Abstract
Purpose
Cortisol awakening response (CAR) and nighttime cortisol levels have been used as indices of adrenocortical activity. However, population-based statistical information regarding these indices has not been provided in healthy subjects. This study was carried out to provide basic statistical information regarding these indices.
Materials and Methods
Cortisol levels were measured in saliva samples collected immediately upon awakening (0 min), 30 min after awakening and in the nighttime on two consecutive days in 133 healthy subjects.
Results
We determined the mean [standard deviation (SD)], median (interquartile range) and 5th-95th percentile range for each measure and auxiliary indices for CAR, i.e., the secreted cortisol concentration within 30 min of awakening (CARscc) and absolute and relative increases in cortisol level within 30 min of awakening (CARi and CARi%, respectively). We also determined these values for auxiliary indices derived from nighttime cortisol level, i.e., the ratio of cortisol level 30 min after awakening (CA30 min) to nighttime level (CA30 min/NC), as well as absolute and relative decreases in cortisol levels from CA30 min to nighttime (DCd and DCd%, respectively). We found no significant differences in cortisol level for any time point or in auxiliary indices between collection days, genders and ages.
Cortisol is the primary steroid produced in the adrenal cortex. Cortisol secretion is regulated by adrenocorticotropic hormone (ACTH) and shows profound circadian rhythmicity and responsiveness to physical and psychological stressors.1,2 Measurement of cortisol levels in saliva has become more common over the past few years, and it is well documented that the level of cortisol in saliva represents the free form of the steroid found in blood.3 Moreover, collection of saliva is much easier than venipuncture and can readily be repeated at frequent intervals. These advantages provide a better assessment of the diurnal rhythm-mediated endogenous cortisol secretion. Salivary cortisol increases and reaches a peak 30 min after awakening and then decreases to its lowest level at nighttime.4-6
Awakening stimulates ACTH secretion in the pituitary, which then stimulates cortisol secretion in the adrenal glands.7 The rapid increase and peak in cortisol level after awakening is termed the cortisol awakening response (CAR).8 Although it is thought that CAR is a distinct part of diurnal cortisol rhythm, CAR and diurnal cortisol rhythm actually represent two separate adrenocortical activities. CAR signifies the activation of the hypothalamus-pituitary-adrenal (HPA) axis after awakening, and the diurnal cortisol decline represents adrenal secretory activity over the remainder of the diurnal cycle.9
CAR has received much attention from researchers and has been used as an adrenocortical index in various fields. Many studies have shown that altered CAR appears to be associated with psychosocial factors and health. Patients with hippocampal atrophy,10 hypertension11 or psychosomatic disorders such as fatigue, depression, post-traumatic stress disorder (PTSD) and sleep disorders exhibit blunted CAR, but healthy subjects under typical stress, such as job-related stress, exhibit normal or heightened CAR.12
The diurnal cortisol decline and nighttime cortisol levels have also been used as adrenocortical indices. In the allostasis theory, altered diurnal cortisol decline is considered to be indicative of adrenocortical activity when determining allostatic status.13 Patients with metastatic breast cancer,14 in an exhausted state15 or with chronic fatigue syndrome16 have altered diurnal cortisol decline. Some studies have shown that nighttime cortisol level, representing adrenocortical activity, can be used to distinguish patients with Cushing's syndrome from healthy controls.17
Based on these previous findings, it is believed that variation in CAR (i.e., heightened or blunted CAR), altered diurnal cortisol decline and nighttime cortisol levels are closely associated with physical and psychosomatic disorders. The magnitude of the increase in cortisol levels after awakening differed from study to study, but there is consensus that a 50-150% increase in cortisol concentration, as measured in saliva, occurs within an hour after awakening.1 We have also found that there is considerable inter-individual variation in cortisol levels when comparing samples obtained immediately upon awakening to those obtained 30 min after awakening.18
The conspicuous variation of biological parameters is considered to be a manifestation of physiological dysfunctions, genetic differences, and diseases, and knowledge of this variation is a prerequisite for rational interpretation of laboratory results. CAR or diurnal cortisol decline has been used as an index of HPA axis function in various research fields, but the available descriptive statistical information on these indices is rather limited, which hinders attempts to evaluate cortisol secretory activity in individual patients. Therefore, in this study, cortisol levels were determined in saliva samples collected immediately upon awakening, 30 min after awakening and during the night from 133 healthy subjects on two consecutive workdays. We also analyzed changes in cortisol levels within the first 30 min of awakening and from 30 min after awakening to nighttime.
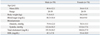
National health insurance companies within Korea support periodic physical examinations for individuals who do not have systemic diseases such as cancer, diabetes, and cardiovascular disease or who have not been hospitalized within the two years following their previous physical examination. Eligible volunteers were enrolled for this study at the time of their periodic physical examination between January and March 2009. None of the selected subjects were diagnosed with diabetes, hypo- or hypertension, a thyroid disorder, adrenal disorder, renal disorder, hepatic disorder or psychiatric disorder. None of the participants was pregnant or a night-shift worker. Individuals undergoing hormone replacement therapy, taking hormones for birth control or taking antidepressant medication or sleeping pills were also excluded. However, it was not possible to trace other minor psychological or physical health issues, such as sporadic or weak pain in the muscles, sleep quality, gastrointestinal trouble or psychological or financial stress among the subjects. General information about the health of the 133 participants is summarized in Table 1.
