Abstract
Background and Purpose
The one-day rivastigmine patch is reportedly well tolerated and has minimal side effects. However, Asian patients show more side effects than those in Western countries. We evaluated tolerability of the rivastigmine patch in South Korean patients with Alzheimer's disease (AD) and the specific factors affecting adverse events of the skin.
Methods
A 6-month, open labeled, multi-centered, observational study was carried out in 440 patients with probable AD from July 2009 to September 2010 (NCT01312363).
Results
A total of 25.9% of the patients experienced adverse skin events at the rivastigmine patch application site and 17.0% discontinued treatment due to adverse events at the skin application site. The most common adverse events were itching and erythema. Patients with an allergic history and users of electric heating appliances reported skin discomfort. Older age was associated with discontinuing treatment.
Rivastigmine has recently been approved in patch formulation for treating mild-to-moderate Alzheimer's disease (AD). The rivastigmine transdermal patch has the potential or induce to minimize blood drug level fluctuations, reduce side effects, and optimize efficacy to provide smooth and continuous drug delivery through the skin.1,2 The 10 cm2 (9.5 mg/day) rivastigmine patch carries similar efficacy to the highest dose of rivastigmine capsule (12 mg/day) but with a superior tolerability profile, caregiver preference, and improved tolerability.3,4,5
Transdermal patches are in constant contact with the skin; thus, they can cause adverse skin reactions.6 The expected side effects of the rivastigmine patch are associated with skin irritations, which is common with other medical patches.7 However, only a few data have been reported on side effects of the rivastigmine patch, such as skin irritation, from Western countries compared with Asian countries.
Many differences exist between Western and Asian countries, such as habits, skin types, and behaviors, which could influence patch tolerability.
The objective of this study was to investigate tolerability of the rivastigmine patch in South Korean patients with AD under actual practical conditions. The incidence of adverse events (AEs) of the skin and factors affecting skin AEs were evaluated.
The inclusion criteria for this study were those established for probable AD by the National Institute of Neurological and Communicative Disorders and Stroke-Alzheimer's Disease and Related Disorders Association,8 age 51-90 years, Mini-Mental State Examination (MMSE) score of 10-26, brain magnetic resonance imaging or computed tomography scan within 12 months that was consistent with a diagnosis of probable AD and showing no clinical evidence of other diseases capable of producing a dementia syndrome, and a reliable caregiver who met the patient at least once weekly and was sufficiently familiar with the patient to provide the investigator with accurate information. The exclusion criteria included any primary neurodegenerative disorder or psychiatric disorder other than AD; clinically significant laboratory abnormalities, such as an abnormal thyroid function test, abnormally low level of vitamin B12 or folate or a positive Venereal Disease Research Laboratory test; history of drug or alcohol addiction in the past 10 years; any severe or unstable medical disease that could prevent completing all study requirements; hearing or visual impairment that could disturb the patient evaluation; and involvement in another clinical trial or treated by any experimental drug within 4 weeks. Medical history was based on family history of dementia, hypertension, diabetes mellitus (DM), hypercholesterolemia, heart disease, and depression and was evaluated at the first visit.
The study was conducted at 22 institutions throughout South Korea in accordance with the Declaration of Helsinki and good clinical reporting practices. The study protocol and informed consent form were reviewed and approved by the Institutional Review Board at each center before the study began. The patients and their legal guardians or a representative gave written informed consent to participate in this study.
This was a 24-week, open labeled, multi-center, observational study. All eligible patients were treated with a 5 cm2 (4.6 mg/day) rivastigmine patch for the first 4 weeks of the run-in period and then the dosage was increased to the target rivastigmine patch size of 10 cm2 (9.5 mg/day), with adjustments as necessary for safety and tolerability. If a patient reported too much discomfort using the high dose patch, an investigator assessed the severity of the side effects and adjusted the dose or considered discontinuation of the study. After patients found their highest, well-tolerated patch size, it was maintained for the remaining 20 weeks of the study. The caregiver applied the patches on the patient's upper or lower back, either upper arm, or on the chest in clean, dry locations. The patches were exchanged every 24 hours and placed in a different location.
The safety and tolerability data were derived from participants who had received at least one dose of the study medication and had undergone at least one safety evaluation. The efficacy assessment was performed at baseline (week 0) and the end of the study (week 24), and safety was monitored at every visit on weeks 0, 4, 8, 12, and 24.
All AEs and serious AEs were recorded at each study visit. Investigators were asked to evaluate severity, relationship with the study drug, and seriousness of the AEs. Skin condition at the application site was monitored by an investigator at every visit. The symptoms monitored by the investigators were erythema, itching, blister, urticaria, pain, and burning; severity (very slight, mild, or moderate); and location (limited or extended).
