Abstract
Objective
To define the MRI findings of congenital high airway obstruction sequence (CHAOS) in a series of fetuses.
Materials and Methods
Prenatal fetal MR images were reviewed in seven fetuses with CHAOS at 21 to 27 weeks of gestation. The MRI findings were reviewed. The MRI parameters evaluated included the appearance of the lungs and diaphragm, presence or absence of hydrops, amount of amniotic fluid, airway appearance, predicted level of airway obstruction, and any additional findings or suspected genetic syndromes.
Results
All the fetuses viewed (7 of 7) demonstrated the following MRI findings: dilated airway below the level of obstruction, increased lung signal, markedly increased lung volumes with flattened or inverted hemidiaphragms, massive ascites, centrally positioned and compressed heart, as well as placentomegaly. Other frequent findings were anasarca (6 of 7) and polyhydramnios (3 of 7). MRI identified the level of obstruction as laryngeal in five cases and tracheal in two cases. In four of the patients, surgery or autopsy confirmed the MRI predicted level of obstruction. Associated abnormalities were found in 4 of 7 (genetic syndromes in 2). Postnatal radiography (n = 3) showed markedly hyperinflated lungs with inverted or flattened hemidiaphragms, strandy perihilar opacities, pneumothoraces and tracheotomy. Two fetuses were terminated and one fetus demised in utero. Four fetuses were delivered via ex utero intrapartum treatment procedure.
Conclusion
MRI shows a consistent pattern of abnormalities in fetuses with CHAOS, accurately identifies the level of airway obstruction, and helps differentiate from other lung abnormalities such as bilateral congenital pulmonary airway malformation by demonstrating an abnormally dilated airway distal to the obstruction.
Congenital high airway obstruction sequence (CHAOS) is a rare, life-threatening condition characterized by complete or near complete intrinsic obstruction of the fetal airway. CHAOS has been considered an almost invariably fatal condition (1) which often goes incorrectly diagnosed until autopsy. However, advances in prenatal imaging, earlier diagnosis in utero, in utero surgical treatment, and delivery via ex utero intrapartum treatment (EXIT) to tracheostomy may contribute to improving the outcome of this condition (1-7). With the exception of case reports (2, 8-10), there is little in the literature describing the MRI findings of CHAOS. We present the MRI findings in a series of seven fetuses with prenatal diagnosis of CHAOS. To our knowledge, this is the largest described series of patients with CHAOS and the first article focusing on the description of MRI findings.
This study was approved by the Internal Review Board at our institution and patient written consent was waived.
We retrospectively reviewed the fetal MR findings of seven fetuses with CHAOS imaged at our institution from 2004 to 2007.
All fetuses were imaged using a 1.5 Tesla scanner (Horizon, General Electric Medical Systems, Milwaukee, WI). The mothers were placed primarily on lateral decubitus, while a torso phased array coil was used to obtain the images. All fetuses were evaluated with a single shot fast spin echo sequence. The sequences were performed using a matrix of 224×192, a field-of-view of 30 or less, and a slice thickness of 3 or 4 mm. Coronal, sagittal, and axial imaging of the head/neck, chest, and abdomen of each fetus was reviewed.
The MR parameters evaluated included lung and diaphragm appearance, presence or absence of hydrops, amount of amniotic fluid, airway dilatation, predicted level of airway obstruction, and any additional abnormalities or suspected genetic syndromes. Airway dilatation was determined to be present if the distal airway was greater in diameter than the proximal airway. The level of airway obstruction was predicted by absence of visualized fluid-filled airway at the upper margin of the dilated fluid-filled airway. Lungs were considered enlarged when the diaphragm was flattened or inverted. The classification for the amount of amniotic fluid, which were normal, polyhydramnios, or oligohydramnios, was subjectively evaluated by MRI and confirmed by the amniotic fluid index obtained by an ultrasound performed on the same date. Hydrops was defined by the presence of two or more of the following: ascites, soft tissue edema, pericardial effusion, pleural effusion, and placentomegaly (11). Placentomegaly was defined by a placental thickness of more than 4 cm (12).
The predicted level of airway obstruction, based on MR findings, was compared to the available results of postnatal surgery, prenatal intervention, or autopsy.
