Introduction
Myocardial abscess, a suppurative infection of the myocardium, endocardium, valves, perivalvular structures, or the cardiac conduction system, have been described very rarely.1) It is very rare and life-threatening disease, which occurs as a complication of infectious diseases or acute myocardial infarction in the setting of debilitating condition. However, there was no report of myocardial abscess mimicking acute myocardial infarction.
Case
A 46-year-old woman, who had suffered from left anterior chest pain lasting 2 days, visited our hospital. She had been treated with chemotherapy for 3 years due to myelodysplastic syndrome (MDS). She did not ever smoke and does not have diabetes or hypertension. Her blood pressure on admission was 120/80 mmHg and body temperature was 36.5℃.
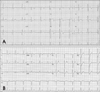
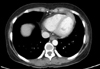
Her electrocardiogram (ECG) on admission showed ST segment elevations and T wave inversions in the anterior leads (Fig. 1A). In initial laboratory examination, leukocytopenia and thrombocytopenia were detected (WBC count= 1,300/mm3, platelet count=5,000/mm3). Initial cardiac markers were normal (Troponin I=0.001 ng/mL, CK-MB= 5.1 U/L, AST=14 U/L) and C-reactive protein was elevated up to 21.5 mg/dL (reference level=0-0.3 mg/dL). Transthoracic echocardiogram (TTE) (Fig. 2) was performed with suspicion of acute coronary syndrome revealed hypokinesia in apical septal and apical anterior wall of left ventricle (LV). We found the hypoechoic lesion at the myocardium just adjacent hypokinetic lesion. The size of lesion was 27.2×11.9 mm in the 2D echocardiogram. Cardiac computed tomography (Cardiac CT) (Fig. 3) demonstrated mild diffuse thickening with contrast enhancement of pericardium and loculated fluid collection in anterior myocardium and pericardium without definite luminal narrowing in coronary arteries.
Because her platelet count was extremely low and size of the lesion was too small, we managed her conservatively with antibiotics (third generation cephalosporin plus aminoglycoside) instead of invasive management. TTE which checked 2 weeks later after the first exam (Fig. 4A and B) showed no significant interval changes. Follow-up chest CT (Fig. 5) which was checked 3 weeks later since antibiotics treatment revealed markedly decreased lesion, but still remained focal wall thickening and enhancement. Furthermore, Follow-up 2D echocardiogram done in 7 weeks later (Fig. 4C and D) demonstrated complete resolution of the lesion and the regional wall motion abnormality. Furthermore, follow-up ECG (Fig. 1B) showed normalization of ST-segment abnormality.
Discussion
Myocardial abscess, a suppurative infection of the myocardium, endocardium, valves, perivalvular structures, or the cardiac conduction system, have been described very rarely.1) Generally, this disease occurs as a complication of infective endocarditis, acute myocardial infarction (AMI), or other infections in the setting of debilitating condition.1-7) In our case, interestingly, there was no definite infection focus or coronary obstruction in cardiac CT. To the best of our knowledge, this is the first case of myocardial abscess presented as AMI, not a following consequence of AMI.
In the past, most cases of myocardial abscess were found during autopsy. Nowadays, however, we can detect the disease during the antemortem period with the development of various diagnostic modalities, such as, TTE, transesophageal echocardiography (TEE), cardiac CT and cardiac magnetic resonance imaging. Despite of such a development of diagnostic tools, the diagnosis of myocardial abscess is challenging. The reason is that it is needed the highly suspicion of the disease, that the disease is very rare, and that diagnostic measures have a low sensitivity yet. TTE has a sensitivity of 23% and a specificity of 98.6% in diagnosing,8) and TEE a sensitivity of 48% sensitivity.9) In the present case, the patient had a typical chest pain and ECG abnormalities suggesting AMI and simultaneously being a obstacle to give a accurate diagnosis. We found a pericardial abscess using TTE and Cardac CT, in which pericardial abscess located along the path of left anterior descending coronary artery. This anatomical location of the abscess might make it possible that presentation of the symptom and sign mimicked acute anterior wall ST-segment elevation myocardial infarction.
Patients with myocardial abscess can be saved by intensive medical treatment including antibiotics and by prompt surgical intervention.10) Generally, urgent surgical intervention is needed in most cases of myocardial abscess. The delay to surgical intervention raises the perioperative risk and the risk of rupture. In spite of medical therapy only, fortunately, our patient overcame the disease. Indeed, 40% of cases involve more than one microbial etiology in myocardial abscess and gram negative infection is often related to debilitating condition. That is why we used third generation cephalosporin plus aminoglycoside. This lucky result might due to relatively small size of the lesion and the absence of definite serious other infection, such as infective endocarditis or sepsis.
Electrocardiographic findings in the myocardial abscess are not specific. Some cases showed fatal arrhythmia such as ventricular arrhythmia or complete heart block and some revealed conduction delay such as PR prolongation.11-14) Nevertheless, almost of them showed non-specific findings in ECG. Our cases showed ST segment elevations and T wave inversion in anterior leads without definite coronary obstruction.
In conclusion, myocardial abscess, a rare but fatal disease, can present as AMI. To give a prompt diagnosis, it is needed the highly suspicion of the disease, especially in the patient presented as AMI without risk factors of coronary artery disease in the setting of debilitating condition such as MDS. Although its accuracy is low, 2D-echocardiography may be helpful to make a diagnosis with the aid of cardiac CT.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download