Abstract
Background
The aim of this study was to evaluate the mid-term changes in cardiac function by transthoracic echocardiogram (TTE) in patients with ST-segment elevation myocardial infarction (STEMI) undergoing primary percutaneous coronary intervention (PCI) according to valsartan dose.
Methods
Between April 2006 and February 2009, 78 subjects (mean age: 57 ± 12 years, M : F = 74 : 4) with STEMI who underwent primary PCI were enrolled. Fifty three patients received low dose valsartan (40 or 80 mg) and 25 patients received high dose valsartan (160 or 320 mg). Follow-up TTE was done approximately 2 years later. We evaluated the changes in left ventricular (LV) function between initial and final TTE after primary PCI and compared the changes between low and high dose valsartan group.
Results
The mean follow-up TTE duration was 24 ± 8 months. Deceleration time (188.6 ± 56.3 msec vs. 221.5 ± 71.3 msec, p = 0.01), E/e' (12.24 ± 5.2 vs. 10.1 ± 4.9, p = 0.002), ejection fraction (52.7 ± 8% vs. 55.2 ± 8.4%, p < 0.01), and wall motion score index (1.45 ± 0.30 vs. 1.33 ± 0.32, p < 0.01) showed significant changes during the follow-up period. Wall motion improvement in injured myocardial segments was more frequently observed in the high-dose valsartan group compared to the low-dose group [18/25 (72%) vs. 24/53 (43.7%), p = 0.03]. There was no significant difference in the changes in cardiac dimensions and function between the low and high dose valsartan group.
Acute myocardial infarction (MI) is frequently associated with left ventricular (LV) remodeling leading to progressive heart failure (HF). LV remodeling after acute MI is an important predictor of mortality.1)2) The mechanisms of the development of HF are not simple, involving changes in LV chamber size and geometry, as well as hemodynamic changes leading to overall decreased cardiac pump performance.3) About 20% of patients with acute MI developed decompensated remodeling and develop HF.4) Angiotensin converting enzyme (ACE) inhibitors and angiotensin receptor blockers (ARBs) have been shown to benefit patients after acute MI. Inhibition of the renin-angiotensin-aldosterone system prevents both LV remodeling and the transition from a compensatory HF to decompensated state after MI.5-7) In large-scale randomized trials, ARBs and ACE inhibitors were effective in suppressing cardiac events in MI patients with compromised LV function.8)9) However, there are few long-term data on follow-up transthoracic echocardiography (TTE) in patients with ST-elevation myocardial infarction (STEMI) who received primary percutaneous coronary intervention (PCI) according to ARBs dose. The aim of this study was to evaluate and compare the mid-term changes in LV wall thickness, dimensions, cardiac function and viable myocardium by TTE in subjects to whom different doses of valsartan were administered.
We prospectively studied 78 patients with STEMI among 136 patients consecutively referred to our catheterization laboratory for emergency PCI between April 2006 and February 2009. The study inclusion criteria were as follows: (1) confirmed STEMI, (2) successful primary PCI [defined as thrombolysis in myocardial infarction trial (TIMI) flow grade 3 and residual stenosis of the infarct-related artery (IRA) < 30%] performed within 90 minutes of door to balloon time or over 90 minutes of door to balloon time in patients with ongoing chest pain or dynamic ST change. (3) Informed consent to perform echocardiography at least at 2 prospectively defined points in time, (4) age > 18 years old. No upper age limit was used. Exclusion criteria were (1) IRA diameter stenosis < 70% with TIMI grade 3 flow or inability to identify IRA, (2) clinical signs of HF or cardiogenic shock, (3) significant other cardiac disease, (4) stroke within the last 3 months, (5) life-limiting noncardiac disease, and (6) contraindication to ARBs use. Of the 136 patients initially selected for the study, 20 (14.7%) did not adhere to follow-up TTE protocol, 10 (7.4%) were excluded for inadequate TTE image quality, and 26 (19.1%) were also excluded due to change of medication to other ARBs because of noncompliance and hypotension. Thus, 78 patients represented the final study group. The study design was shown in Fig. 1. This study was approved by our Institutional Review Committee. The participants were informed of the investigative nature of the study and written informed consent was obtained before enrollment (UCMC06MM005).
Eligible patients were randomly assigned to either the low-dose valsartan group (40 or 80 mg once a day orally) or high-dose valsartan group (160 or 320 mg once a day orally) with group assignments concealed. The study drug was initiated at a dose of 40 mg daily in the low-dose group, and 80 mg daily in the high-dose group for 2 weeks. The dose was then increased to 80 mg daily in the low-dose group and to 160 mg daily in the high-dose group for another 2 weeks. At the 4th week, the dose was increased to 320 mg daily in the high-dose group, and in the low-dose group the study drug dose was not changed. Upward adjustment of the dose of the study medication was required for all patients unless they presented with a blood pressure below 110/70 mmHg or symptomatic hypotension. If the patient could not tolerate a dose of 40 mg (low-dose group) or 160 mg (high-dose group) of the study drug within 2 months after enrollment, the study drug was withdrawn. PCI was performed according to current practice guidelines, and standard medication of STEMI was given to all enrolled patients.