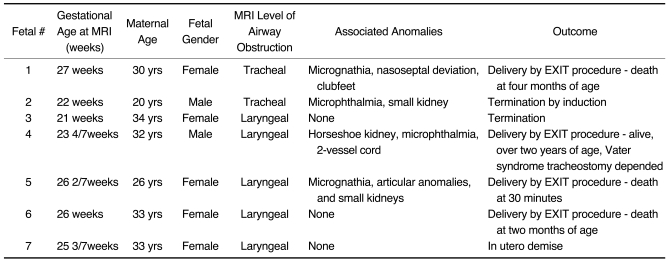
Results from the seven fetuses identified with CHAOS are summarized in Table 1. The gestational age of the fetuses varied from 21 to 27 weeks of gestation.
All fetuses (7 of 7) demonstrated MRI findings of a dilated airway below the level of obstruction, and included an increase in the lung signal, markedly increased lung volumes with flattened or inverted hemidiaphragms, centrally positioned and compressed heart, ascites, and placentomegaly (Figs. 1-3). The trachea and distal airway were dilated in six of the seven fetuses, whereas airway dilatation was isolated to the bronchi in the remaining fetus of the group (1 of 7).
Other frequent findings included anasarca, which was observed in six of the seven fetuses, and polyhydramnios, which was seen in three of the seven fetuses. Oligohydramnios was seen in two of the seven fetuses. Both of these cases were associated with kidney abnormalities. One fetus presented with a small pericardial effusion. There were no pleural effusions.
MRI predicted airway obstruction level was at the level of the larynx in five fetuses and the trachea in two fetuses.
Two fetuses were terminated and one fetus demised in utero. Four fetuses were delivered via EXIT procedure. Two patients underwent a prenatal ultrasound-guided fetoscopic laser laryngotomy. In one patient, the fetoscopic surgery was aborted due to the proximity of the airway obstruction to the vocal cords. In the second patient, the procedure was successfully performed; however, a perioperative premature rupture of membranes resulted in early delivery by EXIT procedure to tracheostomy. The airway obstruction levels confirmed by the above procedures were identical to the levels predicted by MRI. In the three remaining patients, the level of airway obstruction was not confirmed.
One fetus in this study had two MRIs performed; one at 23 weeks of gestation and a follow up at 33 weeks. We noted significant improvement in the findings on follow up MRI. We speculate that this was attributed to in utero perforation of the airway obstruction. In this case, the finding of ascites, increased lung volume, and signal were significantly improved. The only persisting abnormal finding was airway dilatation below the original anatomic site of airway obstruction (Fig. 3).
Associated abnormalities were found on MRI in four fetuses. One had microphthalmia, auricular abnormalities, and small kidneys. Another had a horseshoe kidney, microphthalmia, and a 2-vessel cord. Yet another had micrognathia, nasoseptal deviation, and clubfeet. Lastly, another had microphthalmia and small kidneys. In summary, three fetuses had renal anomalies and three had microphthalmia.
A postnatal radiography was obtained in three of the seven patients. All showed markedly hyperinflated lungs with flattened or inverted hemidiaphragms, strandy perihilar opacities, pneumothoraces, tracheotomy, and enlarged abdomen, likely due to ascites (Fig. 4).
Congenital high airway obstruction sequence is a rare condition characterized by a single identifiable abnormality leading to a pattern of severe life-threatening abnormalities in the affected fetuses. The primary abnormality is an intrinsic obstruction of the upper airway. Causes of obstruction include laryngeal atresia, laryngeal web, laryngeal cyst, and tracheal atresia or stenosis. The obstructed airway causes decreased clearance of fluid produced by the fetal lungs as well as an increase in intratracheal pressure resulting in lung hyperexpansion and abnormal development (1, 2). In addition, there is thinning of the alveolar walls, a decreased number of type II pneumocytes, and a resulting decreased surfactant proportional to the duration of the tracheal obstruction (13). The hyperexpanded lungs cause compression of the heart and inferior vena cava, decreasing venous return and leading to nonimmune hydrops (1, 2, 8). These series of events are responsible for the prenatal imaging characteristics of CHAOS. Our series of cases show that fetuses with CHAOS have typical prenatal MR imaging findings, which include increased lung signal, markedly increased lung volumes with flattened or inverted hemidiaphragms, a dilated airway below the level of obstruction, massive ascites, centrally positioned and compressed heart, and placentomegaly.
