Abstract
Background
It remains unclear whether myocardial contrast echocardiography (MCE) is as accurate as myocardial perfusion imaging with technetium-99m sestamibi (MPI) for the diagnosis of acute coronary syndrome (ACS). We sought to directly compare the diagnostic accuracy of MCE with resting MPI in a head-to-head fashion.
Methods
We prospectively enrolled 98 consecutive patients (mean age; 59±9 years, 68 males) who presented to the emergency department with chest pain suggestive of acute myocardial ischemia. Early MCE was performed by using continuous infusion of perfluorocarbon-exposed sonicated dextrose albumin (PESDA) during intermittent power Doppler harmonic imaging. Myocardial perfusion defects observed in at least one coronary territory were considered positive. Sestamibi was injected immediately after MCE and MPI was obtained within 6 hours of tracer injection.
Results
ACS was confirmed in 67 patients. There were 32 patients with acute myocardial infarction (AMI) and 35 patients with unstable angina requiring urgent revascularization. The sensitivities of MCE and MPI for the diagnosis of ACS were 72% and 61%, respectively, which were significantly higher than those of ST segment change (24%, p<0.001 vs. MCE and vs. MPI) and troponin I (27%, p<0.001 vs. MCE and vs. MPI), with similar specificities of 90% to 100%. On a receiveroperating characteristics curve demonstrating diagnostic accuracy for ACS, the area under the curve of MCE was significantly larger than that of MPI (0.86 vs. 0.77, respectively; p=0.019).
Rapid and accurate diagnosis is essential for optimal management of patients with acute coronary syndrome (ACS). However, the diagnostic process remains problematic in patients presenting to the emergency room with possible myocardial ischemia but without typical electrocardiogram (ECG) changes or elevation of cardiac biomarkers.1-3) Although troponin I has been considered to be the best prognostic marker in patients with ACS, the diagnosis of unstable angina is not based on the elevation of serum cardiac biomarkers and the initial negative result of troponin I cannot exclude the possibility of ACS. In this clinical setting, myocardial perfusion imaging (MPI) with technetium-99m sestamibi, which reflects myocardial blood flow at the time of ongoing chest pain, has the potential to detect ACS more sensitively than serum biomarkers or ECG.4) MPI has been reported to have a high sensitivity for identification of acute myocardial ischemia or infarction, and recommended for selected patients suspected to have ACS but without specific abnormalities on routine triage tests.5)6)
Myocardial contrast echocardiography (MCE) is an emerging technique that permits rapid assessment of both regional function and perfusion at the bedside, in real-time, with a better temporal and spatial resolution than MPI.7-10) It is unclear, however, whether MCE is as accurate as MPI for the diagnosis of ACS including unstable angina and non-ST elevation myocardial infarction in patients presenting to the emergency room. This study was conducted 1) to determine whether early MCE and MPI are superior to the initial level of troponin I and the ECG criteria for the diagnosis of ACS in high-risk chest pain patients and 2) to directly compare the diagnostic accuracy of MCE with resting MPI in a head-to-head study.
We prospectively enrolled 98 consecutive patients who presented to the emergency department during daytime hours with resting chest pain suggestive of myocardial ischemia. Exclusion criteria were age <40 years or >75 years, pregnancy, presence of Q wave or ST-segment elevation, history of myocardial infarction and poor echocardiographic window. Informed consent was obtained from all patients and the study protocol was approved by the ethical committee of our institution.
All patients underwent cardiac biomarkers (creatine kinase-MB, troponin I) determinations and 12-lead ECG examinations at initial presentation to the emergency department and then followed-up at 6 and 24 hours afterward. The serum level of troponin I was measured by the chemiluminescent assay (CLIA assay), and a value of troponin I >1.5 ng/mL was considered abnormal. The presence of significant ECG change was defined as an ST-segment depression >0.05 mV. After the initial clinical evaluation, MCE was performed and 740 MBq of technetium-99m sestamibi was administered intravenously in the emergency room within 6 hours of presentation. As described previously,11) single-photon emission computed tomographic (SPECT) MPI acquisition occurred within 6 hours of tracer injection. The MCE and MPI results were not reported to the attending physicians, who made disposition decisions based on routine assessment.
A diagnosis of acute myocardial infarction (AMI) was confirmed by the presence of more than two of the following criteria: chest pain consistent with myocardial ischemia, development of Q wave and an increase of serum cardiac biomarkers (creatine kinase-MB >10 IU/L, 2 times the upper limit of the normal value).12)13) The definition of acute coronary syndrome was based on the development of AMI or documentation of significant coronary artery stenosis that required urgent revascularization