Study visits were scheduled at 2, 4, 8, 24, 48, 72, and 96 weeks with the follow-up period concluding at 2 years. A routine clinical examination including chest X-ray, TTE and laboratory testing was performed at admission. Serial TTE were performed in each patient within 24 hours at 1, 3, 6, 12, and 24 months after STEMI with commercially available machines (GE VIVID 7, 2.4 MHz: GE Medical Systems, Milwaukee, WI, USA).
2D images were obtained by use of standard views in the left lateral decubitus position. Images were captured in digital format into a cine loop display, and stored to Image-Arena 2.9 (Tomtec imaging systems, Unterschleissheim, Germany) for analysis. LV wall thickness, LV dimensions, fractional shortening, and wall motion score index (WMSI) were obtained in standard views. LV end-systolic and end-diastolic volumes were calculated with the modified biplane Simpson's method and if the two-chamber images were inadequate, a single-plane measurement was made in the apical four-chamber view. Ejection fraction (EF) was calculated from the LV end-systolic and end-diastolic volumes. Pulsed wave Doppler tissue images of the basal septum and lateral walls were acquired by placement of sample volumes at the mitral annulus after acquisition of the 2D images. Pulsed wave Doppler of mitral inflow was obtained in the apical four-chamber view. Regional wall motion was analyzed using the 16-segment model. Regional wall function was semiquantitated using a five-grade scoring system (1: normal, 2: mild to moderate hypokinesia, 3: severe hypokinesia, 4: akinesia, 5: dyskinesia). Improvement in injured myocardium was defined as increase in wall motion score of ≥ 1 grade in more than 2 injured myocardial segments at follow-up TTE. WMSI was derived as the sum of individual scores divided by the total number of segments analyzed. E/e' (average) was defined as the sum of E/e' (septal) and E/e' (lateral) divided by two. The follow-up TTE images were reviewed by 2 independent cardiologists to ascertain the improved wall motion and the parameters of TTE.
Continuous data are expressed as mean ± SD. Baseline data were compared by means of χ2 test or Fisher's exact test for categorical variables and Mann-Whitney U test and Wilcoxon matched-pairs signed-rank test for continuous variables. Univariate and multivariate logistic regression analyses were performed to identify independent predictors of wall motion improvement. Statistical analyses were performed with the SAS statistical software version 9.1 (SAS Institute, Cary, NC, USA) for Windows. A value of p < 0.05 was considered statistically significant.
All 78 patients (male : female ratio = 74 : 4, mean age 57 ± 12 years) with STEMI undergoing primary PCI. Twenty nine patients (37%) had a history of hypertension, 16 patients (21%) had a history of diabetes mellitus, and 45 patients (58%) were smokers. The infarct-related arteries were: left anterior descending artery, 40 (51%): right coronary artery, 32 (41%); and left circumflex artery, 6 (8%). Forty three patients (55%) had 1 vessel disease, 25 patients (32%) had 2 vessel disease, and 10 patients (13%) had 3 vessel disease. Mean door to balloon time was 1.3 ± 0.9 hours.
Fifty-three patients (40 : 80 mg ratio = 8 : 45, mean dose 73.9 ± 14.5 mg) were enrolled to the low-dose group and 25 patients (160 : 320 mg ratio = 21 : 4, mean dose 176 ± 73.1 mg) to the high-dose group according to valsartan dose. The clinical characteristics of patients according to valsartan dose were shown in Table 1.
Table 2 shows TTE findings between initial and final follow-up TTE. The mean TTE follow-up duration was 24 ± 8 months. WMSI and E/e' (average) decreased significantly at final follow-up (WMSI: 1.45 ± 0.30 vs. 1.33 ± 0.32, p < 0.01; E/e': 12.2 ± 5.2 vs. 10.1 ± 4.9, p < 0.01). Ejection fraction and deceleration time increased significantly at final follow-up (ejection fraction: 52.7 ± 8.1% vs. 55.2 ± 8.4%, p < 0.01; 189 ± 56 ms vs. 222 ± 71 ms, p < 0.01).
Table 3 shows the changes of TTE parameters according to valsartan dose. There were no significant difference in the changes of TTE parameters between the low-dose valsartan group and the high-dose valsartan group including WMSI (-0.12 ± 0.22 vs. -0.17 ± 0.20, p = 0.25), E/e' (average) (-1.4 ± 5.3 vs. -1.8 ± 4.2, p = 0.75), ejection fraction (2.1 ± 8.4% vs. 3.9 ± 8.4%, p = 0.38), and deceleration time (33 ± 84 ms vs. 44 ± 79 ms, p = 0.60).
Wall motion improvement in more than 2 segments of injured myocardium by ≥ 1 grade was identified in a significantly higher proportion in the high-dose valsartan group than the low-dose valsartan group [18/25 (72.0%) vs. 24/53 (43.7%), p = 0.03] (Fig. 2). In multivariate regression analysis, EF was an independent TTE parameter for predictability of wall motion improvement of more than 2 segments of injured myocardium by ≥ 1 grade after valsartan treatment in patients with STEMI who underwent primary PCI [odd ratio: 1.078, 95% confidence interval: (1.008-1.154), p = 0.029] (Table 4).