In total, 171 participants with full-time jobs were initially enrolled in this study. A minimum volume of 1 mL of saliva was collected by expectoration without stimulation. Participants were asked to collect their own saliva samples following their sleep-wake cycle: immediately upon awakening, 30 minutes after awakening and nighttime (before bedtime) for two consecutive workdays. For this purpose, a saliva-collecting pack containing six collecting tubes, a zipper bag and instructions was distributed or delivered to each subject.
Participants were instructed to collect saliva samples at the designated times (<10 min after awakening, 30±5 min after awakening and bedtime) on workdays18-20 and to note each collection time on the marking area of the collecting tube (Simport, QC, Canada). All participants were asked not to drink alcohol on the previous night. During the 30 min before collecting the sample, the participants were asked to not smoke, eat food or drink any fluids, to rinse their mouths with water and refrain from brushing their teeth. Cortisol concentrations are stable after storage of saliva at -20 or -80℃ for up to one year, and repeated freezing and thawing of samples up to four times before analysis would not affect the measured concentrations,21 so participants were asked to keep the saliva samples in their own domestic freezers before sample submission.
Samples contaminated with blood, as determined by visual inspection, were excluded from the study. Samples collected outside of the designated times and those lacking a time or date on the marking area of the tube (n=17) were also excluded. We accepted 154 samples collected from nonclinical subjects (men: n=71, women: n=83) to assay after the selection procedure. All participants provided informed consent and were given information regarding their hormonal levels. The study was conducted in accordance with the Declaration of Helsinki, and the protocol was approved by the institutional review board of Korea University Anam Hospital.
The collected samples were stored at -70℃ after removal of debris. To precipitate mucins, the samples were thawed and centrifuged (10,000 g, 15 min, 4℃).22 The supernatant was collected and stored at -70℃ until the assay was performed.
The steroid levels in saliva were determined by radioimmunoassay (RIA) as previously described.18,23 Iodine-125-labeled cortisol [cortisol-3-(O-carboxymethyl oximino)-2-125I iodohistamine] was obtained from PerkinElmer Life and Analytical Sciences (Waltham, MA, USA). Cortisol antiserum was purchased from AbD Serotec (Oxford, UK). Cortisol antiserum cross-reacts with aldosterone, 11-deoxycorticosterone, 11-deoxycortisol, 21-deoxycortisol, corticosterone and other steroids, with cross-reactions of 0.001%, 4.1%, 5.7%, 0.5%, 1.2% and <0.01%, respectively.
Exogenously added 5.5 nmol/L and 22.1 nmol/L cortisol in charcoal-stripped saliva was determined to be 5.4±0.7 nmol/L (n=20) and 22.9±1.9 nmol/L (n=20), respectively. The inter-assay coefficients of variation (CV) as assessed from quality controls with mean cortisol concentrations of 2.8, 5.3 and 13.7 nmol/L were 7.8%, 10.2% and 14.0%, respectively (n=26). Intra-assay CVs for the same pool were less than 10% (n=15). The analytical sensitivity for cortisol was 1 nmol/L.
Absent CAR has only been reported in patients with hippocampal damage,24 severe global amnesia25 and Asperger syndrome.26 However, the absence of CAR commonly appears when collecting the first sample with a delay of more than 10 minutes after awakening (i.e., non-compliant subject) in healthy subjects.19 The typical CAR is defined as an increase of at least 2.5 nmol/L from baseline cortisol levels in compliant subjects,6 and this value is used as an index for normal cortisol response in research and clinical fields.19 For these reasons, all samples from subjects who exhibited a difference of <2.5 nmol/L in cortisol levels measured immediately upon awakening as compared to 30 minutes after awakening on one of the two collection days (21 subjects) were excluded from all further data analyses after the assay procedure. Cortisol values were lower than 75 nmol/L in all samples, indicating that they had not been contaminated with blood and did not have altered pH.27 Ultimately, the data obtained from saliva samples collected from 133 subjects on two consecutive days (male: n=59; female: n=74) (mean age: 38.0±11.9 years) were included in the present study. The 133 subjects were comprised of 46, 26, 31 and 30 subjects in their twenties, thirties, forties and fifties, respectively.
The mean wake-up time for the 133 subjects on the two consecutive days was 6:23 AM (range: 4:30-7:50 AM, r=0.60). The first saliva sample was collected 5.6±1.8 min after awakening (range, 2-8 min after awakening, coefficient of variation (CV)=35.6%), and the second saliva sample was collected 30.5±4.0 min after awakening (range 25-35 min after awakening, CV=9.8%). Nighttime saliva samples were collected at 22:12±2.48 hours (range: 20:16-00:41 hours, r=0.53).
To obtain auxiliary indices for CAR, the increase in cortisol level during the first 30 min after awakening [CARi, cortisol level 30 min after awakening (CA30 min) - cortisol level immediately upon awakening (CA0 min)] and the relative increase in cortisol level during the first 30 min after awakening (CARi%, [(CA30 min-CA0 min)/CA0 min*100] were calculated for each of the 133 subjects. The secreted cortisol concentration ranging from the time immediately upon awakening to 30 min after awakening {CARscc, [(CA0 min+ CA30 min)/2]*(t30 min-t0 min)} was also calculated for each of the 133 subjects after modification of the previously proposed formula for the area under the curve with respect to baseline value.28 To obtain auxiliary indices for nighttime cortisol concentrations, the ratio between CA30 min and nighttime cortisol (CA30 min/NC), the diurnal decrease in cortisol level (DCd, CA30 min-NC) and the relative diurnal decrease in cortisol level (DCd%, [CA30 min-NC]/CA30 min*100) were also calculated.
