Abstract
An immunoglobulin G4 (IgG4)-related disease is a recently emerging entity, and a few cases of IgG4-related disease in lung and pleura have been reported. Herein, we report the case of a 74-year-old man with IgG4-related disease of lung and pleura, clinically suspicious of malignant mesothelioma. Chest computed tomography showed diffuse nodular pleural thickening, and microscopic finding disclosed diffuse thickening of visceral pleura with infiltrations of many lymphoplasma cells with increased number of IgG4-positive plasma cells and a few multinucleated giant cells. It is important for pathologists and clinicians to recognize this rare entity and its histologic finding, because it can be confused with malignant tumors on the radiologic examination although it can be treated with steroid therapy.
Immunoglobulin G4 (IgG4)-related disease is a recent outstanding disease entity that is characterized by elevated level of serum IgG4 and microscopic infiltration of many IgG4-positive plasma cells1. Although IgG4-related lesion was originally introduced as sclerosing pancreatitis, it had been known to involve a variety of organs including salivary glands, gallbladder, kidney, thyroid, lymph node and lung2. Regardless of involved organs, it shares similar clinicopathological features, such as old age, predominance in male, involvement of multiorgan, elevated serum level of IgG4 and excellent response to steroid therapy3. Although a few cases of IgG4-related disease in the lung and pleura (IgG4-LP) have been reported1,4-7, it is important that it can be easily confused to inflammatory conditions or primary/metastatic malignancy showing diffuse pleural thickening and pulmonary nodules. Herein, we report the case of a 74-year-old man with IgG4-LP, clinically mimicking malignant mesothelioma.
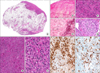
A 74-year-old male patient had been followed-up for 4 years after radical prostatectomy due to adenocarcinoma of prostate. He was experienced smoker with 30 pack-years and had history of medication for diabetes mellitus and hypertension, but no history of drug, allergy or autoimmune disease and occupational or environmental exposure to asbestos. On the follow-up examinations, the right pleural effusion on chest X-ray (Figure 1A, one year ago) and the patchy lesions of the right lung on computed tomography (Figure 1C, 6 months ago) were found. However, serum prostate-specific antigen level was within normal limit, and repeated cytological evaluations for pleural effusion showed no evidence of malignancy. Multiple nodules and diffuse pleural thickening in the left lower lung field were newly developed 3 months ago (Figure 1D). Positron emission tomography also disclosed hot uptake on these new nodules (Figure 1B, arrows) and no identifiable lesions on the other organs including pancreas, thyroid and salivary gland. Under the impression of mesothelioma, wedge resection was done. Microscopically, visceral pleura and alveolar interstitium were thickened with dense cellular infiltration and fibrosis (Figure 2A). Infiltrates were mainly composed of lymphoplasma cells without cytological atypia (Figure 2F, G). Many multinucleated giant cells of foreign-body type were noted near the degenerated elastic layer of the visceral pleura on the inflammatory and fibrotic background (Figure 2B-D). Some blood vessels showed angiocentric infiltration of lymphoplasma cells, but there was no evidence of destructive changes such as neutrophilic infiltration and fibrinoid necrosis in the vessel walls (Figure 2E). All special stains for acid fast bacilli, Grocott-Gomori methenamine silver, periodic acid-Schiff, and mucicarmine failed to demonstrate any organism. The results of immunohistochemical stain with IgG (1:1,000, Dako, Glostrup, Denmark) and IgG4 (1:2,000, Binding Site, Bermingham, UK) revealed increased proportion of IgG4-positive plasma cells, estimated at about 40% (Figure 2H, I). Based on the histological and immunohistochemical findings, IgG4-related disease was confirmed, and increased serum level of IgG4 (over than 201 mg/dL) were subsequently checked. The patient showed excellent response to treatment with steroid (prednisolone) and followed-up over 20 months without any evidence of recurrence.
IgG4 related disease is rare disease, especially in the case with an involvement of the lung. Three cases of IgG4-LP have been reported in Korea, since the first two cases reported in 20096,7. However, these cases were somewhat different from present case that the formers developed mainly as pulmonary nodules and our case presented as pleural nodule.