In this study, high-dose valsartan treatment in patients with STEMI who received primary PCI led to more favorable improvement in regional wall motion abnormalities of the injured myocardium than low-dose valsartan treatment in midterm follow-up duration. However, it remains doubtful whether high-dose valsartan treatment will be superior to low-dose in preventing LV remodeling of injured myocardium.
A small study reported that antihypertensive treatment did not change LV mass, LV morphology.10) Two large randomized clinical studies-the OPTIMAAL and VALIANT trials-have been performed to compare the usefulness of ACE inhibitors and ARBs for secondary prevention of MI.8)9) Neither of the trials revealed any statistically significant differences in the incidence of death from HF between patients treated with ACE inhibitors and those treated with ARBs. In other words, ARBs were not inferior to ACE inhibitors in preventing LV remodeling. To elucidate favorable effects of high- or low-dose valsartan on preventing LV remodeling in patients with STEMI who underwent primary PCI, more long-term data are warranted.
Meanwhile, Tani et al.11) reported that use of losartan in patients with STEMI resulted in a higher LVEF at 6 months than baseline, which is in concordance with the results of our study. Results of large studies suggest that early treatment with ACE inhibitors is superior to late initiation and treatment with ACE inhibitors started within 24 hours of the onset of MI is ideal.5)12)13) In contrast, in previous large-scale clinical studies on the effect of ARBs on MI, drugs were not administered during the very early stage after the onset of MI. ARBs were administered at a median of 3 days after the onset of MI in the OPTIMAAL and at mean 4.9 days after the onset of MI in the VALIANT study. As our study was designed to administer the ARB within 24-48 hours after PCI, there is a time difference in initiation of ACE inhibitors or ARBs between our results and previous large-scale studies. The difference of our results from the above studies might have resulted from this factor, but further investigations are required in larger multicenter trials in the future.
In the VALIANT sub-study that evaluated the TTE results, treatment in patients with MI and LV dysfunction with captopril (50 mg twice a day orally), valsartan (160 mg twice a day orally), or the combination of captopril (50 mg 3 times a day orally) plus valsartan (80 mg twice a day orally) resulted in similar changes in cardiac volume, ejection fraction, and infarct segment length between baseline and 20 months after MI.14) This is partly in concordance with the results of our study, which show that there were no significant differences in change of cardiac volume, EF, WMSI, and diastolic function between groups who received low- or high-dose of valsartan. This result suggests that the efficacy of suppressing LV remodeling is equivalent between low and high dose of valsartan. There are several recent imaging studies addressing LV remodeling after acute MI. Rim et al.15) reported that dobutamine stress echocardiography can be a useful tool for the prediction of LV remodeling after acute MI, and some experimental studies have suggested that inflammatory response is a key component of post-MI LV remodeling.16-18) Monocyte chemoattractant protein-1 (MCP-1) is known to make a major contribution to the pathogenic role of inflammation in cardiovascular disease. The expression of MCP-1 in the myocardium increases during the early stage of MI19)20) and deletion or inhibition of MCP-1 prevents early post-MI LV remodeling.21)22) Kohno et al.23) reported that In post-MI HF, ARBs attenuated MCP-1 expression and macrophage infiltration in the border zone, resulting in less myocardial fibrosis and ARBs may exert its beneficial effect, at least in part, by inhibiting myocardial macrophage-related inflammation. In the present study, administration of high-dose valsartan resulted in a higher frequency of patients with improved wall motion segments in the injured myocardium compared to low dose. This result suggests that higher-dose of ARBs may be needed to inhibit myocardial macrophage-related inflammation and prevent further tissue injury and fibrosis in the border zone myocardium more effectively. To explain these facts, further investigations are required.
There are several limitations in the present study. First, the proportion of dropout was higher in the high-dose valsartan group than the low-dose valsartan group because of non-compliance or side effects such as hypotension. This may be comparable to the results of the VALIANT study, where the proportion of patients taking the target doses in valsartan group was 56% at the end of the study.9) Second, in the present study, major cardiovascular events such as death, MI, target vessel revascularization, and stroke were not evaluated, according to valsartan dose, which may limit its value for clinical implication.
Figures and Tables
Fig. 1
Study design. STEMI: ST-segment elevation myocardial infarction, PCI: percutaneous coronary intervention, BP: blood pressure, TTE: transthoracic echocardiography.