Two-way repeated-measures analysis of variance (ANOVA) was applied to reveal the possible effects of different variables (collection day, gender, collection time and collection day) on the log-transformed cortisol levels at each time point and auxiliary index. Group differences in the observed cortisol levels at each time point and auxiliary index were analyzed using the Mann-Whitney test or Kruskal-Wallis test with Dunn's multiple-comparison test. To assess the stability of cortisol levels at each measure and each auxiliary index between two days, Pearson's correlations were computed between cortisol levels across the two sampling days using GraphPad Prism version 5.01 for Windows (San Diego, CA, USA). Simple regression analysis was performed to determine the relationship between each variable included in Table 1 and steroid concentration variable (cortisol levels at each examined time point) using GraphPad Prism. Statistical calculations were performed using SAS version 9.1 (SAS Institute Inc., Cary, NC, USA). All results are presented as mean±standard deviation (SD), and a p value <0.05 was considered significant.
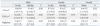
Cortisol levels in the saliva samples collected immediately upon awakening (CA0 min), 30 min after awakening (CA30 min) and at nighttime (NC) for two consecutive days were measured in this study (Fig. 1)(Table 2). The Shapiro-Wilk normality test revealed that the observed CA0 min, CA30 min and NC did not follow a normal distribution (all W with p<0.001) (Fig. 1). The median [interquartile range, (IQR)] values for the observed CA0 min, CA30 min and NC were 7.8 nmol/L (5.0-11.2 nmol/L), 15.4 nmol/L (11.3-22.5 nmol/L) and 2.2 nmol/L (1.6-3.1 nmol/L), respectively. The 5th-95th percentile range for the CA0min was 3.4-17.3 nmol/L; for the CA30 min, it was 7.2-32.8 nmol/L; and for the NC, it was 0.7-5.2 nmol/L (Fig. 1)(Table 2).
Observed CA0 min, CA30 min and NC were also analyzed after logarithmic (log) transformation. The Shapiro-Wilk normality test revealed that the log-transformed CA0 min, CA30 min and NC followed a normal distribution (all W with p>0.05). The log-mean (±SD) value of CA0 min was 0.9±0.2 nmol/L, and that of CA30 min and of NC were 1.2±0.2 nmol/L and 0.3±0.2 nmol/L, respectively. The anti-log values of the log-mean (±SD) CA0 min, CA30 min and NC were 7.7±1.7 nmol/L, 15.8±1.6 nmol/L and 2.2±1.7 nmol/L, respectively.
As seen in Table 2, cortisol levels at each time were comparable in terms of collection days as well as gender. Repeated measures two-way ANOVA revealed that there was no significant collection day or gender effect on cortisol levels immediately upon awakening (CA0 min), 30 min after awakening (CA30 min) or at nighttime (NC)(all F with p>0.05). However, repeated measures two-way ANOVA revealed that there was a significant effect of saliva collection time on cortisol levels ((F2,792=857.2, p<0.001). Since there were no differences in cortisol levels for any measure when comparing the first and second collection days or when comparing males and females, the data at each time point was pooled for the two consecutive days to facilitate analysis.
The observed cortisol levels at each collection time over the first and second collection days were significantly correlated with each other in both genders (r=0.36-0.71, p<0.05 for all analyses) (Table 2). The between-day variation of CA0 min (33.2±20.8%) and NC (32.1±25.5%) was greater than that of CA30 min (21.3±14.9%)(p<0.001 for all analyses). Simple regression analysis revealed that there was no relationship between each variable included in Table and cortisol levels at each examined time point, but nighttime cortisol levels were significantly and positively related to increasing age (F1,131=4.16, p=0.0433 by linear regression analysis).
The auxiliary indices for CAR, the secreted cortisol concentration ranging from the time immediately upon awakening to 30 min after awakening (CARscc), the increased cortisol concentration within 30 min after awakening (CARi) and the relative increase in cortisol concentration 30 min after awakening to immediately upon awakening (CARi%), were calculated from the data obtained for each subject and then analyzed.
The CARscc was distributed in the range from 73.7 nmol/L to 1261.0 nmol/L, and a Shapiro-Wilk normality test revealed that it was not normally distributed (W=0.91, p<0.001), but that log-transformed CARscc followed a normal distribution (W=0.99, p>0.05). CARscc was slightly higher in females (mean: 406.0±188.9 nmol/L) on both collection days than in males (mean: 373.7±183.1 nmol/L).
But a two-way ANOVA test revealed that there was no significant collection day or gender effect on the CARscc (all F with p>0.05). Although the mean values of CARscc for subjects in their twenties (446.2±240.1 nmol/L) were slightly higher than those of other ages examined in this study (30 s-50 s: 340.4-385.8 nmol/L), CARscc was not significantly different among the ages examined (p>0.05, Kruskal-Wallis test with Dunn's multiple-comparison test). CARscc values between the first and second collection days were strongly correlated (r=0.70, p<0.001), and the between-day variation for CARscc was 20.8±16.7%.
CARi was distributed in the range of 2.6 nmol/L to 31.9 nmol/L, and CARi% ranged from 22.7 to 506.9%. Both auxiliary indices were distributed abnormally (all W with p<0.001), but the log-transformed CARi% followed a normal distribution (W=0.99, p>0.05). The CARi% was comparable regarding collection days (1st day; 136.9±121.2%, 2nd day; 126.3±110.7%) and genders (male; 126.5±85.2%, female; 134.7±92.3%). A two-way ANOVA test revealed that there was no significant collection day or gender effect on CARi% (all F with p>0.05). CARi was also similar between the collection days (1st day; 8.6±5.8 nmol/L, 2nd day; 8.7±6.3 nmol/L) and between genders (male; 7.8±4.6 nmol/L, female; 9.1±5.5 nmol/L) (all U with p>0.05). The mean values of CARi for subjects in their twenties (9.7±5.9 nmol/L) were slightly higher than for other age groups examined in this study (30 s-50 s; 8.5-7.4 nmol/L), but these differences were not significant among the ages examined (p>0.05, Kruskal-Wallis test with Dunn's multiple-comparison test). The mean values of CARi% were also comparable among ages examined (20 s-50 s; 126.2-144.7%, p>0.05).