The identification of airway obstruction is key to establishing the diagnosis of CHAOS and to differentiating it from bilateral lung masses such as a bilateral congenital pulmonary airway malformation (CPAM) or other causes of extrinsic airway obstruction such as a double aortic arch (9). In this series, MRI showed an abnormally dilated airway distal to the level of obstruction in all fetuses. These findings are not easily identified by ultrasound. Interestingly, two patients were referred to our institution for further evaluation with prior ultrasound diagnosis of bilateral CPAM. The MRI was able to identify the correct diagnosis of high airway obstruction, not seen on prior ultrasound, and change the prognosis and management of those fetuses.
Important advances in perinatal surgical procedures have recently been made improving the survival rate and outcome in several prenatally diagnosed conditions, including CHAOS (2, 6, 7). The EXIT procedure is used to ensure adequate uteroplacental gas exchange, until the airway is evaluated and secured (4, 14). The surgical/obstetrical literature uniformly agrees that CHAOS patients should be delivered via EXIT to tracheostomy (1-5). There have been several reports of in utero improvement of CHAOS due to spontaneous perforation or fistulization of the airway obstruction (2, 7, 10). The improvement of patients with spontaneous perforations of the obstruction suggest that an intrauterine fetoscopic laser laryngotomy may be helpful in treating selected cases of fetuses with CHAOS. For adequate antenatal surgical procedures in the treatment of CHAOS, early diagnosis and accurate evaluation of obstruction level are important.
One fetus in our series showed a marked improvement of almost all of the findings on a follow up MRI. We assume this was a result of an in utero perforation of the airway obstruction or fistulization of the obstructing membrane. This patient is the only patient alive in our series and is now two years old. Interestingly, the only finding that did not improve after the suspected perforation was the airway dilatation below the area of obstruction. Persistent airway dilatation was also described in a case report of improved MR imaging findings in a postnatally confirmed case of in utero tracheo-esophageal fistula development in a fetus with CHAOS (10).
Most cases of CHAOS are sporadic, however, several genetic syndromes have been linked with CHAOS. Moreover, the most commonly associated genetic syndrome is Fraser syndrome, which is characterized by a variable expression of laryngeal atresia, cryptophthalmos, syndactyly, renal agenesis, and abnormalities of the ears and external genitalia (2, 15). Fetal MRI has also been an important tool in identifying these associated abnormalities and suspect genetic syndromes. The accurate identification of associated syndromes help with management decisions and parental counseling. Several fetuses in this series had associated abnormalities; genetic syndromes were confirmed in two fetuses.
Live born neonates with CHAOS often have several postnatal symptoms/abnormalities including respiratory distress caused by the abnormal development of the lungs, diaphragmatic dysfunction likely caused by stretching of the diaphragm, tracheomalacia and capillary leak syndrome (2). Three of our patients experienced postnatal imaging and all showed the same characteristics at conventional radiography: markedly hyperinflated lungs with flattened or inverted hemidiaphragms, strandy perihilar opacities, pneumothoraces, tracheotomy, and enlarged abdomen likely due to ascites. Despite the improvements in imaging and treatment, few infants with CHAOS survive over the long-term. Only one patient from this series is still alive. In the surviving patients, airway reconstruction after adequate child growth and clinical stabilization is attempted in order to improved quality of life (16). However, since few of these infants survive outside of the nursery, true long-term outcome is unknown at this point. Further longitudinal studies of the surviving infants need to be performed.
In conclusion, MRI shows a consistent pattern of abnormalities in fetuses with CHAOS including an interrupted airway, dilatation of the more distal airway, markedly increased lung volumes with flattened or everted hemidiaphragms, centrally positioned and compressed heart, ascites, and placentomegaly. MRI accurately identifies the level of airway obstruction, helping to differentiate from other lung pathologies such as bilateral CPAM. Fetal MRI also helps to identify associated abnormalities and possible associated genetic syndromes, playing an important role in parental counseling and surgical/delivery planning.
References
1. Hedrick MH, Ferro MM, Filly RA, Flake AW, Harrison MR, Adzick NS. Congenital high airway obstruction syndrome (CHAOS): a potential for perinatal intervention. J Pediatr Surg. 1994; 29:271–274. PMID: 8176604.