To evaluate regional wall motion abnormalities and myocardial perfusion, intravenous MCE was performed in apical 4-, 3-, and 2-chamber views with triggered replenishment imaging using Sonos 5500 instrument (Philips Medical Imaging, Andover, Massachusetts, USA). Intermittent harmonic power Doppler imaging was performed with a broadband harmonic transducer that transmitted and received at mean frequencies of 1.8 and 3.6 MHz, respectively. Emission power was set at the highest level (mechanical index 1.3 to 1.6). Images were obtained by triggering at end-systole. In an attempt to differentiate true perfusion from motion artifact, a dual-frame imaging technique was used. The 2 frames were displayed side by side. One represented the perfusion frame and the other represented the post-destruction frame which was obtained approximately 50 milliseconds later. In the cases of tissue motion artifact, the post-destruction frame showed nearly the same signal intensity as the actual perfusion frame and the motion artifact could easily be recognized.
The contrast agent, perfluorocarbon-exposed sonicated dextrose albumin (PESDA),14) was intravenously administered as a continuous infusion of 0.05 mL/kg in 30 mL of normal saline at a rate of 0.8 to 3 mL/min. The Doppler gain setting and infusion rate of a contrast agent were adjusted to maximize the left ventricular cavity signal without causing attenuation artifacts in the destruction-phase image. If a myocardial defect was noted in the perfusion image after a pulsing interval of 4 to 6 beats, the triggering interval was increased to every eighth or tenth beats.15) The focus was set at the level of the mitral annulus and was moved to an appropriate level when necessary. According to each coronary artery territory, the position of the transducer was adjusted to locate the region of interest in the center of the image sector, and MCE was repeated by adjusting the triggering interval. If perfusion defects were consistent with a typical ischemic territory of a coronary artery, observed in the subendocardial area, or associated with wall motion abnormalities of the same area, or if the severity of perfusion defects improved according to the lengthening triggering interval, perfusion defects were regarded as true myocardial perfusion defects and not artifacts.16) Myocardial perfusion defects present in at least one coronary territory were considered positive (Fig. 1A). MCE results were interpreted by different reviewers blinded to the clinical data.
As soon as possible after MCE, all patients underwent resting MPI with technetium-99m sestamibi. For SPECT imaging, 64 projections were obtained for 20 seconds, each at >180° using a dual-head rotating gamma camera. Image reconstruction was performed using standard back-projection algorithms. Short-axis slices of the left ventricles were normalized to peak heart rate. Circumferential count profiles were generated for five short-axis slices from apex to base. Scintigraphic results were analyzed by an experienced nuclear medicine physicians who were blinded to patients' clinical and laboratory data. Perfusion images were evaluated without gating in 35 (36%) patients and with gating in 63 (64%) patients, allowing assessment of regional function. Positive MPI was defined as a mild or definite perfusion defect on SPECT MPI performed without gating, and a definite perfusion defect with associated abnormality in wall motion and thickening on gated MPI.
Coronary angiography was performed in all patients by standard techniques. Quantitative analysis of coronary angiography was done by experienced investigators using a quantitative analyzer (Ancor 2.0, Siemens, Erlangen, Germany). Significant stenosis that required urgent revascularization was defined as critical stenosis (diameter stenosis ≥90%) with the potential to affect coronary blood flow at rest and stenosis associated with ulceration or thrombus (Fig. 1B).
Continuous variables are presented as mean±SD. Statistical analysis of differences between the groups was performed using the Student's t-test or Mann-Whitney U test, as appropriate. For categorical variables, Chi-square test compared the frequency ratio between groups. The McNemar test was used to compare the sensitivity and specificity of MCE and MPI with those of the ECG and troponin criteria. A receiver-operating characteristics (ROC) curve was plotted to compare the diagnostic accuracy of MCE with MPI using the Delong et al.17) method. A p value <0.05 was considered statistically significant.
All 98 patients with resting chest pain suggestive of myocardial ischemia underwent MCE and resting MPI. The mean age of the studied population was 59±9 years, and 69% of the patients were male, 58% had essential hypertension, 19% had diabetes, 14% had a previous history of coronary artery disease. Twenty patients were positive for troponin I and 19 patients had ST-segment depression on ECG analysis. Of the 98 studied patients, 67 patients were diagnosed with ACS. AMI was confirmed in 32 patients. The infarct was found in territories of the left anterior descending artery in 14 patients, the right coronary artery in 9 patients, and the left circumflex artery in 9 patients. Of these 32 patients, 22 underwent percutaneous coronary intervention and 5 underwent coronary artery bypass graft surgery. One patient who underwent urgent bypass surgery died in hospital. Unstable angina requiring urgent revascularization was identified in 35 patients, 30 of whom underwent revascularization without mortality (PCI for 24 patients, CABG for 6 patients): 5 patients refused surgery. Baseline clinical and laboratory data in the 67 patients with ACS and the 31 patients without ACS are summarized in Table 1. There were significantly more males in the patients with ACS compared with those without ACS (78% vs. 52%, p=0.017), and the ACS patients had significantly higher serum troponin I concentrations (2.4±6.5 vs. 0.4±1.0 ng/mL, p=0.020) than those without ACS.