Fig. 2
Comparison of the percent of patients according to improvement of wall motion in the injured myocardium between low- and high-dose valsartan groups
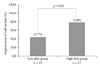
Table 2
The change of transthoracic echocardiography (TTE) parameters between initial and final follow-up TTE

Table 4
Multivariate regression analysis

Ejection fraction shows an independent transthoracic echocardiographic parameter for predictability of wall motion improvement of more than 2 segments of injured myocardium by ≥ 1 grade after valsartan treatment in subjects with ST-segment elevation myocardial infarction who underwent primary percutaneous coronary intervention
Acknowledgements
The present study was supported by grants from the Korean Society of Echocardiography (2007).
References
1. Pfeffer MA, Braunwald E. Ventricular remodeling after myocardial infarction, Experimental observations and clinical implications. Circulation. 1990. 81:1161–1172.

2. St John Sutton M, Pfeffer MA, Plappert T, Rouleau JL, Moyé LA, Dagenais GR, Lamas GA, Klein M, Sussex B, Goldman S, et al. Quantitative two-dimensional echocardiographic measurements are major predictors of adverse cardiovascular events after acute myocardial infarction. The protective effects of captopril. Circulation. 1994. 89:68–75.

4. Gaudron P, Eilles C, Kugler I, Ertl G. Progressive left ventricular dysfunction and remodeling after myocardial infarction. Potential mechanisms and early predictors. Circulation. 1993. 87:755–763.

5. Pfeffer MA, Braunwald E, Moyé LA, Basta L, Brown EJ Jr, Cuddy TE, Davis BR, Geltman EM, Goldman S, Flaker GC, et al. The SAVE Investigators. Effect of captopril on mortality and morbidity in patients with left ventricular dysfunction after myocardial infarction. Results of the survival and ventricular enlargement trial. N Engl J Med. 1992. 327:669–677.

6. Harada K, Sugaya T, Murakami K, Yazaki Y, Komuro I. Angiotensin II type 1A receptor knockout mice display less left ventricular remodeling and improved survival after myocardial infarction. Circulation. 1999. 100:2093–2099.

7. Patel AR, Konstam MA. Recent advances in the treatment of heart failure. Circ J. 2002. 66:117–121.

8. Dickstein K, Kjekshus J. OPTIMAAL Steering Committee of the OPTIMAAL Study Group. Effects of losartan and captopril on mortality and morbidity in high-risk patients after acute myocardial infarction: the OPTIMAAL randomised trial. Optimal Trial in Myocardial Infarction with Angiotensin II Antagonist Losartan. Lancet. 2002. 360:752–760.

