Abstract
Giant serpentine aneurysms are uncommon types of aneurysmal disease and have angiographically authentic features. We report a case of a 44-year-old male with headache and seizure. He presented a giant serpentine aneurysm arising from the middle cerebral artery (MCA). It was a large intracranial aneurysm thrombosed as a mass-like lesion while it maintained its outflow drainage into the distal MCA branches. The balloon occlusion test (BOT) was performed to test the tolerance of temporary collateral circulation. Following routine cerebral angiography, we performed an endovascular embolization on the proximal artery of MCA. He was discharged from the hospital with alert mental status and mild Gerstmann syndrome. The short-term follow-up imaging studies showed the decreased mass effect, and the patient presented an improved Gerstmann syndrome. After a careful evaluation of BOT, an endovascular embolization can be one of the powerful therapeutic instruments for giant serpentine aneurysm.
Giant serpentine aneurysm is rare and its endovascular treatment is usually considered to be technically challenging. Since its first description in 1977, a giant serpentine aneurysm is now known to be a subgroup of large aneurysms with a persistent serpentine vascular channel.3)7)9) Its size is usually > 25 mm in diameter with a partial filling of thrombus in the sac.3)6)9) The blood flow passing through the aneurysm is usually slow and the aneurysmal sac is connected to the distal branch of a feeding artery causing a mass effect. Due to the presence of thrombus with calcification, it can be large enough to create a mass effect along with a midline shift. It often comes along with cerebral edema mimicking a brain tumor in the brain computed tomography (CT).6)10) Classical neurosurgical operation was considered most of time for the debulking purposes. However, as the recent endovascular treatment is evolved with a cutting-edge high-level technique, neurosurgeons are now given alternative treatment options to treat this disease entity. We experienced an interesting case of giant serpentine aneurysm which was treated with endovascular embolization with a selective balloon occlusion test (BOT).
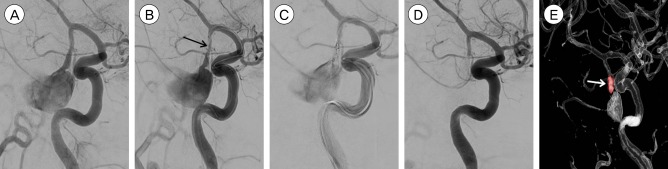
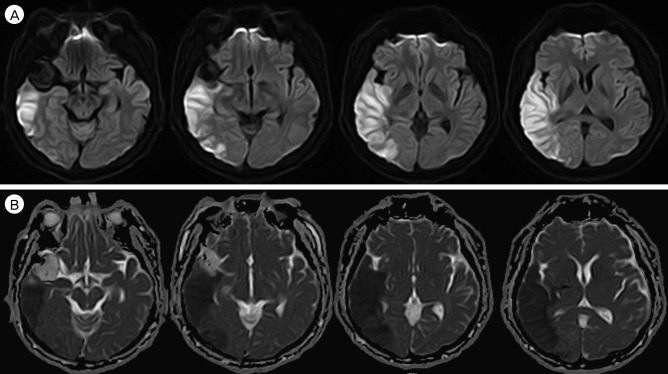
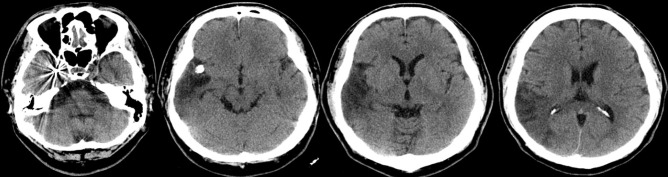
A 44-year-old male patient was admitted to our emergency department due to a seizure attack while he was undergoing brain magnetic resonance imaging (MRI) scan at a local hospital. He presented a history of a sudden onset of severe headache three weeks prior to his visit to our institution. Except the surgical history of cholecystectomy in 2014, he had neither a history of epilepsy nor medical diseases. He was an alert patient without neurologic deficit on his first arrival. The initial brain computed tomography (CT) scan demonstrated a 3.5 × 3.2 cm sized oval shape mass filled with a thrombus. A midline shift to the left of 3 mm and a slightly decreased size of right lateral ventricle were observed. The brain CT scan with contrast showed a mass-like lesion with a heterogeneous enhancement. It was identified to be a large tortuous vessel connected to an aneurysmal sac arising from the inferior trunk of right middle cerebral artery (MCA) according to the brain CT angiography (Fig. 1). The brain MRI revealed a mass of heterogenic signal intensity suggesting different stages of thrombus formation within the aneurysmal sac (Fig. 2). The patient consequently underwent a distracted subtraction angiography (DSA). We observed a contrast pooling in the inferior trunk of right MCA and a dilated outflow, which was drained to the distal MCA branches (Fig. 3).