CARi values between the first and second collection days were strongly correlated (r=0.47, p<0.001), and the between-day variation for observed CARi was 33.3±27.0%. The CARi% values on the first and second collection days were weakly but significantly correlated (r=0.27, p<0.005), and the between-day variation for CARi% was 47.9±33.9%.
Median (IQR) values and the 5th-95th percentile range for the CARscc, CARi and CARi%, and the mean (SD) and central 95% interval for the log-transformed CARscc and CARi% are summarized in Table 3.
The molar ratios between CA30 min and NC (CA30 min/NC ratio), the diurnal decrease in cortisol levels from 30 min after awakening to nighttime (DCd) and the relative diurnal decrease in cortisol levels (DCd%) were calculated and analyzed.
The CA30 min/NC ratio ranged from 1.9 to 43.9, and did not follow a normal distribution (W=0.81, p<0.01). However, the log-transformed CA30 min/NC ratio was distributed normally (W=0.99, p>0.05). The CA30 min/NC ratio in females (mean; 9.8±6.6) on both collection days was slightly higher than that of males (8.5±4.2), but a two-way ANOVA test revealed that there was no significant collection day or gender effect on the CA30 min/NC ratio (all F with p>0.05). There was no significant difference in the absolute mean CA30 min/NC ratio among the ages examined (20 s-50 s; 6.8-8.6) (p>0.05, Kruskal-Wallis test with Dunn's multiple-comparison test). There was a weak but significant correlation in the observed CA30 min/NC ratio between the first and second collection days (r=0.35, p<0.001), and the between-day variation for the observed CA30 min/NC ratio was 37.0±27.8%.
DCd ranged from 1.9 to 43.9 nmol/L, and DCd% ranged from 45.3 to 95.3%. DCd and DCd% did not follow a normal distribution (all W with p<0.01). Log-transformed DCd followed a normal distribution (W=0.99, p>0.05), but log-transformed DCd% did not (W=0.79, p<0.01). The mean value of DCd was comparable between females (14.9±7.0 nmol/L) and males (13.5±7.3 nmol/L) and between the first (14.5±8.2 nmol/L) and second (15.5±8.4 nmol/L) collection days (all F with p>0.05). The mean value of DCd% was also similar between males (82.7±10.4%) and females (84.5±9.1%) and between the first (83.1±11.5%) and second (84.5±10.1%) collection days (all U with p>0.05).
There was a weak but significant correlation in DCd% between the first and second collection days (r=0.35, p<0.001), and the between-day variation for DCd% was 10.1±8.2%. A Kruskal-Wallis test with Dunn's multiple-comparison test revealed that there was no age-related difference in CA30 min/NC ratio (20 s-50 s; 8.7-10.9), DCd (20 s-50 s; 12.7-16.9 nmol/L) or DCd% (20 s-50 s; 82.1-86.8%)(p>0.05 for all analyses).
The values of DCd and DCd% on the first and second collection day were significantly correlated (r=0.67 and 0.37, respectively, p<0.001 for all analyses), and the between-day variation for the DCd and DCd% was 25.8±19.1% and 10.2±8.1%, respectively. The statistical information for the observed and log-transformed CA30 min/NC ratio, DCd and DCd% is summarized in Table 4.
Information regarding variations in hormone levels between individuals is essential for the accurate interpretation of laboratory results. Measured cortisol levels or indices for adrenal function in and of themselves are difficult to interpret in routine tests. To overcome this difficulty, the present study provides basic statistical information regarding cortisol levels immediately upon awakening, 30 min after awakening and at nighttime. This study also assessed the additional parameters of the cortisol increase within the first 30 min of awakening and the cortisol decrease from 30 min after awakening to nighttime to increase the understanding of cortisol secretory activity.
Indices for adrenal function, such as cortisol diurnal rhythm, molar cortisol to dehydroepiandrosterone ratio and nighttime cortisol level have been commonly used in various research fields.13 CAR is a relatively new index for the HPA axis,4 and it represents the activation of the HPA axis in response to awakening.7 Knowledge of variations regarding CAR and nighttime cortisol levels in healthy subjects is a basic prerequisite for evaluating HPA axis function. Because a cortisol peak is generally observed 30 minutes after awakening,1,6 we need statistical information or a reference range for each variable, such as cortisol level immediately upon awakening, 30 min after awakening, CARi and CARi%, to correctly interpret individual variations of CAR. Only 14 papers investigating CAR4,6,20,29-39 and three papers proposing a reference range for morning cortisol levels40-42 in healthy subjects were identified after searching for previous studies with the key word "salivary cortisol" in PubMed (1960-June, 2010). However, none of these previous studies provided statistical information to evaluate individual variations in CAR.
There have been study-to-study variations in reported cortisol levels immediately after awakening (15.1-23.4 nmol/L) and 30 minutes after awakening (23.0-34.7 nmol/L) in four population-based studies (n>120).6,20,38,39 Cortisol levels immediately after awakening and 30 minutes after awakening (8.4±5.2 nmol/L and 17.0±8.7, respectively) in the present study were lower than mean values in previous studies, but the CARi in the present study (median; 7.7 nmol/L) was close to that of previous studies (8.0-11.4 nmol/L). This indicates that cortisol levels more steeply within the first 30 minutes increased in our study's subjects (median; 114.1%) than in those of previous studies (mean; 48.3-68.0%). Genetic factors and social stress significantly influence CAR,43 and some studies have also reported racial/ethnic variations in CAR and diurnal cortisol rhythm.44,45 When we account for the racial/ethnic difference in CAR and the significant influence of genetic, social, and environmental factors on CAR, the relatively lower cortisol levels after awakening and the sharper increase in cortisol level indicate a particular characteristic of HPA axis function in the Korean working population.
