Abstract
Precutaneous transcatheter device closure of interatrial communications is used as an alternative to surgery or long-term anticoagulation for the treatment of patients with paradoxical cerebral embolism. We report a case of successful percutaneous transcatheter closure of small atrial septal defect in a 34 year old female patient with acute cerebral infarction presumably caused by paradoxical embolism through the defect.
The cause of ischemic stroke so called, cryptogenic strokes is uncertain in approximately 40% of cases despite of intensive evaluation.1) Passage of thromboemboli from the right side circulation to the left side circulation through interatrial communications such as patent foramen ovale (PFO) or atrial septal defect (ASD) has been postulated as a possible mechanism of these cryptogenic strokes.2-5) Furthermore, percutaneous device closure of the interatrial communications has been proved to be a safe and effective method for the secondary prevention of presumed paradoxical embolism.6-10)
We report a case of successful percutaneous closure of small ASD in patient with acute cerebral infarction presumably caused by paradoxical embolism through the defect.
A 34-year-old female who was in the eighth week of gestational age was presented with a sudden onset of stuporous mental status and quadriplegia. The patient had been apparently healthy without any known medical illness before admission. Imaging studies including brain computed tomography (CT), CT angiography (CTA), and magnetic resonance image (MRI) revealed multifocal cerebral and cerebellar infarction associated with thrombotic occlusion in the distal basilar artery, P1 portion of both posterior cerebral arteries, and the origin site of both superior cerebellar arteries (Fig. 1). Conventional 4 vessel angiography also revealed thrombotic total occlusion of the distal basilar artery without distal flow (Fig. 2A and B). Intra-arterial thrombolytic therapy using urokinase was done after the successful positioning of the arterial catheter within the basilar artery. After the successful thrombolytic therapy, thrombus in the basilar artery was resolved and distal flow was improved (Fig. 2C and D). Mental status and neurologic deficits of the patient were nearly normalized within 2 weeks of hospitalization and therapeutic abortion was done.
Laboratory tests for the evaluation of hypercoagulability showed no abnormal findings. Imaging studies including transthoracic echocardiography (TTE), transesophageal echocardiography (TEE), carotid ultrasound, and venous CTA of the extremities for the evaluation of thromboembolic source also showed no abnormal findings except for hemodynamically insignificant small ASD of secundum type (Fig. 3). Paradoxical cerebral embolism through the ASD could have been a possible mechanism of cryptogenic stroke in this patient. Therefore, percutaneous device closure of the ASD was planned for the secondary prevention of recurrent cerebral infarction.
Percutaneous transcatheter closure of ASD was performed under general anesthesia. Under the guidance of fluoroscopy and TEE, the diameter of the ASD was 0.65 cm and balloon stretched diameter of the ASD measured by TEE using the sizing balloon was 0.9 cm. The delivery catheter containing 1.0 cm sized Amplatzer septal occluder (ASO) was passed over the guidewire and introduced into the left atrium. The left atrial disk and waist were opened and positioned against the interatrial septum before the deployment of the right atrial disk. To exclude the presence of any device instability, careful pull and push movement tests were performed before releasing the device. After adequate stability was achieved, the ASO device was released. After the successful deployment of the ASO device, TEE showed good positioning of the device with minimal residual shunt flow through the device (Fig. 3B). On the next day, a follow-up TTE revealed stable positioning of the device without residual shunt flow (Fig. 4). The patient was discharged and had no events during 6-months of clinical follow-up.
We report here an unusual case of acute cryptogenic cerebral infarction in young female patient with small ASD. Although the diameter of the ASD was 0.6 cm and the ratio of pulmonary (Qp) to systemic blood flow (Qs) was 1.35, the ASD of this patient was treated by percutaneous device closure. ASD itself in this patient was not significant hemodynamically and thus it was not an indication for surgery or percutaneous device closure. Despite intensive evaluation, however, the cause of acute cerebral infarction was not identified and thus paradoxical embolism through the ASD was a possible explanation for the cause of cerebral infarction in this young female patient. Although it was the first attack, the size of cerebral infarction was very large and it was expected that the recurrence of cerebral infarction might be critical in this patient. Therefore, we planned to perform precutaneous device closure of the ASD for the prevention of recurrent cerebral infarction.
Paradoxical embolism involves the passage of the venous thromboembolic material into the arterial system through a right to left intracardiac shunt.2-5) Despite wide intensive evaluation, the cause of ischemic stroke remains uncertain in approximately 40% of cases and is presumably associated with this paradoxical embolic phenomenon. The clinical presentations of paradoxical embolism are various and include cerebral infarction, peripheral vascular thrombotic occlusion, renal infarction, myocardial infarction, and so on. The importance of PFO with and without atrial septal aneurysm and ASD as a mechanism for paradoxical embolism in still controversial, but continues to gain acceptance.
Paradoxical embolism in the setting of atrial shunts is traditionally treated by long-term antiplatelet agents, warfarin, or direct closure of the defect in the atrial septum.11)12) Recently, several effective devices were introduced and used for percutaneous transcatheter closure of PFO or ASD as an alternative for surgical treatment. Previous studies including the study of Windecker et al have been demonstrated that percutaneous device closure of the PFO or ASD is as an effective technique for the prevention of recurrent systemic thromboembolism in patients with cryptogenic stroke like this patient.6-10)
In conclusion, percutaneous transcatheter closure of interatrial communication might be a promising therapeutic strategy and should be considered especially in patients with paradoxical embolism who are presented with severe life threatening manifestation in its first attack.
Figures and Tables
Fig. 1
Computed tomographic angiography of the brain revealed thrombotic occlusion in the distal basilar artery, P1 portion of both cerebral arteries, and the origin site of both superior cerebellar arteries (A). Magnetic resonance image of the brain revealed multifocal cerebral and cerebellar infarction (B).
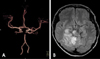
Fig. 2
Conventional 4 vessel angiography also revealed thrombotic occlusion in the distal basilar artery, P1 portion of both cerebral arteries, and the origin site of both superior cerebellar arteries without distal flow (A, B). Follow up angiography just after the administration of intra-arterial urokinase revealed resolution of the thrombus with the restoration of distal flow.