2. Lim FY, Crombleholme TM, Hedrick HL, Flake AW, Johnson MP, Howell LJ, et al. Congenital high airway obstruction syndrome: natural history and management. J Pediatr Surg. 2003; 38:940–945. PMID: 12778398.

3. Shimabukuro F, Sakumoto K, Masamoto H, Asato Y, Yoshida T, Shinhama A, et al. A case of congenital high airway obstruction syndrome managed by ex utero intrapartum treatment: case report and review of the literature. Am J Perinatol. 2007; 24:197–201. PMID: 17372858.

4. DeCou JM, Jones DC, Jacobs HD, Touloukian RJ. Successful ex utero intrapartum treatment (EXIT) procedure for congenital high airway obstruction syndrome (CHAOS) owing to laryngeal atresia. J Pediatr Surg. 1998; 33:1563–1565. PMID: 9802816.

5. Crombleholme TM, Sylvester K, Flake AW, Adzick NS. Salvage of a fetus with congenital high airway obstruction syndrome by ex utero intrapartum treatment (EXIT) procedure. Fetal Diagn Ther. 2000; 15:280–282. PMID: 10971081.

6. Paek BW, Callen PW, Kitterman J, Feldstein VA, Farrell J, Harrison MR, et al. Successful fetal intervention for congenital high airway obstruction syndrome. Fetal Diagn Ther. 2002; 17:272–276. PMID: 12169810.

7. Kohl T, Hering R, Bauriedel G, Van de Vondel P, Heep A, Keiner S, et al. Fetoscopic and ultrasound-guided decompression of the fetal trachea in a human fetus with Fraser syndrome and congenital high airway obstruction syndrome (CHAOS) from laryngeal atresia. Ultrasound Obstet Gynecol. 2006; 27:84–88. PMID: 16308883.

8. Onderoglu L, Saygan Karamursel B, Bulun A, Kale G, Tuncbilek E. Prenatal diagnosis of laryngeal atresia. Prenat Diagn. 2003; 23:277–280. PMID: 12673628.
9. Shum DJ, Clifton MS, Coakley FV, Hornberger LK, Joe BN, Goldstein RB, et al. Prenatal tracheal obstruction due to double aortic arch: a potential mimic of congenital high airway obstruction syndrome. AJR Am J Roentgenol. 2007; 188:W82–W85. PMID: 17179331.

10. Kuwashima S, Kitajima K, Kaji Y, Watanabe H, Watabe Y, Suzumura H. MR imaging appearance of laryngeal atresia (congenital high airway obstruction syndrome): unique course in a fetus. Pediatr Radiol. 2008; 38:344–347. PMID: 18071686.

11. Ulreich S, Gruslin A, Nodell CG, Pretorius DH. Nyberg DA, McGahan JP, Pretorius DH, Pilu G, editors. Fetal hydrops and ascites. Diagnostic imaging of fetal anomalies. 2003. Philadelphia: Lippincott Williams & Wilkins;p. 713.
12. Sepulveda W, Sebire NJ, Harris R, Nyberg DA. Nyberg DA, McGahan JP, Pretorius DH, Pilu G, editors. The placenta, umbilical cord, and membranes. Diagnostic imaging of fetal anomalies. 2003. Philadelphia: Lippincott Williams & Wilkins;p. 85.
13. Davey MG, Hooper SB, Tester ML, Johns DP, Harding R. Respiratory function in lambs after in utero treatment of lung hypoplasia by tracheal obstruction. J Appl Physiol. 1999; 87:2296–2304. PMID: 10601181.
14. Mychaliska GB, Bealer JF, Graf JL, Rosen MA, Adzick NS, Harrison MR. Operating on placental support: the ex utero intrapartum treatment procedure. J Pediatr Surg. 1997; 32:227–230. PMID: 9044127.

15. Berg C, Geipel A, Germer U, Pertersen-Hansen A, Koch-Dorfler M, Gembruch U. Prenatal detection of Fraser syndrome without cryptophthalmos: case report and review of the literature. Ultrasound Obstet Gynecol. 2001; 18:76–80. PMID: 11489232.

