INTRODUCTION
The essential aspect of treating patients with poisoning is to ascertain what the toxic substance is, the extent of its toxicity, and how to treat it. In order to provide rapid access to information for the treatment of toxic substances, the United States has been offering Poisindex (
1) since 1985, while the United Kingdom has been operating Toxbase (
2) online since 1999. According to a survey conducted in Australia, the most used electronic resource was Poisindex, though after accessing Toxinz, 64% of respondents indicated that they preferred Toxinz (
3). However, there are limitations to using such databases in non-English speaking countries due to language issues.
In Korea, a web-based poisoning information database (PIDB) has been constructed within the Toxicity Information Service System with the support of the National Institute of Food and Drug Safety Evaluation in order to provide emergency treatment information in Korean for poisoning patients (
4). The PIDB began with the compilation of treatment information for 50 substances in 2007, and with the addition of common and clinically important toxic substances each year, the PIDB provides acute treatment information for 470 substances as of the end of 2014.
Hence, the authors aimed to determine how much help the PIDB actually provides for the treatment of poisoning in the emergency department (ED). For this purpose, the authors planned to investigate the distribution of toxic substances in domestic ED patients and assess their inclusion in the PIDB, in order to suggest the scope of additional toxic substances that should be included in the PIDB in the future.
MATERIALS AND METHODS
Investigation of domestic toxic substances
The distribution of toxicity patients showed regional variation; thus, data was extracted from 20 hospitals across the country in order to determine the distribution at the national level: four hospitals in Seoul, two in Gyeonggi-do, two in Busan, two in Daejeon, two in Daegu, two in Gwangju, two in Chungcheong-do, one in Gangwon-do, one in Jeolla-do, one in Gyeongsangnam-do, and one in Jeju-do. After verifying the willingness of clinical toxicologists at these hospitals to participate, the participating hospitals were confirmed. Patients with poisoning who visited the ED at each hospital between January 1 and December 31, 2013 were selected, and a retrospective analysis of their medical records was performed. Patients with poisoning were selected as those with a final diagnosis pertaining to diagnostic codes T36–65, and all types of toxicity were included, such as bites, inhalation, and drug intoxication.
From the medical records, each patient's age, sex, number of toxic substances, route of exposure, and substance names were verified. In the case of combination drugs, the main toxic substances were recorded. For example, although the common over-the-counter analgesic Geworin is a combination drug comprising acetaminophen, isopropylantipyrine, and caffeine, it was summarized as the main ingredient, acetaminophen. Formulations for which it was difficult to determine the representative ingredient, such as herbal preparations, were classified by brand name. Patients who had been exposed to several substances were analyzed for each individual exposure. Thus, a patient who consumed three types of drugs was analyzed as three cases of exposure. Patients for whom the precise substance name could not be determined from the medical records were marked as unknown.
Comparison with the PIDB
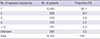
Toxic substances revealed to be the cause were checked for inclusion among the 470 toxic substances registered in the PIDB. Using the Tox-Info classification system, these substances were classified as Medical Drug, Pesticide, Household Chemical, Animal or Plant, Herbal Medicine, or Other. Even if the precise substance name was not available from the medical records, if the type of substance could be determined, it was classified according to the above categories, and when the type could not be determined, it was marked as unknown.
The number of toxic substances, route of exposure, and frequency of exposure for each substance were analyzed by type. Additionally, the frequency of inclusion in the PIDB was calculated by type. The coverage rate was defined as “the number of substances included in the PIDB/total number of toxic substances.”
Data analysis was performed using descriptive statistics, with continuous variables summarized as the mean and standard deviation and categorical variables summarized as frequency and percentage.
Ethics statement
This study was approved by the institutional review board of Gangnam Severance Hospital (#3-2013-0305), and informed consent was waived by the board.
DISCUSSION
Representative databases providing information about toxic substances include the Micromedex Poisindex system of the United States, containing information for over 400,000 toxic substances, and Toxbase of the United Kingdom, containing information for 14,000 types of toxic substances. However, such systems are difficult to use for emergency physicians in non-English speaking countries. One representative database provided in Korean is the Toxicity Information Service System (Tox-Info), which has been operated by the National Institute of Food and Drug Safety Evaluation since 2007 (
http://www.nifds.go.kr/toxinfo/Index). Tox-info is composed of four information databases including toxicity, poisoning, consumer product, and tobacco databases (
4). As of 2014, there were 1,300 items in the toxicity database, which provides information on the characteristics of toxic substances, and in the PIDB, which provides treatment information for emergency patients, 470 toxic substances were registered. Approximately 50 to 60 substances are added to PIDB every year after review by expert panels. Each PIDB entry takes the form of a systematic review article that includes the following subtitles: Clinical Introduction, Toxicology/Toxicokinetics, Clinical Pattern in Acute Toxicity, Diagnosis of Toxicity, Field and Emergency Treatment, Expert Treatment or Antidotes, and Cautions in Pregnancy.
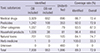
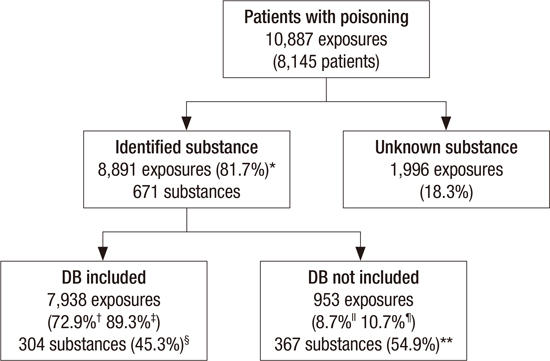
The analysis of patients with poisoning who visited one of 20 EDs in 2013 revealed that 671 toxic substances caused toxicity and 10,887 cases involved toxic exposure. Of these, 72.9% were caused by toxic substances registered in the PIDB, and the coverage rate was 89.3% when cases with an unknown causative substance were excluded. Thus, although there are only a small number of substances (470 as of 2014) registered in the PIDB, the high coverage rate is thought to demonstrate that the most common toxic substances were included in the database. Indeed, all of the 20 most common substances were already registered in the PIDB.