As the tension and anger experienced in the daytime positively influence the subsequent nighttime cortisol level,46 nighttime cortisol level is considered a transducer of the daytime psychosocial and emotional experiences in healthy subjects. Nighttime cortisol level is also influenced by chronic psychological stress, such as chronic high financial strain and job stress, in healthy subjects.47 Nighttime cortisol level has been used as a first-line screening test in the diagnosis of Cushing's syndrome.48 A single determination of midnight salivary cortisol level or the molar ratio between morning and nighttime cortisol has been a reliable index for discriminating patients with Cushing's syndrome from normal subjects.49,50 A reference range for nighttime has not been proposed. The observed range of nighttime cortisol levels in healthy subjects of previous studies (0.3-15.2 nmol/L)39,49-52 and that of the present study (0.6-7.3 nmol/L) closely overlap. The previously proposed cut-off value of late-nighttime (23:00) salivary cortisol level for the identification of Cush-ing's syndrome in adults (3.6-15.2 nmol/L)51,52 was above the 95th percentile for nighttime cortisol in the present study. The morning to midnight molar cortisol ratio in patients with Cushing's syndrome (1.8±0.4) in a previous study31 was below the 5th percentile for the CA30 min/NC ratio, as determined in this study. Thus, information on nighttime cortisol levels and auxiliary indices for nighttime cortisol levels presented in this study might have clinical relevance for the identification of Cushing's syndrome and altered diurnal cortisol rhythm.
There are no systematic guidelines from a respected body such as the International Federation of Clinical Chemistry (IFCC)53-56 to create reference values and intervals for salivary cortisol. It is also difficult to apply IFCC recommendations to salivary cortisol because cortisol secretory activity shows a profound diurnal rhythm and is affected by psychological and physical stress and genetic factors, as described above. Novel guidelines that designate reference values and intervals for salivary cortisol are needed to make this assessment more useful and available for clinical purposes.
We also found no significant differences in cortisol level for any time point or in the auxiliary indices between collection days, genders and ages, similar to other studies.4,6 However, there are some limitations to this study, one being the relatively small age range of participants. Subjects below 20 and above 60 years of age were not included. Previous studies have shown that age, body mass index and menstruation cycle are not associated with baseline or peak cortisol level.1,36,37 Thus, the present results will help to understand cortisol secretory activity in working-age, active adults as well as younger and older patients. Second, daily stress and cortisol-related minor health issues, such as sporadic fatigue and sleep disorders, were not fully examined in each subject, and the effects of these parameters on cortisol secretory activity was not included in this study. Although chronic diseases and economic, psychological and daily stress influence cortisol secretory activity,12 we do not yet fully understand the nature of these relationships. Thus, given our selective inclusion and exclusion criteria for cortisol-related acute and sporadic minor health issues, this dataset may be helpful in creating reference ranges for salivary cortisol. Third, we did not objectively monitor the saliva collecting time. To avoid the effect of delayed collection on measured CAR, saliva samples collected outside of the designated time were excluded from the inspection stage. All samples from subjects who exhibited a difference of <2.5 nmol/L in cortisol levels measured immediately upon awakening as compared to 30 minutes after awakening on one of the two collection days were considered non-complaint, and all of their samples were excluded from this study. Accurate saliva sampling is critical for the assessment and interpretation of cortisol profiles, and electronic monitoring devices will be helpful to objectively monitor saliva collection time and improve adherence to the designated collection time.19
Overall, collection of saliva is much easier than venipuncture and can readily be repeated at frequent intervals. These advantages provide a better assessment of the subtle changes in diurnal rhythm-mediated endogenous cortisol secretion. Confounding factors of CAR and nighttime cortisol level have been identified, and guidelines for the collection of saliva samples and psychosomatic and psychiatric symptoms associated with HPA axis dysfunction have also been well-documented.1,12 Therefore, knowledge of the variations in CAR and nighttime cortisol levels will be helpful towards understanding the laboratory results of each individual subject. For these reasons, we provided descriptive statistics regarding CAR and salivary nighttime cortisol level in a Korean working population. The information provided in the present study will be of value to medical specialists and researchers involved in HPA axis assessment.
Figures and Tables
Fig. 1
Cortisol levels immediately upon awakening (A), 30 min after awakening (B), and at nighttime (C). Cortisol levels were determined from saliva samples collected immediately upon, 30 min after awakening and at nighttime from 133 healthy subjects over two consecutive days. The data at each time point was pooled for the two consecutive days. Boxes represent the interquartile range (IQR), whiskers represent the 5th-95th percentile range, and outliers are represented by closed circles. Horizontal lines and the cross symbol within the boxes represent the median and mean cortisol values, respectively.

