Abstract
Background and Objectives
Marfan syndrome (MFS) is a connective tissue disorder with autosomal dominant inheritance and a highly variable clinical spectrum. However, there are limited data available on the clinical features of Korean patients with MFS. The aim of the present study was to describe the clinical characteristics and outcomes of Korean patients with MFS.
Subjects and Methods
We included all patients who were diagnosed with MFS between January 1995 and May 2015 at a single tertiary medical center. Patients with an MFS-related disorder including MASS phenotype (myopia, mitral valve prolapse, borderline and non-progressive aortic root dilatation, skeletal findings, and striae), mitral valve prolapse syndrome, and ectopia lentis syndrome were excluded. A total of 343 Korean patients aged ≥15 years who satisfied the revised Ghent nosology were included.
Results
The mean patient age at diagnosis was 35.9±12.6 years and 172 (50.1%) patients were male. Median follow-up duration was 52.8 months. A total of 303 patients (88.6%) had aortic root dilatation with Z score ≥2 or aortic root dissection. Ectopia lentis was relatively less common (163 patients, 55.1%) and systemic score ≥7 was found in 217 patients (73.8%). Among 219 probands, a family history of MFS was present in 97 patients (44.5%) and sporadic cases in 121 patients (55.5%). Among the 157 probands who underwent genetic analysis, 141 (89.8%) had an FBN1 mutation associated with aortic root aneurysm/dissection. Aortic dissection (AD) or intramural hematoma (IMH) was identified in 110 patients (32.1%). Among the 221 patients without AD or IMH, descending aortic aneurysms were identified in 19 patients (8.6%). Two hundred thirteen patients (62%) underwent cardiovascular surgery of any type. Eight patients died during follow-up.
Conclusion
We described the clinical characteristics and outcomes of Korean MFS patients. Cardiovascular manifestations were commonly detected and FBN1 mutation was present in approximately 90% of patients. In contrast, ectopia lentis was identified in approximately half of patients. Our findings will be informative for the evaluation of patients with MFS.
Marfan syndrome (MFS) is a connective tissue disorder with autosomal dominant inheritance that is caused by mutation in the fibrillin-1 (FBN1) gene.1)2) The clinical spectrum of MFS is highly variable, even within an affected family, and shows multiorgan involvement affecting the skeleton, the cardiovascular system, the eyes, the lungs, and the skin. Cardiovascular involvement is the most common cause of morbidity and mortality in MFS.3)
The diagnosis of MFS has depended on the revised Ghent nosology, which is based on data obtained from predominantly Western populations.4) Possible ethnic differences in the clinical manifestations of patients with MFS have been suggested.5) However, there are limited data available on the clinical features of Korean patients with MFS, and the available reports are based on only small numbers of patients.5)6) Therefore, the aim of the present study was to describe the clinical characteristics and outcomes of Korean patients with MFS.
We identified all patients who were diagnosed with MFS between January 1995 and May 2015 in the Marfan Clinic at a single tertiary medical center. We screened 409 patients. Patients who were diagnosed with MFS-related disorders including MASS phenotype (myopia, mitral valve prolapse, borderline and non-progressive aortic root dilatation, skeletal findings, and striae), mitral valve prolapse syndrome (MVPS), and ectopia lentis syndrome (ELS) were excluded. Among patients with possible MFS, those who did not satisfy the revised Ghent nosology because of insufficient evaluation for MFS were also excluded.4) In addition, patients aged <20 years who had insufficient systemic features and borderline aortic root dilatation indicating potential MFS were excluded. Finally, a total of 343 Korean patients aged ≥15 years who satisfied the revised Ghent nosology were included.