In this study, excluding duplicates, 304 of the 671 types of toxic substances (45.3%) were found to be registered in the PIDB. Of the 470 substances registered in the PIDB due to their clinical importance, 168 substances (35.7%) were not actually encountered in clinical practice.
Among the substances that actually caused toxicity yet were not registered in the database, there were 602 cases of toxicity for 211 types of drugs. Of these, the drugs with the highest number of toxicity cases were diazepam (121 cases), benztropine (24 cases), and flurazepam (16 cases). There were also 108 cases of toxicity for 58 types of pesticides not included in the database; the most common were flocoumafen (12 cases), clothianidin (five cases), and flubendiamide (five cases). Additionally, there were 133 cases of toxicity for 32 types of plants or animals, of which the most common were mushrooms (51 cases), pokeweed (27 cases), thistle (eight cases), and shellfish (eight cases), and there were 38 cases of toxicity for 28 types of household substances.
The distribution of toxic substances is known to show considerable regional variations. Looking at the distribution of toxic substances in Korea reported by So et al. (
5), pesticides were most common at 30.7%; however, in a study by Oh et al. (
6), drugs were most common at 41.5%. In this study, in order to reduce regional differences, 20 hospitals were selected evenly from across the country. However, there are limitations in predicting the national distribution of toxicity, and a national poisoning registry needs to be developed. In this study, by type, 49.7% of the toxic substances were drugs, and 15.6% were pesticides. Of the drugs, the most common were zolpidem and acetaminophen, and of the pesticides, the most common were paraquat and glyphosate. The sale of paraquat was banned due to high mortality at the end of 2012, and it is expected that toxicity cases will decline when the existing supplies are used up. A single-center study showed that the number of suicide attempters with paraquat decreased after the paraquat ban, while the proportion of glyphosate and glufosinate increased (
7).
In this study, the most commonly reported toxic substance was carbon monoxide (CO). In the past, CO poisoning was usually unintentional poisoning caused by carbon boilers; however, since 2009, there has been a rapid increase in the number of intentional cases, and the causes are becoming more diverse (
89).
In the United States, the most common toxic substances are analgesics (11.5%), followed by cosmetics/personal care products (7.7%), household cleaning substances (7.6%), and sedatives/hypnotics/antipsychotics (5.9%); however, the frequency of toxicity from sedatives is rapidly increasing (
10).
During the analysis of the PIDB, confusion was caused when the drug class name and generic name were both included. For example, when a class name such as benzodiazepine and generic names such as alprazolam and lorazepam were both registered, it was not obvious whether substances such as midazolam or diazepam should be considered under the benzodiazepine class or as generic drugs that needed to be newly registered. In this study, pharmaceutical drugs were classified according to generic name. However, pesticides were classified separately, as the class name of pesticides can be easily verified from the Korean Guidelines for the Use of Pesticides. In order to prevent this confusion, the US National Poison Data System (NPDS) database uses 1,081 unified generic codes. These are divided into 68 major categories and 172 subcategories and are regularly updated by the American Association of Poison Control Centers–Micromedex Joint Coding Group (
10).
In cases of plants, particularly mushrooms, it is often difficult to verify the precise species. The PIDB already includes amatoxin (Amanita), psilocybin, orellanine, Podostroma cornu-damae, Ganoderma lucidum, Phellinus linteus, and Ramaria mushrooms; however, there is a need to consider including other toxic mushrooms in Korea that were classified as “not included” in this study, such as Panaeolus, Russula, and Fomes mushrooms.
This study had several limitations. First, this study compared toxic substances causing actual poisoning with 470 substances registered in the currently constructed PIDB and did not analyze whether the information in the PIDB was actually used in the treatment of poisoning patients. If the Tox-Info website were improved in the future to make it possible to measure download counts, this would help to ascertain the extent of use for each substance. Second, as this was a multicenter, retrospective study of medical records, there was a possibility selection error in the process of selecting toxicity patients at each hospital. The number of poisoning patients at each hospital during one year showed large discrepancies, ranging from 144 to 1,088 patients. Moreover, in the case of ethanol, although there were only 534 cases, it is likely that this number only included a fraction of the actual number of hospital visits, thus demonstrating the tendency to exclude acute ethanol intoxication from the scope of poisoning. Third, there were 1,996 cases (18.3%) in which the precise substance causing toxicity in the patient was unknown, which could have caused deviation in the distribution of toxic substances.
In spite of these limitations, the PIDB in 2014 included 89.3% of the identifiable toxic substances in actual cases, demonstrating that, despite the low number of included substances, the database can be usefully applied to actual clinical practice. Nevertheless, as the PIDB only dealt with 45.3% of the toxic substances to which patients were actually exposed and preferences of prescription drugs continued to change, regular updates and additions of toxic substances are required. Particularly, substance categories for which the coverage rate was revealed to be less than 90%, such as medical drugs and natural toxins, should be added with high priority. Finally, it is recommended that the Tox-Info website be revised to be able to count the number of visitors or downloads of the PIDB materials.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download