ACKNOWLEDGEMENTS
This work was supported by a Grant from the Korean Ministry of Education, Science and Technology (The Regional Core Research Program/Biohousing Research Institute).
References
1. Clow A, Thorn L, Evans P, Hucklebridge F. The awakening cortisol response: methodological issues and significance. Stress. 2004. 7:29–37.

2. Hucklebridge F, Hussain T, Evans P, Clow A. The diurnal patterns of the adrenal steroids cortisol and dehydroepiandrosterone (DHEA) in relation to awakening. Psychoneuroendocrinology. 2005. 30:51–57.

3. Vining RF, McGinley RA, Maksvytis JJ, Ho KY. Salivary cortisol: a better measure of adrenal cortical function than serum cortisol. Ann Clin Biochem. 1983. 20:329–335.

4. Pruessner JC, Wolf OT, Hellhammer DH, Buske-Kirschbaum A, von Auer K, Jobst S, et al. Free cortisol levels after awakening: a reliable biological marker for the assessment of adrenocortical activity. Life Sci. 1997. 61:2539–2549.

5. Edwards S, Evans P, Hucklebridge F, Clow A. Association between time of awakening and diurnal cortisol secretory activity. Psychoneuroendocrinology. 2001. 26:613–622.

6. Wüst S, Wolf J, Hellhammer DH, Federenko I, Schommer N, Kirschbaum C. The cortisol awakening response - normal values and confounds. Noise Health. 2000. 2:79–88.
7. Wilhelm I, Born J, Kudielka BM, Schlotz W, Wüst S. Is the cortisol awakening rise a response to awakening? Psychoneuroendocrinology. 2007. 32:358–366.

8. Federenko I, Wüst S, Hellhammer DH, Dechoux R, Kumsta R, Kirschbaum C. Free cortisol awakening responses are influenced by awakening time. Psychoneuroendocrinology. 2004. 29:174–184.

9. Schmidt-Reinwald A, Pruessner JC, Hellhammer DH, Federenko I, Rohleder N, Schürmeyer TH, et al. The cortisol response to awakening in relation to different challenge tests and a 12-hour cortisol rhythm. Life Sci. 1999. 64:1653–1660.

10. Buchanan TW, Kern S, Allen JS, Tranel D, Kirschbaum C. Circadian regulation of cortisol after hippocampal damage in humans. Biol Psychiatry. 2004. 56:651–656.

11. Wirtz PH, von Känel R, Emini L, Ruedisueli K, Groessbauer S, Maercker A, et al. Evidence for altered hypothalamus-pituitary-adrenal axis functioning in systemic hypertension: blunted cortisol response to awakening and lower negative feedback sensitivity. Psychoneuroendocrinology. 2007. 32:430–436.

12. Chida Y, Steptoe A. Cortisol awakening response and psychosocial factors: a systematic review and meta-analysis. Biol Psychol. 2009. 80:265–278.

13. McEwen BS, Wingfield JC. The concept of allostasis in biology and biomedicine. Horm Behav. 2003. 43:2–15.

14. Palesh O, Zeitzer JM, Conrad A, Giese-Davis J, Mustian KM, Popek V, et al. Vagal regulation, cortisol, and sleep disruption in women with metastatic breast cancer. J Clin Sleep Med. 2008. 4:441–449.