Environmental monitoring factors, such as residence type, bed type, heating or cooling system type, and bathing frequency per week were evaluated. In addition, history of allergy, humidifier use, and the patient's skin type were compared with the first visit using an evaluation form. Patients and their caregivers were asked at every visit about concerns or problems associated with using the patch. Finally, patients who discontinued the study prematurely were evaluated through regular visits for the primary endpoint.
The patch discontinuation rate in previous studies5,14 was 10.7%. The additional drop-out caused by ethnic and environmental factors was assumed to be about 10% in this study. We set α=0.05, and a power of 80% with two-sided 1-β=0.80 to calculate the two proportion comparisons for superiority. According to the calculation, 209 patients were needed. Additionally, assuming a loss of up to 50% of patients, which was reported in a previous Korean study in patients with AD,15 the final sample size was more than 309 patients.
Continuous variables are presented as means±standard deviation, and categorical variables are presented as frequencies and percentages. Demographics and clinical characteristics were compared according to skin AEs, using Student's t-test for continuous variables and the chi-square test for categorical variables. Potential factors affecting skin AEs were entered into a multivariate logistic analysis regression and the odds ratios with 95% confidence intervals were reported. A p-value <0.05 were considered significant. Statistical analyses were performed using SPSS 20.0 (SPSS Inc., Chicago, IL, USA).
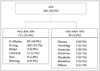
The study was conducted from July 2009 to September 2010, and 440 patients were enrolled. Mean age was 75.9±7.2 years, the majority of patients (68.8%) were female, and the mean education level was 6.0±4.9 years. A total of 157 patients (35.7%) discontinued the study during the 24 weeks. Finally, 283 patients completed the rivastigmine patch therapy (Fig. 1).
The number of patients reporting at least one AE over the 24-week study period was 126 (28.6%). A total of 114 patients (25.9%) reported skin AEs during the run-in period. The most frequently reported skin AE was itching (23.2%), followed by erythema (18.9%). Eighteen patients (4.2%) reported another AE. The most frequently reported other AE was nausea (0.9%), followed by dizziness (0.7%) and headache (0.7%) (Fig. 2).
The clinical characteristics according to skin AEs are shown in Table 1. No significant differences were observed for age, sex, education, or medical history (family history of dementia, hypertension, DM, hypercholesterolemia, heart disease, and depression). More patients with skin AEs had a history allergy than those without skin AEs (χ2=6.32, df=1, p=0.02). More patients with skin AEs used a cooling fan (χ2=4.50, df=1, p=0.04) and an electric heating appliance (χ2=11.71, df=1, p<0.01). Patients with skin AEs had a lower CDR score (t=2.51, p=0.01) and a lower CDR-SB score (t=2.44, p=0.02). Additionally, patients with skin AEs had a lower rate of DM compared with that of patients with no skin AEs (12.9% vs. 15.8%, p=0.04). No significant differences were observed in the other clinical characteristics, such as skin disease, dry skin type, air conditioner use, bathing frequency, humidifier use, systolic and diastolic blood pressures, body mass index, MMSE score, IADL, or GDpS score.
The types of skin AEs, severity of the skin AEs, and patch size are shown in Table 2. The frequencies of any skin AE were 8.4% at week 4, 18.7% at week 8, 19.1% at week 16, and 14.8% at week 24. The frequencies of discontinuation due to any skin AE were 3.0% at week 4, 6.6% at week 8, 7.4% at week 16, and 1.7% at week 24. Sixty-six patients (22.2%) were using the 5 cm2 patch at 24 weeks.
Among all patients who discontinued the study (n=157), 78 (49.7%) had an AE, and 75 (47.8%) had a skin AE. The type of skin AEs that most frequently led to discontinuation was itching, followed by erythema, pain, urticaria, burning, and blistering. The other AEs that most frequently led to discontinuation were nausea, followed by dizziness. Most patients experienced very slight or mild skin AEs.
Among 114 patients with skin lesions, 85 (19.3%) had a limited skin lesion and 29 (6.6%) had an extended skin lesion at the application site (Fig. 3). Among patients with limited skin lesions, 35 (41.2%) completed the study, and 50 (58.8%) did not (drop-out). Among patients with extended skin lesions, 4 (13.8%) completed and 25 (86.2%) did not complete the study.
A multivariate logistic regression analysis was performed with variables associated (p<0.05 or <0.10) with skin AEs in the initial univariate analysis to identify predictors of skin AEs. Both analyses showed that an allergy history and using an electric heating appliance were associated with skin AEs (Table 3).
The predictors of study discontinuation due to skin AEs in the multivariate logistic regression analysis were older age, erythema skin lesions, more severe skin AEs, and skin AEs in a broad area (Table 4).
We evaluated skin tolerability to the rivastigmine patch in patients with AD under actual conditions. We also evaluated the incidence and reasons for dropping out of the study, the incidence and types of skin AEs, and factors affecting skin AEs. Our results may contribute to understand and improve tolerability to the rivastigmine patch.