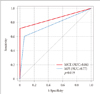
Positive perfusion defects were detected by MCE and MPI in 48 (49%) and 43 (44%) patients, respectively. The sensitivities and specificities of these methods for the diagnosis of ACS and AMI are shown in Table 2. For identifying ACS, MCE and MPI showed higher sensitivities (72% and 61%, respectively) than initial level of troponin I and ECG changes (27% and 24%, respectively; p<0.001 for each), and all methods showed similar specificities of 90% to 100%. The negative predictive values of MCE and MPI for ACS were 62% and 53%, respectively, and the positive predictive values of them were 100% and 95%, respectively. The sensitivities and specificities for the diagnosis of ACS were compared between MCE and MPI according to the analysis method of the MPI study. In the 63 patients who underwent gated MPI, MCE and MPI sensitivities were 78% and 61%, respectively (p=0.09), and both methods had specificities of 100%. In the 35 patients whose MPI results were interpreted without regional function data, both MCE and MPI had sensitivities of 62%, and the specificities were 100% and 78%, respectively (p>0.05). ROC curves for ACS were plotted to compare the diagnostic accuracy of MCE and MPI, and the area under the curve of MCE was significantly larger than that of MPI (0.86 and 0.77, respectively; p=0.019) (Fig. 2). For the diagnosis of AMI, the area under the curve of MCE was similar to that of MPI (0.76 and 0.75, p>0.05).
Quantitative coronary angiograms detected 72 significant lesions that required urgent revascularization. The area under the curve of MCE and MPI was 0.85 and 0.77, respectively, in the territory of the left anterior descending artery, 0.76 and 0.80, respectively, in the right coronary artery, and 0.83 and 0.83, respectively, in the left circumflex artery (p>0.05 for each).
In this study, we confirmed that both MCE and MPI were more accurate than the routinely used troponin I and ECG criteria to detect ACS earlier. In a head-to-head comparison with resting MPI, MCE had a greater diagnostic accuracy for identifying ACS and a similar accuracy for diagnosing AMI.
In the emergency department, patients with symptoms suggestive of acute myocardial ischemia undergo routine triage examinations, including ECG and measurement of cardiac biomarkers, however, these are insufficient to exclude the possibility of ACS.1-3) Although we found that initial troponin I and ECG criteria were highly specific for detecting ACS or AMI, the sensitivities of these methods for ACS were only 27% and 24%, respectively, and the sensitivities for AMI were only 53% and 41%, respectively. This limitation may lead to the inappropriate discharge of patients with real critical ischemia. For patients presenting to the emergency departments with possible ACS but non-diagnostic ECG and normal troponin I levels, the American College of Cardiology/American Heart Association guidelines classify the resting MPI as a class I (level A) indication, partly based on a prospective, randomized controlled trial indicating that MPI may be helpful in determining the management strategy for patients with acute chest pain.6) A previous study has reported that the sensitivity of positive MPI for predicting AMI or revascularization is 81% with a high negative predictive value of 95%.5) Owing to the high-quality images and minimal redistribution after administration, technetium-99m sestamibi can be injected during chest pain, and images obtained a few hours later will reflect myocardial blood flow at the time of injection.4)18) This technique is a validated method for assessing perfusion defects in clinical practice. However, owing to several disadvantages associated with MPI, including the time delay for image acquisition, poor spatial resolution and that it cannot be performed at the bedside, an alternative diagnostic tool is needed for relevant decision making in emergency patients with acute chest pain.
It has been suggested that MCE can offer more useful prognostic information than routine assessment methods in patients with acute chest pain.19)20) We have previously reported that the sensitivity of MCE (77%) for the detection of ACS is significantly higher than that of ECG change (28%), troponin I (34%) and regional wall motion abnormalities (49%), with similar specificities of 85% to 96%.16) Although a prospective, multicenter study comparing MCE with resting technetium-99m sestamibi MPI found a 77% concordance between these two methods, suggesting both may be useful in diagnosing adverse cardiac events, their diagnostic accuracy in perfusion assessment was not compared.20) In addition, unstable angina was excluded in evaluating events. In contrast, we directly compared the diagnostic accuracy of initial MCE with that of resting MPI for identifying ACS, including both unstable angina and AMI. In a head-to-head comparison, we found that MCE could diagnose ACS more accurately than MPI in emergency-department patients with potential cardiac ischemia. For diagnosis of AMI, MCE also showed good sensitivity and specificity, similar to