The involvements of lung and pleura in IgG4-related disease have a variety of radiological and histological features. Common microscopic findings of these lesions can be characterized as obliterative vasculitis with dense fibrosis and marked infiltration of IgG4-positive plasma cells5. According to the review by Zen et al.1, IgG4-LP can be radiologically categorized into pulmonary lesions (patterns of nodular, bronchovascular, interstitial, and round shaped ground glass opacity) and pleural lesion, and also histologically into solid nodular, bronchovascular and alveolar interstitial type. On clinical and radiologic evaluations, IgG4-LP also can be masqued as interstitial or bronchopneumonia as well as malignancies of lung or pleura1. Therefore, it is necessary to have histological confirmation and to recognize each microscopic subclasses for the exclusions of neoplasms or the other inflammatory disorders, because it can be critical point for treatment plan.
Clinicoradiological differential diagnoses include some malignant diseases, such as malignant mesothelioma, pseudomesotheliomatous adenocarcinoma and epithelioid hemangioendothelioma with pleural involvement. Malignant mesothelioma has a typical radiologic pattern showing diffuse infiltrative pleural thickening and frequent pleural effusion. However, it is histologically different from IgG4-LP, that the former shows infiltrative atypical tumor cells forming papillae, pseudoacini or solid nests, and the tumor cells are positive for mesothelial markers (Calretinin or HBME-1)8. A small part of pulmonary adenocarcinoma, called as pseudomesotheliomatous adenocarcinoma, can be developed with mesotheliomatous radiologic pattern. Most cases of this disease were usually detected in the advanced states with the involvements of multi-lobes or multiple nodal metastasis8. Histologically, pseudomesotheliomatous adenocarcinoma displays glandular structures with tumor cells that are immunoreactive for typical adenocarcinoma marker (thyroid transcription factor-1)8. Although thoracic epithelioid hemangioendothelioma can rarely involve the pleura with diffuse infiltrative thickening, the tumor mass consists of epithelioid cells with abundant cytoplasm and intracytoplasmic vacuolization and positive for vascular endothelial markers (CD31, CD34, and factor VIII)9.
Histopathologically, IgG4-LP should be discriminated from other inflammatory or neoplastic conditions. Because IgG4-LP might show obliterative phlebitis and arteritis, disease of vasculitis should be considered as differential diagnosis. Although primary vasculitis typically shows destruction of the vessel walls with fibrinoid necrosis, neutrophilic infiltration and granuloma formation, these are uncommon findings in the IgG4-LP. Vascular involvement of infectious disease can also display an inflammatory infiltrates in the vessel walls5. Therefore, vascular destruction or sources of infection should be examined by other special stains.
Recently, it has been suggested that some portion of lesions known as inflammatory pseudotumor (IPT) may be IgG4-related sclerosing disease10. Both IgG4-LP and inflammatory myofibroblastic tumor (IMT, previously included within IPT category) can share similar tumorous microscopic finding, comprising of infiltrate of lymphocytes and plasma cells with bland-looking spindle cell proliferation and fibrosis. However, IMT shows rare obstructive phlebitis, inflammatory infiltration with lower ratio of IgG4/IgG-positive plasma cells and no increased serum level of IgG4 on the contrary to IgG4-related disease11.
Lymphomatoid granulomatosis (LYG) can be one of the another differential diagnosis, because of its morphologic similarity4,5. LYG is one of B lineage lymphoproliferative disorder that is associated with Epstein-Barr virus (EBV) and can show obliterative vasculitis and interstitial inflammation4. It is occasionally difficult to distinguish between LYG and IgG4-LP, because grade 1 of LYG (LYG-G1) is frequently devoid of cellular atypia, necrosis and EBV infected cells5. Evaluation for the ratio of IgG4/IgG-positive plasma cells might be a critical diagnostic tool between IgG4-LP and LYG-G11,3. According to the recently proposed histologic criteria, increased ratio of IgG4/IgG-positive plasma cells (more than 40%) is diagnostic for IgG4 related sclerosing disorders2. The ratio of IgG4/IgG-positive plasma cells of our case was about 40%, compatible with IgG4-LP.
Interestingly, our case had a distinct histologic feature that multinucleated giant cells were noted around the peripheral lung field. We thought the possibility that these multinucleated giant cells are associated with the phagocytosis of the damaged elastic fibers of the pleura, because these giant cells are mainly located at the peripheral area showing destruction of elastic fibers of the visceral pleura (Figure 2E).