Skin tolerability profiles of the rivastigmine patch have been reported previously.2,5,6,16,17,18,19,20,21,22 Some patients treated with the rivastigmine transdermal patch may develop a skin AE, as with other kinds of medical patches. No, slight, or mild skin irritations in the Investigation of transDermal Exelon in ALzheimer's disease (IDEAL) study5 ranged from 90% to 98% across four patch sizes (5, 10, 15, and 20 cm2). The percentage of patients who discontinued the study as a result of a skin irritation from the rivastigmine patch was 1-2%. Skin tolerability of the rivastigmine patch during the open-label extension phase of the IDEAL was generally similar to that observed in the double-blind phase of the IDEAL.6 In a Japanese study,17 85.1% of participants using the 5 cm2 rivastigmine patch and 83.2% of participants using the 10 cm2 patch had no, slight, or mild skin irritations. The most common severe skin irritation was erythema from the 5 cm2 patch and pruritus from the 10 cm2 patch. Skin irritations were observed in 42.0% of patients using the rivastigmine patch plus memantine and 34.9% of patients using the rivastigmine patch only in the Korean Exelon Patch and Combination With Memantine Comparative Trial (EXPECT) study.2 In a German study,18 8.7% of patients developed erythema and 8.2% of patients developed pruritus. The most common AE leading to study discontinuation was a skin and subcutaneous tissue disorder (7.2% of patients). In the Slovenian EXTRA NEW study,19 14.09% of patients had skin reactions. In a Thai study,20 14.2-15.8% of patients developed an itching AE. In a Belgium study,22 26.9% of patients experienced skin adverse reactions. The most commonly reported AE leading to treatment discontinuation in the Canadian EMBRACE study21 was a skin and subcutaneous tissue disorder (9.4%). Our results show that 25.9% of patients had skin AEs and 17.0% of patients with skin AEs in discontinued treatment. Taken together, these results suggest some differences between the prevalence of skin irritation across study groups and that skin AEs led to treatment discontinuation in 7.2-17.0% of cases. These data also suggest that skin tolerability to rivastigmine was generally favorable if care was taken.
The most common skin AEs in our study were itching and erythema. Previous studies showed similar results and2,5,6,16,17,18,19,20,21,22 these skin reactions were localized, usually appearing after 1-4 months of treatment and decreased in intensity after removing the patch. These skin reactions were typically mild erythema (redness) and itching (pruritus), caused by contact irritation, and were not followed by any serious medical problem. Allergic dermatitis with use of the rivastigmine patch is rare, and typically manifests as localized redness with swelling but may spread beyond the patch border.
The main factors associated with a risk of developing skin AEs are patch-related factors and clinical characteristics. Patch-related factors include the patch substance in contact with skin, substance concentration, size of the contact area, and contact duration.6,23,24 It was reported that the rivastigmine patch causes more skin irritations than that in comparably sized placebo patches, suggesting that rivastigmine itself could be an additional irritant or allergen.6 Second, the clinical characteristics of skin AEs are sex, age, and medical factors.25 Women have a higher tendency towards developing allergic dermatitis, whereas the evidence is more controversial for sex associations with the development of irritant dermatitis. However, we found no relationship between clinical characteristics and skin AEs. Skin tends to become less elastic, undergoes epidermal thinning, become less resistant to shearing, more likely to be torn after trauma, and has less ability to heal with age.6,26,27 Therefore, elderly subjects are more prone to develop irritant dermatitis but they may be at a decreased risk for allergic dermatitis. Because of these factors, elderly patients, such as those with AD, tend to have fragile skin that requires a more cautious approach, particularly with respect to avoiding mild-to-moderate erythema caused by removing a patch.28 Medical factors include pre-existing skin conditions, sensitivity to any patch component, and a medical history of allergy. Excess sweating increases the risk for a skin AE.29 However, the IDEAL study included a number of countries that experience high temperatures where heavy perspiration is expected, and no noticeable difference were reported.14
In this study, we identified predictable skin AEs and the factors predicting treatment discontinuation due to a skin AE. The predictive factors we found were an allergy history and use of an electric heating appliance. The association between allergy history and skin irritation is easily assumed; however, the association with electric heating appliances is less obvious. Patients with AD stay indoors most of the day because of mobility limitations may more frequently use these appliances. Use of an electric heating appliance will dry the skin and affects the immune system and the etiology of allergy.30,31 We also showed that the patch treatment was discontinued due to skin AEs in older aged subjects, those with erythema skin lesions, more severe and extended lesion locations.
In conclusion, our results show that the rivastigmine patch is generally tolerable in patients with AD in an actual environment. Our results could contribute to improve tolerability to treating patients with AD. Further study with the rivastigmine patch is needed to confirm our results, which that could have practical implications in the daily management of patients with AD.
Figures and Tables
Table 3
Predictors of skin adverse events