those of MPI. The perfusion defects observed in MCE could be differentiated from artifacts by adjusting the triggering intervals, analyzing patterns of defects and interpreting defects in the context of regional wall motion. SPECT imaging could be performed with standardized protocols and quantitative analysis of perfusion defects, but the severity and extent of resting perfusion defects was often mild in ACS and indistinguishable from attenuation artifacts, resulting in a lower diagnostic accuracy of MPI. Early MCE overcame the limitation of the low sensitivity of baseline cardiac enzymes and ECG criteria for ACS, and complemented the diagnostic accuracy of conventional MPI. We suggest that incorporating MCE into routine triage tests for ACS may increase the diagnostic accuracy in these patients and lead to rapid and appropriate managements for ACS.
MCE is operator-dependent and has no standardized protocol. Moreover, multiple variables and artifacts affecting the optimal MCE analysis may reduce its diagnostic accuracy. Despite these technical pitfalls, MCE may be preferable to MPI in some clinical situations. MCE has a better spatial resolution and is feasible at any time without the aid of specialists, unlike MPI. Additionally, MCE can be performed at the bedside and interpreted without delay, enabling the rapid diagnosis of ACS at the time of presentation to the emergency department.
We qualitatively analyzed MCE data in this study. Although off-line quantitative assessment may provide more objective results, simultaneous interpretation during the acquisition of images is required for timely decision.
MPI could not be performed immediately after MCE on all patients due to a tight schedule of routine SPECT studies. Delays in obtaining MPI possibly underestimated the diagnostic accuracy of MPI. Since low feasibility and availability of MPI may restrict its utility at the emergency department, infrastructure would be needed to realistically use perfusion imaging in the routine clinical practice. In addition, the gating method was not used for about one-third of patients. Gated MPI allows simultaneous evaluation of perfusion and function, and has been shown to result in improved specificity by differentiating between defects and attenuation artifacts.21) However, we found that the diagnostic accuracy of MPI with and without gating was similar. Seven (11%) patients with true perfusion defects not associated with regional dysfunction were dichotomized as negative on gated MPI and two (6%) patients with attenuation artifacts were dichotomized as positive on MPI without gating.
This study was designed to test the diagnostic efficacy in high-risk chest pain patients and the incidence of ACS was higher than in other studies. The diagnostic accuracy of MCE and MPI may be changed in patients with intermediate or low risk chest pain. We excluded patients with previous myocardial infarction because perfusion imaging is unable to differentiate between ACS and previous myocardial infarction.
ACS was defined as the development of AMI or documentation of significant coronary artery stenosis that required urgent revascularization, a definition that has been used as a surrogate for unstable angina.12)13) Although it cannot be clearly defined, we included unstable angina in ACS, considering the prognostic implication of the early detection of unstable angina.
Finally, the small sample size of this study is also a limitation and further studies with enough power are needed to confirm our results.
Compared with routinely used troponin I, ECG criteria and even MPI, MCE is more accurate in diagnosing ACS. Early MCE is proposed to be a useful imaging technique in patients presenting to the emergency department with resting chest pain for whom early and accurate diagnosis remains difficult.
Figures and Tables
Fig. 1
Myocardial contrast echocardiography using power harmonic Doppler imaging with a dual-frame triggering (A). Left, perfusion frame was generated when the first packet of pulses encountered microbubbles in the myocardium and destroyed them. Right, post-destruction frame was obtained approximately 50 milliseconds later demonstrating the myocardium which was void of microbubbles. Apical perfusion defects are observed in the first perfusion imaging frame with 1 : 5 trigger rate. There was moderately decreased perfusion of the left anterior descending artery territory on myocardial perfusion imaging and critical stenosis of the left anterior descending artery on coronary angiography (B).
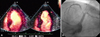
Fig. 2
Receiver-operating characteristics curve comparing the accuracy of myocardial contrast echocardiography (MCE) and myocardial perfusion imaging (MPI) for diagnosis of acute coronary syndrome (ACS). The area under the curve (AUC) of MCE was significantly larger than that of MPI (0.86 and 0.77, p=0.019).
Acknowledgements
We are indebted to Dr. Sung-Cheol Yoon at Ulsan University's Department of Biostatistics for helpful review of the statistical analysis in the paper.
References
1. Selker HP, Zalenski RJ, Antman EM, Aufderheide TP, Bernard SA, Bonow RO, Gibler WB, Hagen MD, Johnson P, Lau J, McNutt RA, Ornato J, Schwartz JS, Scott JD, Tunick PA, Weaver WD. An evaluation of technologies for identifying acute cardiac ischemia in the emergency department: a report from a National Heart Attack Alert Program Working Group. Ann Emerg Med. 1997. 29:13–87.