The multidisciplinary data including physical examination, computed tomography (CT) angiography, transthoracic echocardiography, slitlamp examination, and genetic analysis were collected retrospectively from the medical records. We measured the aortic diameter at the level of the sinus of Valsalva on at least two images from transthoracic echocardiography.7) If transthoracic echocardiographic imaging before aortic surgery or aortic dissection was not available, we measured the diameter at the level of the sinus of Valsalva on CT angiography.8) The Z-score was calculated on the basis of aortic diameter with age and body surface area (BSA).9) The descending aorta was considered to be an aneurysm if any diameter of the aorta was greater than 35 mm without aortic dissection.8) Ectopia lentis was diagnosed by an ophthalmologist using slit lamp examination. In addition, patients were regarded as having ectopia lentis if they had a history of previous eye surgery for lens dislocation. Myopia was defined as a spherical equivalent less than -3.0 diopters. An FBN1 gene mutation was defined as positivity for the mutation known to be associated with aortic root aneurysm/dissection.4) Extended physical examination was performed by medical specialists. Protrusio acetabuli was defined as medial displacement of the acetabulum on axial CT images.7)10) We obtained death registry data from the National Statistical Office of South Korea.
Continuous variables are presented as mean±one standard deviation, and categorical variables as numbers and percentages. Data analysis was performed using SPSS version 21 (IBM, Armonk, NY, USA). This study was approved by the institutional review board of Samsung Medical Center.
A total of 343 patients with MFS and 218 probands were identified. Median follow-up duration was 52.8 months (range 0.0 to 233.9 months). The mean patient age at diagnosis was 35.9±12.6 years and 172 patients (50.1%) were male. Mean height was 184.4±10.0 cm for male patients and 170.5±7.7 cm for females. Beta-blockers were used in 96.8% of patients with MFS and angiotensin-converting enzyme (ACE) inhibitors or angiotensin receptor blockers (ARBs) were used in 68.8% of them during the last 3 years of follow-up. The clinical characteristics of the patients with MFS are described in Table 1.
In the systemic features, facial features (231 patients, 75.2%), wrist and thumb sign (216 patients, 71.1%), myopia (162 patients, 70.4%), skin striae (69.8%), protrusio acetabuli (205 patients, 64.3%), and dural ectasia (196 patients, 61.8%) were common. In contrast, skeletal manifestations including pectus carinatum deformity (27 patients, 8.2%), pectus excavatum or chest asymmetry (50 patients, 15.2%), increased arm/height (45 patients, 15.0%), and reduced elbow extension (55 patients, 17.5%) were rarely detected.
The components of revised Ghent nosology in patients with MFS are shown in Table 2. A total of 303 patients (88.6%) had aortic root dilatation with Z score ≥2 or aortic root dissection. Ectopia lentis was relatively less common (163 patients, 55.1%) and systemic score ≥7 was found in 217 patients (73.8%). Among 218 probands, 121 patients (55.5%) were identified as sporadic cases and 97 patients (44.5%) had a family history. Among the 157 probands who underwent genetic analysis, 141 (89.8%) patients had an FBN1 mutation associated with aortic root aneurysm/dissection.
Clinical outcomes of Korean patients with MFS are shown in Table 3. Of a total of 343 patients, aortic dissection (AD) or intramural hematoma (IMH) was identified in 110 patients (32.1%). Among the 110 patients with AD or IMH, AD was detected in 106 patients (96.3%), including 2 patients with a mixed type of AD and IMH, and IMH was present in only 4 patients (3.6%). Of the 106 patients with AD, 70 (66.0%) had type A AD and 36 (34.0%) had Type B AD. Data on aortic diameter of sinus of Valsalva at the time of AD was available in 40 patients and was 6.29±1.19 cm (range 3.4 to 9.3 cm) in patients with Type A AD. Two patients experienced Type A AD with aortic diameter at the level of sinus of Valsalva less than 4.5 cm. Among the 36 patients with type B AD, maximal diameter of the descending aorta at the time of diagnosis with type B AD was 4.51±1.66 cm (range 2.64 to 8.4 cm) in 31 patients for whom data were available.
Among the 221 patients who did not have AD or IMH, descending aortic aneurysm was identified in 19 patients (8.6%); thoracic aortic aneurysm in 3 patients (15.8%), thoracoabdominal aortic aneurysm in 6 patients (31.6%), and abdominal aortic aneurysm in 10 patients (52.6%). Of a total of 343 patients, 213 patients underwent cardiovascular surgery of any type. Patients' age at the time of initial cardiovascular surgery was 35.5±11.3 years (range 6.3-69.6 years). Eight patients died during follow-up.