Data are presented as odds ratios (95% confidence intervals) from a multivariate logistic regression analysis with two models. Model 1 was performed with variables associated (p<0.05) with skin adverse events in the initial univariate analysis. Model 2 was performed with variables associated (p<0.10) with skin adverse events in the initial univariate analysis.
CDR: Clinical Dementia Rating, CDR-SB: CDR-sum of boxes scores.
References
1. Oertel W, Ross JS, Eggert K, Adler G. Rationale for transdermal drug administration in Alzheimer disease. Neurology. 2007; 69:4 Suppl 1. S4–S9.

2. Choi SH, Park KW, Na DL, Han HJ, Kim EJ, Shim YS, et al. Tolerability and efficacy of memantine add-on therapy to rivastigmine transdermal patches in mild to moderate Alzheimer's disease: a multicenter, randomized, open-label, parallel-group study. Curr Med Res Opin. 2011; 27:1375–1383.

3. Winblad B, Kawata AK, Beusterien KM, Thomas SK, Wimo A, Lane R, et al. Caregiver preference for rivastigmine patch relative to capsules for treatment of probable Alzheimer's disease. Int J Geriatr Psychiatry. 2007; 22:485–491.

4. Lee JH, Sevigny J. Effects of body weight on tolerability of rivastigmine transdermal patch: a post-hoc analysis of a double-blind trial in patients with Alzheimer disease. Alzheimer Dis Assoc Disord. 2011; 25:58–62.

5. Winblad B, Cummings J, Andreasen N, Grossberg G, Onofrj M, Sadowsky C, et al. A six-month double-blind, randomized, placebo-controlled study of a transdermal patch in Alzheimer's disease--rivastigmine patch versus capsule. Int J Geriatr Psychiatry. 2007; 22:456–467.

6. Cummings JL, Farlow MR, Meng X, Tekin S, Olin JT. Rivastigmine transdermal patch skin tolerability: results of a 1-year clinical trial in patients with mild-to-moderate Alzheimer's disease. Clin Drug Investig. 2010; 30:41–49.
7. Widman TJ, Oostman H, Storrs FJ. Allergic contact dermatitis from medical adhesive bandages in patients who report having a reaction to medical bandages. Dermatitis. 2008; 19:32–37.

8. McKhann G, Drachman D, Folstein M, Katzman R, Price D, Stadlan EM. Clinical diagnosis of Alzheimer's disease: report of the NINCDSADRDA Work Group under the auspices of Department of Health and Human Services Task Force on Alzheimer's Disease. Neurology. 1984; 34:939–944.

9. Kang Y, Na DL, Hahn S. A validity study on the Korean Mini-Mental State Examination (K-MMSE) in dementia patients. J Korean Neurol Assoc. 1997; 15:300–308.
10. Morris JC. The Clinical Dementia Rating (CDR): current version and scoring rules. Neurology. 1993; 43:2412–2414.
11. Choi SH, Na DL, Lee BH, Hahm DS, Jeong JH, Yoon SJ, et al. Estimating the Validity of the Korean Version of Expanded Clinical Dementia Rating (CDR) Scale. J Korean Neurol Assoc. 2001; 19:585–591.
12. Bae JN, Cho MJ. Development of the Korean version of the Geriatric Depression Scale and its short form among elderly psychiatric patients. J Psychosom Res. 2004; 57:297–305.