2. Pope JH, Ruthazer R, Beshansky JR, Griffith JL, Selker HP. Clinical Features of Emergency Department Patients Presenting with Symptoms Suggestive of Acute Cardiac Ischemia: A Multicenter Study. J Thromb Thrombolysis. 1998. 6:63–74.
3. Fineberg HV, Scadden D, Goldman L. Care of patients with a low probability of acute myocardial infarction. Cost-effectiveness of alternatives to coronary-care-unit admission. N Engl J Med. 1984. 310:1301–1307.

4. Beller GA. Beller GA, editor. Radiopharmaceuticals in nuclear cardiology. Clinical Nuclear Cardiology. 1995. Philadelphia, PA: Saunders;37–81.
5. Kontos MC, Jesse RL, Schmidt KL, Ornato JP, Tatum JL. Value of acute rest sestamibi perfusion imaging for evaluation of patients admitted to the emergency department with chest pain. J Am Coll Cardiol. 1997. 30:976–982.

6. Udelson JE, Beshansky JR, Ballin DS, Feldman JA, Griffith JL, Handler J, Heller GV, Hendel RC, Pope JH, Ruthazer R, Spiegler EJ, Woolard RH, Selker HP. Myocardial perfusion imaging for evaluation and triage of patients with suspected acute cardiac ischemia: a randomized controlled trial. JAMA. 2002. 288:2693–2700.