Although IgG4-related disease shows excellent response to steroid therapy, the definite prognostic factors still remains obscure and the extents of the involved organs also cannot predict the prognosis4. However, it can be supposed that the patients will receive unnecessary operations, if those cases showing concurrent or subsequent pleural and lung lesions are suggested of the mesothelioma or pulmonary malignancies on the clinical and radiological examinations. Therefore, it is important for pathologists to consider the possibility of IgG4-related disease and to rule out the other benign or malignant diseases for the appropriate treatments.
Figures and Tables
Figure 1
Radiologic findings of IgG4-related disease of lung and pleura. (A, C) Chest X-ray (taken 1 year ago) and computed tomography (taken 6 months ago) demonstrate pleural effusion with patchy ground-glass opacity lesions in the right lung. (D) Subsequent computed tomography reveals newly developed, diffuse patchy lesions with pleural thickening and fissural nodularity in both lung, which radiologically suggests mesothelioma or pleural seeding from the lung cancer. (B) These lesions show hot uptake on positron emission tomography. (E) After steroid therapy, the lesions of both lobes are improved with residual small nodule in the left pleura.
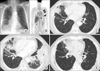
Figure 2
Microscopic findings of IgG4-related disease of lung and pleura (A) Scanned view of the lesion displays pleural thickening and subpleural fibrosis. (B-D, F, G) Infiltrate cells are mainly composed of lymphocytes and plasma cells in the background of dense fibrosis. Dispersed giant cells are also noted in some areas (C, F, and G, H&E stain; B and D, Elastic stain; B, ×12.5; C and D, ×200; E, ×100; F, ×40; G, ×400). (E) Small blood vessels are infiltrated by lymphoplasma cells without fibrinoid necrosis or granuloma formation. Immunohistochemical stainings for IgG (H) and IgG4 (I) reveal increased ratio of IgG4/IgG positive plasma cells, estimated at about 40% (H and I, ×200).
References
1. Zen Y, Inoue D, Kitao A, Onodera M, Abo H, Miyayama S, et al. IgG4-related lung and pleural disease: a clinicopathologic study of 21 cases. Am J Surg Pathol. 2009; 33:1886–1893.
2. Divatia M, Kim SA, Ro JY. IgG4-related sclerosing disease, an emerging entity: a review of a multi-system disease. Yonsei Med J. 2012; 53:15–34.
3. Cheuk W, Chan JK. IgG4-related sclerosing disease: a critical appraisal of an evolving clinicopathologic entity. Adv Anat Pathol. 2010; 17:303–332.
4. Shigemitsu H, Koss MN. IgG4-related interstitial lung disease: a new and evolving concept. Curr Opin Pulm Med. 2009; 15:513–516.
5. Yamashita K, Haga H, Kobashi Y, Miyagawa-Hayashino A, Yoshizawa A, Manabe T. Lung involvement in IgG4-related lymphoplasmacytic vasculitis and interstitial fibrosis: report of 3 cases and review of the literature. Am J Surg Pathol. 2008; 32:1620–1626.
6. Park HY, Han J, Kang G, Yi CA, Chung MP. IgG4-related lung disease presenting as a consolidative mass: a case report. J Lung Cancer. 2010; 9:103–105.
7. Yoo JW, Roh JH, Lim CM, Lee SD, Kim WS, Kim DS, et al. Two cases of pulmonary involvement of immunoglobulin G4 related autoimmune disease. Tuberc Respir Dis. 2009; 67:359–363.
8. Koss M, Travis W, Moran C, Hochholzer L. Pseudomesotheliomatous adenocarcinoma: a reappraisal. Semin Diagn Pathol. 1992; 9:117–123.
9. Kim EY, Kim TS, Han J, Choi JY, Kwon OJ, Kim J. Thoracic epithelioid hemangioendothelioma: imaging and pathologic features. Acta Radiol. 2011; 52:161–166.
10. Zen Y, Fujii T, Sato Y, Masuda S, Nakanuma Y. Pathological classification of hepatic inflammatory pseudotumor with respect to IgG4-related disease. Mod Pathol. 2007; 20:884–894.
11. Yamamoto H, Yamaguchi H, Aishima S, Oda Y, Kohashi K, Oshiro Y, et al. Inflammatory myofibroblastic tumor versus IgG4-related sclerosing disease and inflammatory pseudotumor: a comparative clinicopathologic study. Am J Surg Pathol. 2009; 33:1330–1340.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download