair et al.7) reported that anemia was strongly associated with diastolic dysfunction in outpatients who had coronary artery disease and preserved systolic function assessed by mitral inflow pattern. Even in the absence of left ventricular hypertrophy or renal insufficiency, anemia remained strongly associated with diastolic dysfunction.
In our study, anemic patients had characteristic features compared with non-anemic patients. Anemic patients showed higher LV mass index than non-anemic patients. Increased LV mass has been reported in a few previous studies, such as studies in sickle cell anemia patients,15) and patients with hemoglobin levels < 8 g/dL.16) It is interesting that even though the degree of anemia was not so severe in this study compared with previous studies. LV hypertrophy was more prominent in the anemic group. Therefore, we can speculate that LV geometric remodeling may occur earlier than previously expected.
LA volume index and E/E' are important parameter of diastolic dysfunction. E/E' ratio is used as an initial estimation of the LV filling pressure, particularly in patients with preserved systolic function. LA volume can be viewed as a morphologic expression of chronic increased LV filling pressure results in remodeling. The multivariable logistic analysis showed that anemia was negatively related E/E' ratio even after adjusting for LV mass index, LA volume index and the presence of CRF. Needless to say, CRF was strongly associated with the presence of anemia, as expected. However, a more significant finding in this study is the relationship between anemia and LV filling pressure, even after controlling for the presence of CRF. Therefore, our results suggest that anemia may be an important mediator in the pathway from diastolic dysfunction to heart failure in hypertensive patients regardless of renal insufficiency.
There are possible explanations for these findings between anemia and diastolic dysfunction in hypertensive patients. Low hemoglobin reduces systemic vascular resistance as a result of blood viscosity and enhanced nitric oxide-mediated vasodilation. This vasodilation lowers the blood pressure and subsequently stimulates the baroreceptor mediated neurohormonal activation. Adaptation to an anemic state involves augmentation of the cardiac index and stroke volume.17) This overall increase in sympathetic and inotropic activity places additional stress on the myocardium, perhaps leading to remodeling of the myocytes and vasculature and possible aggravation of vascular damages in hypertensive patients. In addition, studies on the coronary blood flow in anemic patients have shown a decrease in myocardial oxygen consumption, despite an increase in myocardial workload and oxygen extraction.18) Oxygen demand and supply mismatch can lead to myocardial ischemia and result in diastolic dysfunction.
The present study has certain limitations that need to be taken into account. First, this is a cross-sectional study, so we cannot present the long term follow-up data or the result after correction of anemia. Recent studies indirectly support the benefit of treating mild anemia in high risk hypertensive patients with chronic heart failure and chronic kidney disease.19) Second, because the duration and severity of hypertension are not known in the patient group, the influence of these factors on LV mass and diastolic function cannot be assessed in this study. Third, due to the relatively small number of study subjects, the effect of other associated risk factors including obesity and advanced age cannot be clearly elucidated. However, age and BMI were not different between the anemic and non-anemic patients and in multivariate logistic analysis, LV filling pressure was demonstrated to significantly associated with anemia even after adjusting for renal insufficiency. Finally, because our participants were composed of newly diagnosed hypertensive patients, these results may not be applied uncritically to other disease groups.
Figures and Tables
Fig. 1
Relation of Hemoglobin levels with corresponding E/E' values, reflecting LV filling pressure, in hypertensive patients over 50 year-old. E/E': the ratio of early transmitral inflow to septal diastolic velocity of the mitral annulus.
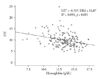
Table 2
Comparison of echocardiographic parameters between anemic and non-anemic patients

*p < 0.05. LVEDD: left ventricular end-diastolic diameter, LVESD: left ventricular end-systolic diameter, SWT: septal wall thickness, PWT: posterior wall thickness, LVMI: left ventricular mass index, LAD: left atrail diameter, LAVI: left atrial volume index, EF: ejection fraction, E: mitral early diastolic, A: mitral late diastolic, DT: deceleration time of mitral inflow velocity, E': mitral annular early diastolic, A': mitral annular late diastolic, E/E': the ratio of early transmitral inflow to septal diastolic velocity of the mitral annulus
References
1. Maeder MT, Kaye DM. Heart failure with normal left ventricular ejection fraction. J Am Coll Cardiol. 2009. 53:905–918.

2. Rakusan K, Cicutti N, Kolar F. Effect of anemia on cardiac function, microvascular structure, and capillary hematocrit in rat hearts. Am J Physiol Heart Circ Physiol. 2001. 280:H1407–H1414.

3. Amin MG, Tighiouart H, Weiner DE, Stark PC, Griffith JL, MacLeod B, Salem DN, Sarnak MJ. Hematocrit and left ventricular mass: the Framingham Heart study. J Am Coll Cardiol. 2004. 43:1276–1282.