References
2. Gazzaniga AB, Dalen JE. Paradoxical embolism: Its pathophysiology and clinical recognition. Ann Surg. 1970. 171:137–142.
3. Wu LA, Malouf JF, Dearani JA, Hagler DJ, Reeder GS, Petty GW, Khandheria BK. Patent foramen ovale in cryptogenic stroke. Arch Intern Med. 2004. 164:950–956.

4. Muller L, Dillon T, Beekman RH. Myocardial ischemia: Atypical presentation of an atrial septal defect in childhood. J Interv Cardiol. 2005. 18:397–399.

5. Bartz PJ, Cetta F, Cabalka AK, Reeder GS, Squarcia U, Agnetti A, Aurier E, Carano N, Tachana B, Hagler DJ. Paradoxical emboli in children and young adults: Role of atrial septal defect and patent foramen ovale device closure. Mayo Clin Proc. 2006. 81:615–618.

6. Windecker S, Wahl A, Chatterjee T, Garachemani A, Eberli FR, Seiler C, Meier B. Percutaneous closure of patent foramen ovale in patients with paradoxical embolism: Long-term risk of recurrent thromboembolic events. Circulation. 2000. 101:893–898.

7. Hung J, Landzberg MJ, Jenkins KJ, King MEE, Lock JE, Palacios IF, Lang P. Closure of patent foramen ovale for paradoxical emboli: Intermediate-term risk of recurrent neurological events following transcatheter device placement. J Am Coll Cardiol. 2000. 35:1311–1316.

8. Bruch L, Parsi A, Grad MO, Rux S, Burmeister T, Krebs H, Kleber FX. Transcatheter closure of interatrial communications for secondary prevention of paradoxical embolism: Single-center experience. Circulation. 2002. 105:2845–2848.

9. Khairy P, O'Donnell CP, Landzberg MD. Transcatheter closure versus medical therapy of patent foramen ovale and presumed paradoxical thromemboli: A systematic review. Ann Intern Med. 2003. 139:753–760.

10. Harms V, Reisman M, Fuller CJ, Spencer MP, Oslen JV, Krabill KA, Gray WA, Jesurum JT. Outcomes after transcatheter closure of patent foramen ovale in patients with paradoxical embolism. Am J Cardiol. 2007. 99:1312–1315.





 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download