16. Hartnick CJ, Rutter M, Lang F, Willging JP, Cotton RT. Congenital high airway obstruction syndrome and airway reconstruction: an evolving paradigm. Arch Otolaryngol Head Neck Surg. 2002; 128:567–570. PMID: 12003589.
Fig. 1
27-week-old fetus with congenital high airway obstruction sequence.
A. Coronal T2-weighted single shot fast spin echo image shows markedly enlarged lung volumes (L) and increase in lung signal, marked ascites (A), and dilated bronchi bilaterally (arrows).
B. Sagittal T2-weighted single shot fast spin echo image once again shows inverted diaphragm (arrowheads), ascites (A), dilated bronchus (arrow) and subcutaneous edema (black arrows).
C. Axial T2-weighted single shot fast spin echo image shows centrally positioned and compressed heart (H), dilated bronchi (arrows), large lung volumes (L), and subcutaneous edema (black arrow).
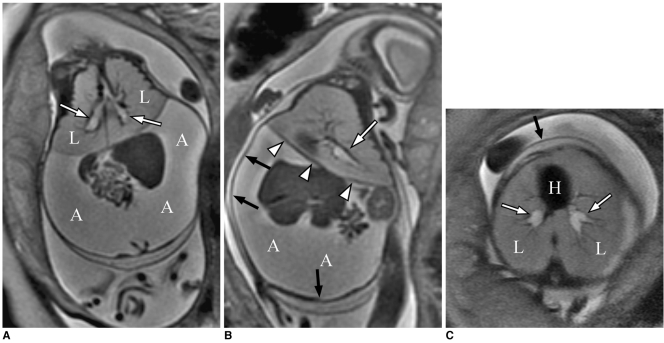
Fig. 2
22-week-old fetus with congenital high airway obstruction sequence.
A. Axial T2-weighted single shot fast spin echo image shows marked placentomegaly (P). Note that fetus has centrally positioned and compressed heart (H), and large lung volumes (L).
B. Coronal T2-weighted single shot fast spin echo image shows markedly enlarged lung volumes (L) and increase in lung signal, marked ascites (A), and dilated airway (arrow). Note inverted diaphragms.
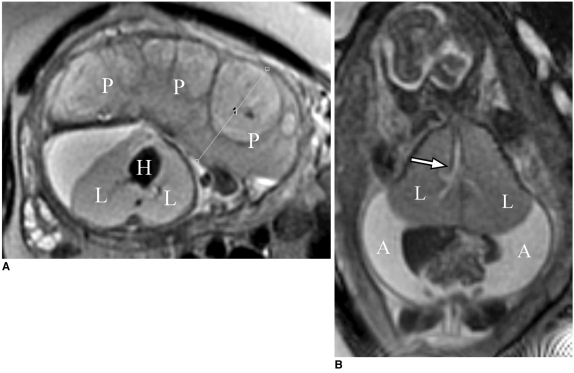
Fig. 3
Congenital high airway obstruction sequence with decreased imaging findings on follow up fetal MR imaging.
A. Sagittal T2-weighted single shot fast spin echo image obtained at 23-weeks of gestation shows markedly enlarged lung volumes (L) and increased lung signal, marked ascites (A), and inverted diaphragms (arrows). Note gap seen in fluid-filled, high-signal airway (arrowheads) at level of larynx, consistent with level of obstruction.
B. Sagittal T2-weighted single shot fast spin echo image obtained at 33-weeks of gestation shows marked interval reduction in degree of ascites (A), marked decrease in lung volume with resolution of inverted diaphragm (arrows). Gap seen in fluid-filled, high-signal airway at level of larynx is still seen. However, airway distal to level of obstruction (arrowhead) remains dilated.
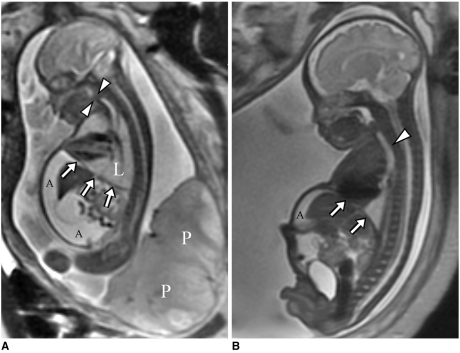
Fig. 4
Radiograph of chest and abdomen in 1-day-old child with congenital high airway obstruction sequence, delivered by ex utero intrapartum treatment to tracheostomy. Note markedly hyperinflated lungs with flattened hemidiaphragms, strandy perihilar opacities, pneumothoraces, tracheotomy, and enlarged abdomen, which is likely due to ascites. Child expired at 2-months of age.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download