15. Lindeberg SI, Eek F, Lindbladh E, Ostergren PO, Hansen AM, Karlson B. Exhaustion measured by the SF-36 vitality scale is associated with a flattened diurnal cortisol profile. Psychoneuroendocrinology. 2008. 33:471–477.

16. Nater UM, Maloney E, Boneva RS, Gurbaxani BM, Lin JM, Jones JF, et al. Attenuated morning salivary cortisol concentrations in a population-based study of persons with chronic fatigue syndrome and well controls. J Clin Endocrinol Metab. 2008. 93:703–709.

17. Gafni RI, Papanicolaou DA, Nieman LK. Nighttime salivary cortisol measurement as a simple, noninvasive, outpatient screening test for Cushing's syndrome in children and adolescents. J Pediatr. 2000. 137:30–35.

18. Kim MS, Lee YJ, Ahn RS. Day-to-day differences in cortisol levels and molar cortisol-to-DHEA ratios among working individuals. Yonsei Med J. 2010. 51:212–218.

19. Kudielka BM, Broderick JE, Kirschbaum C. Compliance with saliva sampling protocols: electronic monitoring reveals invalid cortisol daytime profiles in noncompliant subjects. Psychosom Med. 2003. 65:313–319.

20. Schlotz W, Hellhammer J, Schulz P, Stone AA. Perceived work overload and chronic worrying predict weekend-weekday differences in the cortisol awakening response. Psychosom Med. 2004. 66:207–214.

21. Gröschl M, Wagner R, Rauh M, Dörr HG. Stability of salivary steroids: the influences of storage, food and dental care. Steroids. 2001. 66:737–741.

22. Gozansky WS, Lynn JS, Laudenslage ML, Kohrt WM. Salivary cortisol determined by enzyme immunoassay is preferable to serum total cortisol for assessment of dynamic hypothalamic--pituitary--adrenal axis activity. Clin Endocrinol (Oxf). 2005. 63:336–341.

23. Ahn RS, Lee YJ, Choi JY, Kwon HB, Chun SI. Salivary cortisol and DHEA levels in the Korean population: age-related differences, diurnal rhythm, and correlations with serum levels. Yonsei Med J. 2007. 48:379–388.

24. Buchanan TW, Kern S, Allen JS, Tranel D, Kirschbaum C. Circadian regulation of cortisol after hippocampal damage in humans. Biol Psychiatry. 2004. 56:651–656.

25. Wolf OT, Fujiwara E, Luwinski G, Kirschbaum C, Markowitsch HJ. No morning cortisol response in patients with severe global amnesia. Psychoneuroendocrinology. 2005. 30:101–105.

26. Brosnan M, Turner-Cobb J, Munro-Naan Z, Jessop D. Absence of a normal cortisol awakening response (CAR) in adolescent males with Asperger syndrome (AS). Psychoneuroendocrinology. 2009. 34:1095–1100.

27. Steptoe A, Siegrist J, Kirschbaum C, Marmot M. Effort-reward imbalance, overcommitment, and measures of cortisol and blood pressure over the working day. Psychosom Med. 2004. 66:323–329.

28. Pruessner JC, Kirschbaum C, Meinlschmid G, Hellhammer DH. Two formulas for computation of the area under the curve represent measures of total hormone concentration versus time-dependent change. Psychoneuroendocrinology. 2003. 28:916–931.

29. Hucklebridge F, Clow A, Evans P. The relationship between salivary secretory immunoglobulin A and cortisol: neuroendocrine response to awakening and the diurnal cycle. Int J Psychophysiol. 1998. 31:69–76.

30. Hucklebridge F, Sen S, Evans PD, Clow A. The relationship between circadian patterns of salivary cortisol and endogenous inhibitor of monoamine oxidase A. Life Sci. 1998. 62:2321–2328.

31. Hucklebridge FH, Clow A, Abeyguneratne T, Huezo-Diaz P, Evans P. The awakening cortisol response and blood glucose levels. Life Sci. 1999. 64:931–937.

32. Pruessner JC, Hellhammer DH, Kirschbaum C. Burnout, perceived stress, and cortisol responses to awakening. Psychosom Med. 1999. 61:197–204.

33. Schmidt-Reinwald A, Pruessner JC, Hellhammer DH, Federenko I, Rohleder N, Schürmeyer TH, et al. The cortisol response to awakening in relation to different challenge tests and a 12-hour cortisol rhythm. Life Sci. 1999. 64:1653–1660.

34. Edwards S, Clow A, Evans P, Hucklebridge F. Exploration of the awakening cortisol response in relation to diurnal cortisol secretory activity. Life Sci. 2001. 68:2093–2103.

35. Brooke-Wavell K, Clow A, Ghazi-Noori S, Evans P, Hucklebridge F. Ultrasound measures of bone and the diurnal free cortisol cycle: a positive association with the awakening cortisol response in healthy premenopausal women. Calcif Tissue Int. 2002. 70:463–468.