9. Pfeffer MA, McMurray JJ, Velazquez EJ, Rouleau JL, Køber L, Maggioni AP, Solomon SD, Swedberg K, Van de Werf F, White H, Leimberger JD, Henis M, Edwards S, Zelenkofske S, Sellers MA, Califf RM. Valsartan in Acute Myocardial Infarction Trial Investigators. Valsartan, captopril, or both in myocardial infarction complicated by heart failure, left ventricular dysfunction, or both. N Engl J Med. 2003. 349:1893–1906.

10. Kim YS, Cho HK, Chung IM, Park SH, Park SH, Shin GJ. Changes in LV mass, LV morphology and diastolic function of LV in response to antihypertensive treatment. J Korean Soc Echocardiogr. 1997. 5:154–163.

11. Tani S, Nagao K, Anazawa T, Kawamata H, Furuya S, Takahashi H, Iida K, Matsumoto M, Kumabe N, Onikura M, Hirayama A. Effects of enalapril and losartan in left ventricular remodeling after acute myocardial infarction: a possible mechanism of prevention of cardiac events by angiotensin-converting enzyme inhibitors and angiotensin receptor blockers in high-risk myocardial infarction. Intern Med. 2009. 48:877–882.

12. ISIS-4 (Fourth International Study of Infarct Survival) Collaborative Group. ISIS-4: a randomised factorial trial assessing early oral captopril, oral mononitrate, and intravenous magnesium sulphate in 58,050 patients with suspected acute myocardial infarction. Lancet. 1995. 345:669–685.
13. Gruppo Italiano per lo Studio della Sopravvivenza nell'infarto Miocardico. GISSI-3: effects of lisinopril and transdermal glyceryl trinitrate singly and together on 6-week mortality and ventricular function after acute myocardial infarction. Lancet. 1994. 343:1115–1122.
14. Solomon SD, Skali H, Anavekar NS, Bourgoun M, Barvik S, Ghali JK, Warnica JW, Khrakovskaya M, Arnold JM, Schwartz Y, Velazquez EJ, Califf RM, McMurray JV, Pfeffer MA. Changes in ventricular size and function in patients treated with valsartan, captopril, or both after myocardial infarction. Circulation. 2005. 111:3411–3419.

15. Rim SJ, Chung NS, Lee NH, Goh CW, Ha JW, Kim JY, Oh EK, Ahn SK, Kim TY, Lee MH, Jang YS, Shim WH, Cho SY, Kim SS. Dobutamine echocardiography in the prediction of left ventricular remodeling after acute myocardial infarction. J Korean Soc Echocardiogr. 1997. 5:85–93.

16. Frangogiannis NG, Smith CW, Entman ML. The inflammatory response in myocardial infarction. Cardiovasc Res. 2002. 53:31–47.

17. Anzai T, Yoshikawa T, Shiraki H, Asakura Y, Akaishi M, Mitamura H, Ogawa S. C-reactive protein as a predictor of infarct expansion and cardiac rupture after a first Q-wave acute myocardial infarction. Circulation. 1997. 96:778–784.

18. Maekawa Y, Anzai T, Yoshikawa T, Sugano Y, Mahara K, Kohno T, Takahashi T, Ogawa S. Effect of granulocyte-macrophage colony-stimulating factor inducer on left ventricular remodeling after acute myocardial infarction. J Am Coll Cardiol. 2004. 44:1510–1520.

19. Kumar AG, Ballantyne CM, Michael LH, Kukielka GL, Youker KA, Lindsey ML, Hawkins HK, Birdsall HH, MacKay CR, LaRosa GJ, Rossen RD, Smith CW, Entman ML. Induction of monocyte chemoattractant protein-1 in the small veins of the ischemic and reperfused canine myocardium. Circulation. 1997. 95:693–700.

20. Hayasaki T, Kaikita K, Okuma T, Yamamoto E, Kuziel WA, Ogawa H, Takeya M. CC chemokine receptor-2 deficiency attenuates oxidative stress and infarct size caused by myocardial ischemia-reperfusion in mice. Circ J. 2006. 70:342–351.

21. Hayashidani S, Tsutsui H, Shiomi T, Ikeuchi M, Matsusaka H, Suematsu N, Wen J, Egashira K, Takeshita A. Anti-monocyte chemoattractant protein-1 gene therapy attenuates left ventricular remodeling and failure after experimental myocardial infarction. Circulation. 2003. 108:2134–2140.





 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download