7. Jeetley P, Burden L, Greaves K, Senior R. Prognostic value of myocardial contrast echocardiography in patients presenting to hospital with acute chest pain and negative troponin. Am J Cardiol. 2007. 99:1369–1373.

8. Kaul S, Senior R, Dittrich H, Raval U, Khattar R, Lahiri A. Detection of coronary artery disease with myocardial contrast echocardiography: comparison with 99mTc-sestamibi single-photon emission computed tomography. Circulation. 1997. 96:785–792.

9. Jeetley P, Hickman M, Kamp O, Lang RM, Thomas JD, Vannan MA, Vanoverschelde JL, van der Wouw PA, Senior R. Myocardial contrast echocardiography for the detection of coronary artery stenosis: a prospective multicenter study in comparison with single-photon emission computed tomography. J Am Coll Cardiol. 2006. 47:141–145.

10. Senior R, Lepper W, Pasquet A, Chung G, Hoffman R, Vanoverschelde JL, Cerqueira M, Kaul S. Myocardial perfusion assessment in patients with medium probability of coronary artery disease and no prior myocardial infarction: comparison of myocardial contrast echocardiography with 99mTc single-photon emission computed tomography. Am Heart J. 2004. 147:1100–1105.

11. Lee CW, Moon DH, Hong MK, Lee JH, Choi SW, Yang HS, Kim JJ, Park SW, Park SJ. Effect of abciximab on myocardial salvage in patients with acute myocardial infarction undergoing primary angioplasty. Am J Cardiol. 2002. 90:1243–1246.

12. Kontos MC, Jesse RL, Anderson FP, Schmidt KL, Ornato JP, Tatum JL. Comparison of myocardial perfusion imaging and cardiac troponin I in patients admitted to the emergency department with chest pain. Circulation. 1999. 99:2073–2078.

13. Ohman EM, Armstrong PW, Christenson RH, Granger CB, Katus HA, Hamm CW, O'Hanesian MA, Wagner GS, Kleiman NS, Harrell FE Jr, Califf RM. GUSTO IIA Investigators. Cardiac troponin T levels for risk stratification in acute myocardial ischemia. N Engl J Med. 1996. 335:1333–1341.

14. Porter TR, Xie F. Visually discernible myocardial echocardiographic contrast after intravenous injection of sonicated dextrose albumin microbubbles containing high molecular weight, less soluble gases. J Am Coll Cardiol. 1995. 25:509–515.

15. Heinle SK, Noblin J, Goree-Best P, Mello A, Ravad G, Mull S, Mammen P, Grayburn PA. Assessment of myocardial perfusion by harmonic power Doppler imaging at rest and during adenosine stress: comparison with (99m)Tc-sestamibi SPECT imaging. Circulation. 2000. 102:55–60.

16. Kang DH, Kang SJ, Song JM, Choi KJ, Hong MK, Song JK, Park SW, Park SJ. Efficacy of myocardial contrast echocardiography in the diagnosis and risk stratification of acute coronary syndrome. Am J Cardiol. 2005. 96:1498–1502.

17. DeLong ER, DeLong DM, Clarke-Pearson DL. Comparing the areas under two or more correlated receiver operating characteristic curves: a nonparametric approach. Biometrics. 1988. 44:837–845.

18. Hilton TC, Thompson RC, Williams HJ, Saylors R, Fulmer H, Stowers SA. Technetium-99m sestamibi myocardial perfusion imaging in the emergency room evaluation of chest pain. J Am Coll Cardiol. 1994. 23:1016–1022.

19. Rinkevich D, Kaul S, Wang XQ, Tong KL, Belcik T, Kalvaitis S, Lepper W, Dent JM, Wei K. Regional left ventricular perfusion and function in patients presenting to the emergency department with chest pain and no ST-segment elevation. Eur Heart J. 2005. 26:1606–1611.

20. Kaul S, Senior R, Firschke C, Wang XQ, Lindner J, Villanueva FS, Firozan S, Kontos MC, Taylor A, Nixon IJ, Watson DD, Harrell FE. Incremental value of cardiac imaging in patients presenting to the emergency department with chest pain and without ST-segment elevation: a multicenter study. Am Heart J. 2004. 148:129–136.

21. DePuey EG, Rozanski A. Using gated technetium-99m-sestamibi SPECT to characterize fixed myocardial defects as infarct or artifact. J Nucl Med. 1995. 36:952–955.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download