In the present study we documented the clinical characteristics of a large number of Korean patients with MFS. The majority of Korean MFS patients had cardiovascular manifestations, especially ascending aorta dilatation/dissection, and an FBN1 mutation. Systemic score ≥7 was identified in approximately two-thirds of all patients. In contrast, ectopia lentis and a family history of MFS were relatively uncommon findings that were documented in about half of our MFS patients.
The mortality rate in patients with MFS is 20-40 times higher than in normal individuals of the same age.11) The clinical manifestations of patients with MFS are highly variable. As more than two-thirds of our Korean patients with MFS showed characteristic wrist and/or thumb sign, facial features, and skin striae, we suggest that careful physical examination is extremely important for the diagnosis of MFS. In addition, we identified that dural ectasia and protrusio acetabuli were also common findings. In the process of evaluation of aortic dissection, inspective review of CT angiography could be critical in diagnosing MFS, especially for young patients without risk factors such as hypertension, because sufficient data for the diagnosis of MFS might be obtained by CT angiography.12)
Among patients with MFS, possible ethnic differences in clinical manifestations between Asian and Western populations were reported.13) Akutsu et al.13) showed that Japanese patients with MFS had less common skeletal involvement as compared with Western patients. This is consistent with our findings in Korean patients with MFS. We identified increased arm/height in 15% and scoliosis in 19% of our patients, compared with 55% and 53% of Western patients with MFS, respectively.14) In addition, Korean patients with MFS had shorter height, lower body weight, and lower body surface area in comparison with Western patients.15)
We identified more common cardiovascular involvement that included aortic root dilatation of Z score ≥2 or aortic root dissection in 88%, any aortic dissection or IMH in 32%, and Type A AD in 20% of our Korean patients with MFS, compared with corresponding values of 77%, 21% and 14% among Western patients, respectively.14) In addition, more than 60% of our patients had some form of cardiovascular surgery, even though their mean age was only 35.9 years. The most common cause of death in MFS is a cardiovascular manifestation such as aortic dissection, congestive heart failure, or valvular heart disease.2) Cardiovascular involvement might manifest more commonly in Asian patients than in Western patients.13)14)15) Therefore, we suggest that more careful evaluation and follow-up for cardiovascular involvement might be needed in Korean patients with MFS.
With respect to ocular manifestations, ectopia lentis was present in 54.6% of Korean patients in the present study. In earlier studies, Asian patients with MFS had a lower occurrence of ectopia lentis (25-36%) as compared with Western patients (54%).5)13)14)15) However, the results of previous studies might have shown selection bias because of the small numbers of patients involved. We identified that Korean patients with MFS had a comparable incidence of ocular manifestation including ectopia lentis and myopia, although ocular manifestation was relatively less frequent than other organ involvement. Nonetheless, considering the cardiovascular and skeletal manifestations, ethnic differences of clinical features in MFS patients are possible.
If patients have a family history of MFS, diagnosis can be made with comparative ease based on the revised Ghent nosology when the patients have any manifestations among ectopia lentis, systemic score ≥7, and aortic dilatation with Z score ≥2 or aortic root dissection. In contrast, for patients without family history of MFS, the diagnosis of MFS should depend on an aortic dilatation with Z score ≥2 or aortic root dissection, except for patients with concurrent ectopia lentis and an FBN1 mutation of known association with aortic root aneurysm/dissection. Therefore, the diagnosis of MFS might be delayed until significant aortic root dilatation with Z score ≥2 or aortic dissection has developed. In Korea, the diagnosis of genetic disorders is particularly difficult because patients tended to be reluctant to undergo genetic screening, although this situation has recently improved. Moreover, probands with a family history were only 45.5% of cases in this study. A cohort of Korean patients with MFS might consist mainly of patients diagnosed by cardiovascular events such as aortic dissection rather than asymptomatic patients diagnosed by family screening. In this regard, the rate of cardiovascular manifestations in Korean patients with MFS might be overestimated. Therefore, early detection of asymptomatic patients in Korea through active genetic screening of MFS-affected families would be critical.
The present study has several limitations. Because of its retrospective design, data collection based on medical records was limited. In addition, this study might have a selection bias. Because our center was a tertiary referral center, we could not obtain sufficient data for long-term clinical outcomes. Nevertheless, we described the clinical characteristics and outcomes during a median follow-up duration of 52.8 months.