13. Ku HM, Kim JH, Kwon EJ, Kim SH, Lee HS, Ko HJ, et al. A study on the reliability and validity of Seoul-instrumental activities of daily livings (S-IADL). J Korean Neuropsychiatr Assoc. 2004; 43:189–199.
14. Winblad B, Grossberg G, Frölich L, Farlow M, Zechner S, Nagel J, et al. IDEAL: a 6-month, double-blind, placebo-controlled study of the first skin patch for Alzheimer disease. Neurology. 2007; 69:4 Suppl 1. S14–S22.

15. Choi SH, Kim SY, Na HR, Kim BK, Yang DW, Kwon JC, et al. Effect of ApoE genotype on response to donepezil in patients with Alzheimer's disease. Dement Geriatr Cogn Disord. 2008; 25:445–450.

16. Darreh-Shori T, Jelic V. Safety and tolerability of transdermal and oral rivastigmine in Alzheimer's disease and Parkinson's disease dementia. Expert Opin Drug Saf. 2010; 9:167–176.

17. Nakamura Y, Imai Y, Shigeta M, Graf A, Shirahase T, Kim H, et al. A 24-week, randomized, double-blind, placebo-controlled study to evaluate the efficacy, safety and tolerability of the rivastigmine patch in Japanese patients with Alzheimer's disease. Dement Geriatr Cogn Dis Extra. 2011; 1:163–179.

18. Articus K, Baier M, Tracik F, Kühn F, Preuss UW, Kurz A. A 24-week, multicentre, open evaluation of the clinical effectiveness of the rivastigmine patch in patients with probable Alzheimer's disease. Int J Clin Pract. 2011; 65:790–796.

19. Pregelj P. Safety and tolerability of rivastigmine transdermal patch formulation in newly diagnosed patients with Alzheimer's dementia in naturalistic conditions. Psychogeriatrics. 2012; 12:165–171.

20. Kulkantrakorn K, Tanyakitpisal P, Towanabut S, Dejthevaporn C, Rangseekajee P, Pongpakdee S, et al. Rivastigmine patch for treatment of Alzheimer's disease in clinical practice in Thailand. Psychogeriatrics. 2013; 13:1–8.

21. Gauthier S, Robillard A, Cohen S, Black S, Sampalis J, Colizza D, et al. Real-life effectiveness and tolerability of the rivastigmine transdermal patch in patients with mild-to-moderate Alzheimer's disease: the EMBRACE study. Curr Med Res Opin. 2013; 29:989–1000.

22. Segers K, Cytryn E, Surquin M. Do local meteorological conditions influence skin irritation caused by transdermal rivastigmine? A retroprospective, pilot study. J Clin Psychopharmacol. 2012; 32:412–415.

23. Upadhye MR, Maibach HI. Influence of area of application of allergen on sensitization in contact dermatitis. Contact Dermatitis. 1992; 27:281–286.

24. Hurkmans JF, Boddé HE, Van Driel LM, Van Doorne H, Junginger HE. Skin irritation caused by transdermal drug delivery systems during long-term (5 days) application. Br J Dermatol. 1985; 112:461–467.

25. Ale I, Lachapelle JM, Maibach HI. Skin tolerability associated with transdermal drug delivery systems: an overview. Adv Ther. 2009; 26:920–935.

26. Waller JM, Maibach HI. Age and skin structure and function, a quantitative approach (I): blood flow, pH, thickness, and ultrasound echogenicity. Skin Res Technol. 2005; 11:221–235.

27. Waller JM, Maibach HI. Age and skin structure and function, a quantitative approach (II): protein, glycosaminoglycan, water, and lipid content and structure. Skin Res Technol. 2006; 12:145–154.

28. Fisher AA. Dermatitis due to transdermal therapeutic systems. Cutis. 1984; 34:526–527.
29. Beltrani VS, Beltrani VP. Contact dermatitis. Ann Allergy Asthma Immunol. 1997; 78:160–173. quiz 174-176.

30. Di Giampaolo L, Di Donato A, Antonucci A, Paiardini G, Travaglini P, Spagnoli G, et al. Follow up study on the immune response to low frequency electromagnetic fields in men and women working in a museum. Int J Immunopathol Pharmacol. 2006; 19:4 Suppl. 37–42.




 PDF
PDF ePub
ePub Citation
Citation Print
Print







 XML Download
XML Download