36. Kirschbaum C, Kudielka BM, Gaab J, Schommer NC, Hellhammer DH. Impact of gender, menstrual cycle phase, and oral contraceptives on the activity of the hypothalamus-pituitary-adrenal axis. Psychosom Med. 1999. 61:154–162.

37. Kudielka BM, Kirschbaum C. Awakening cortisol responses are influenced by health status and awakening time but not by menstrual cycle phase. Psychoneuroendocrinology. 2003. 28:35–47.

38. Kunz-Ebrecht SR, Kirschbaum C, Marmot M, Steptoe A. Differences in cortisol awakening response on work days and weekends in women and men from the Whitehall II cohort. Psychoneuroendocrinology. 2004. 29:516–528.

39. Sjögren E, Leanderson P, Kristenson M. Diurnal saliva cortisol levels and relations to psychosocial factors in a population sample of middle-aged Swedish men and women. Int J Behav Med. 2006. 13:193–200.

40. Aardal E, Holm AC. Cortisol in saliva--reference ranges and relation to cortisol in serum. Eur J Clin Chem Clin Biochem. 1995. 33:927–932.
41. Hansen AM, Garde AH, Christensen JM, Eller NH, Netterstrøm B. Evaluation of a radioimmunoassay and establishment of a reference interval for salivary cortisol in healthy subjects in Denmark. Scand J Clin Lab Invest. 2003. 63:303–310.

42. Patel RS, Shaw SR, Macintyre H, McGarry GW, Wallace AM. Production of gender-specific morning salivary cortisol reference intervals using internationally accepted procedures. Clin Chem Lab Med. 2004. 42:1424–1429.

43. Wüst S, Federenko I, Hellhammer DH, Kirschbaum C. Genetic factors, perceived chronic stress, and the free cortisol response to awakening. Psychoneuroendocrinology. 2000. 25:707–720.

44. Cohen S, Schwartz JE, Epel E, Kirschbaum C, Sidney S, Seeman T. Socioeconomic status, race, and diurnal cortisol decline in the Coronary Artery Risk Development in Young Adults (CARDIA) Study. Psychosom Med. 2006. 68:41–50.

45. DeSantis AS, Adam EK, Doane LD, Mineka S, Zinbarg RE, Craske MG. Racial/ethnic differences in cortisol diurnal rhythms in a community sample of adolescents. J Adolesc Health. 2007. 41:3–13.

46. Adam EK, Hawkley LC, Kudielka BM, Cacioppo JT. Day-to-day dynamics of experience--cortisol associations in a population-based sample of older adults. Proc Natl Acad Sci U S A. 2006. 103:17058–17063.

47. Grossi G, Perski A, Lundberg U, Soares J. Associations between financial strain and the diurnal salivary cortisol secretion of long-term unemployed individuals. Integr Physiol Behav Sci. 2001. 36:205–219.

48. Carroll T, Raff H, Findling JW. Late-night salivary cortisol measurement in the diagnosis of Cushing's syndrome. Nat Clin Pract Endocrinol Metab. 2008. 4:344–350.

49. Yaneva M, Mosnier-Pudar H, Dugué MA, Grabar S, Fulla Y, Bertagna X. Midnight salivary cortisol for the initial diagnosis of Cushing's syndrome of various causes. J Clin Endocrinol Metab. 2004. 89:3345–3351.

50. Raff H, Raff JL, Findling JW. Late-night salivary cortisol as a screening test for Cushing's syndrome. J Clin Endocrinol Metab. 1998. 83:2681–2686.

51. Castro M, Elias PC, Quidute AR, Halah FP, Moreira AC. Out-patient screening for Cushing's syndrome: the sensitivity of the combination of circadian rhythm and overnight dexamethasone suppression salivary cortisol tests. J Clin Endocrinol Metab. 1999. 84:878–882.

52. Papanicolaou DA, Mullen N, Kyrou I, Nieman LK. Nighttime salivary cortisol: a useful test for the diagnosis of Cushing's syndrome. J Clin Endocrinol Metab. 2002. 87:4515–4521.

53. Solberg HE. The theory of reference values Part 5. Statistical treatment of collected reference values. Determination of reference limits. J Clin Chem Clin Biochem. 1983. 21:749–760.

54. Solberg HE. International Federation of Clinical Chemistry (IFCC). Scientific Committee. Clinical Section. Expert Panel on Theory of Reference Values. International Committee for Standardization in Haematology (ICSH), Standing Committee on Reference Values. Approved Recommendation (1986) on the theory of reference values. Part 1. The concept of reference values. J Clin Chem Clin Biochem. 1987. 25:337–342.

55. Solberg HE, PetitClerc C. International Federation of Clinical Chemistry (IFCC). Scientific Committee. Clinical Section. Expert Panel on Theory of Reference Values. Approved recommendation (1988) on the theory of reference values. Part 3. Preparation of individuals and collection of specimens for the production of reference values. J Clin Chem Clin Biochem. 1988. 26:593–598.

56. Solberg HE, Stamm D. International Federation of Clinical Chemistry, Scientific Division: approved recommendation on the theory of reference values. Part 4. Control of analytical variation in the production, transfer and application of reference values. Eur J Clin Chem Clin Biochem. 1991. 29:531–535.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download