In conclusion, we described the clinical characteristics and outcomes of Korean patients with MFS. Cardiovascular manifestations were commonly detected and an FBN1 gene mutation was present in approximately 90% of patients. In contrast, ectopia lentis was identified in approximately half of our patients. To the best of our knowledge, the current study reports on clinical characteristics based on the largest numbers of Korean MFS patients studied to date. Our findings will be informative for the evaluation of patients with MFS.
Figures and Tables
Table 1
Clinical characteristics of patients with MFS

Table 2
Components of the revised Ghent nosology in patients with MFS
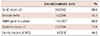
| Events/available data | % | |
|---|---|---|
| Ao (Z score ≥2) | 303/342 | 88.6 |
| Ectopia lentis | 163/296 | 55.1 |
| FBN1 gene mutation | 141/157* | 89.8 |
| Systemic score ≥7 | 217/294 | 73.8 |
| Family history of MFS | 97/218 | 44.5 |
Table 3
Clinical outcomes of patients with MFS

References
1. Pyeritz RE. Marfan syndrome. N Engl J Med. 1990; 323:987–989.
2. Judge DP, Dietz HC. Marfan's syndrome. Lancet. 2005; 366:1965–1976.
3. von Kodolitsch Y, De Backer J, Schüler H, et al. Perspectives on the revised Ghent criteria for the diagnosis of Marfan syndrome. Appl Clin Genet. 2015; 8:137–155.
4. Loeys BL, Dietz HC, Braverman AC, et al. The revised Ghent nosology for the Marfan syndrome. J Med Genet. 2010; 47:476–485.
5. Yoo EH, Woo H, Ki CS, et al. Clinical and genetic analysis of Korean patients with Marfan syndrome: possible ethnic differences in clinical manifestation. Clin Genet. 2010; 77:177–182.
6. Yang JH, Han H, Jang SY, et al. A comparison of the Ghent and revised Ghent nosologies for the diagnosis of Marfan syndrome in an adult Korean population. Am J Med Genet A. 2012; 158A:989–995.
7. Lang RM, Badano LP, Mor-Avi V, et al. Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J Am Soc Echocardiogr. 2015; 28:1–39.e14.
8. Kim EK, Choi SH, Sung K, et al. Aortic diameter predicts acute type A aortic dissection in patients with Marfan syndrome but not in patients without Marfan syndrome. J Thorac Cardiovasc Surg. 2014; 147:1505–1510.
9. Devereux RB, de Simone G, Arnett DK, et al. Normal limits in relation to age, body size and gender of two-dimensional echocardiographic aortic root dimensions in persons ≥15 years of age. Am J Cardiol. 2012; 110:1189–1194.
10. Lin FY, Devereux RB, Roman MJ, et al. Assessment of the thoracic aorta by multidetector computed tomography: age- and sex-specific reference values in adults without evident cardiovascular disease. J Cardiovasc Comput Tomogr. 2008; 2:298–308.
11. Williams A, Davies S, Stuart AG, Wilson DG, Fraser AG. Medical treatment of Marfan syndrome: a time for change. Heart. 2008; 94:414–421.
12. Sohn GH, Jang SY, Moon JR, et al. The usefulness of multidetector computed tomographic angiography for the diagnosis of Marfan syndrome by Ghent criteria. Int J Cardiovasc Imaging. 2011; 27:679–688.
13. Akutsu K, Morisaki H, Takeshita S, et al. Characteristics in phenotypic manifestations of genetically proved Marfan syndrome in a Japanese population. Am J Cardiol. 2009; 103:1146–1148.
14. Faivre L, Collod-Beroud G, Loeys BL, et al. Effect of mutation type and location on clinical outcome in 1,013 probands with Marfan syndrome or related phenotypes and FBN1 mutations: an international study. Am J Hum Genet. 2007; 81:454–466.
15. Franken R, den Hartog AW, van de Riet L, et al. Clinical features differ substantially between Caucasian and Asian populations of Marfan syndrome. Circ J. 2013; 77:2793–2798.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download