4. Slama M, Susic D, Varagic J, Frohlich ED. Diastolic dysfunction in hypertension. Curr Opin Cardiol. 2002. 17:368–373.

5. Bella JN, Palmieri V, Liu JE, Kitzman DW, Oberman A, Hunt SC, Hopkins PN, Rao DC, Arnett DK, Devereux RB. Hypertension Genetic Epidemiology Network Study Group. Relationship between left ventricular diastolic relaxation and systolic function in hypertension: The Hypertension Genetic Epidemiology Network (HyperGEN) Study. Hypertension. 2001. 38:424–428.

6. Srivastava PM, Thomas MC, Calafiore P, Macisaac RJ, Jerums G, Burrell LM. Diastolic dysfunction is associated with anemia in patients with Type II diabetes. Clin Sci (Lond). 2006. 110:109–116.

7. Nair D, Shlipak MG, Angeja B, Liu HH, Schiller NB, Whooley MA. Association of anemia with diastolic dysfunction among patients with coronary artery disease in the Heart and Soul Study. Am J Cardiol. 2005. 95:332–336.

8. Sarnak MJ, Tighiouart H, Manjunath G, MacLeod B, Griffith J, Salem D, Levey AS. Anemia as a risk factor for cardiovascular disease in The Atherosclerosis Risk in Communities (ARIC) study. J Am Coll Cardiol. 2002. 40:27–33.

9. Iron Deficiency Anaemia. Assessment, Prevention and Control. A Guide for Programme Managers. Document WHO/NHD/01.3. 2001. Geneva: World Health Organization.
10. Lang RM, Bierig M, Devereux RB, Flachskampf FA, Foster E, Pellikka PA, Picard MH, Roman MJ, Seward J, Shanewise JS, Solomon SD, Spencer KT, Sutton MS, Stewart WJ. Chamber Quantification Writing Group. American Society of Echocardiography's Guidelines and Standards Committee. European Association of Echocardiography. Recommendations for chamber quantification: a report from the American Society of Echocardiography's Guidelines and Standards Committee and the Chamber Quantification Writing Group, developed in conjunction with the European Association of Echocardiography, a branch of the European Society of Cardiology. J Am Soc Echocardiogr. 2005. 18:1440–1463.

11. Devereux RB, Alonso DR, Lutas EM, Gottlieb GJ, Campo E, Sachs I, Reichek N. Echocardiographic assessment of left ventricular hypertrophy: comparison to necropsy findings. Am J Cardiol. 1986. 57:450–458.

12. Benjamin EJ, D'Agostino RB, Belanger AJ, Wolf PA, Levy D. Left atrial size and the risk of stroke and death. The Framingham Heart Study. Circulation. 1995. 92:835–841.
13. Ren JF, Kotler MN, DePace NL, Mintz GS, Kimbiris D, Kalman P, Ross J. Two-dimensional echocardiographic determination of left atrial emptying volume: a noninvasive index in quantifying the degree of nonrheumatic mitral regurgitation. J Am Coll Cardiol. 1983. 2:729–736.

14. Horwich TB, Fonarow GC, Hamilton MA, MacLellan WR, Borenstein J. Anemia is associated with worse symptoms, greater impairment in functional capacity and a significant increase in mortality in patients with advanced heart failure. J Am Coll Cardiol. 2002. 39:1780–1786.

15. Lester LA, Sodt PC, Hutcheon N, Arcilla RA. Cardiac abnormalities in children with sickle cell anemia. Chest. 1990. 98:1169–1174.

16. Caldas MC, Meira ZA, Barbosa MM. Evaluation of 107 patients with sickle cell anemia through tissue Doppler and myocardial performance index. J Am Soc Echocardiogr. 2008. 21:1163–1167.

17. Anand IS. Anemia and chronic heart failure implications and treatment options. J Am Coll Cardiol. 2008. 52:501–511.
18. Bahl VK, Malhotra OP, Kumar D, Agarwal R, Goswami KC, Bajaj R, Shrivastava S. Noninvasive assessment of systolic and diastolic left ventricular function in patients with chronic severe anemia: A combined M-mode, two-dimensional, and Doppler echocardiography study. Am Heart J. 1992. 124:1516–1523.

19. Olsen MH, Wachtell K, Beevers G, Dahlöf B, Devereux RB, de Faire U, Fyhrquist F, Ibsen H, Kjeldsen SE, Lederballe-Pedersen O, Lindholm LH, Narayan P, Nieminen MS, Omvik P, Oparil S, Wedel H. Prognostic importance of hemoglobin in hypertensive patients with electrocardiographic left ventricular hypertrophy: the Losartan Intervention For End point reduction in hypertension (LIFE) study. Am Heart J. 2009. 157:177–184.





 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download