Upon his hospital admission, he had no further seizure events, but, his symptoms of headache and dizziness remained the same consistently. Subsequently, a BOT was carried out to assess the patency of collateral cerebral circulation. After the proximal occlusion of the aneurysm by Sceptor C balloon (Microvention, Tustin CA, USA), the following parameters were intensively monitored for half an hour: the patient's somatosensory evoked potential (SSEP); cognitive and language function; and motor and sensory changes. The patient did not present any neurologic symptoms during the test (Fig. 4).
Based on the BOT results, an endovascular embolization was planned. 100 mg of aspirin and 75 mg of clopidogrel were given to the patient for seven days as a premedication method. On the day of coil embolization, a proximal artery occlusion by a dual catheter technique was planned. Firstly, we placed two catheters in the proximal artery of right MCA inferior trunk. Then, coiling was performed with two catheters in turn (Fig. 5). After coil embolization, the aneurysmal sac was completely occluded with its distal outflow. The patient was alert with no neurological symptoms immediately after the embolization. However, the next day after coiling, he was deteriorated to a drowsy mental status with dyscalculia. Diffusion weighted imaging of brain MRI was performed immediately in the acute setting of suspected stroke. A focal area of restricted diffusion involving right temporo-parietal lobe was observed (Fig. 6). The treatment protocol with mannitol and hypertonic saline was added while maintaining the oral medication with aspirin and clopidogrel. On the post-operative day 22, the patient's mental status improved and was noted as being alert even though he still exhibited mild Gerstmann syndrome. Two weeks after his hospital discharge, the follow-up brain CT scan showed a resolved mass effect and a decreased size of a low density lesion (Fig. 7).
Giant serpentine aneurysms are clinically uncommon, with an incidence of 0.1%.2) Most serpentine aneurysms are large with partially thrombosed lesions and are frequently located in the posterior circulation and in the middle cerebral artery.10) The symptomatic presentation is mostly due to a mass effect of its giant nature. Nevertheless, occasional ischemic symptoms are also caused by an unexpected embolic event in the distal branches of cerebral artery, the occlusions of collateral branches, and the flow impairments.10) Hemorrhagic complication is reported be rather rare. The characteristic neuro-imaging features of these aneurysms are as follows: a large size (> 25 mm); and a twisted vascular course within the aneurysm with multiple entrance and exit points. Giant serpentine aneurysms usually contain a ball of thrombus showing peripheral calcification and impose a mass effect with a midline shift. Additionally, cerebral edema in the vicinity of an aneurysmal mass is observed, mimicking a brain tumor in the CT scan. Aggressive surgical treatment is recommended for the giant serpentine aneurysms as a non-surgical management will eventually result in a continuous aneurysmal growth, neurological deterioration and poor outcomes.5)6)7) Total surgical excision, carotid ligation, entrapment, or aneurysm wrapping were traditionally recommended.1)3) These methods were primarily implemented in the field of revascularization operation of neurosurgery even though surgical morbidity and mortality rates of giant serpentine aneurysms were as high as 33%.1)4)8) Bypass surgery along with the excision of aneuysmal mass has been reported to be one of the successful treatment options for giant serpentine aneurysms. Immediate relief from the symptoms related to the mass effect was its strong advantage while the distal blood flow was patent at the same time. Nowadays, an endovascular treatment is another attractive option for the giant serpentine aneurysms with several reports of successful treatment. Giant serpentine aneurysms have been treated effectively by parent artery occlusion with detachable balloons and coils.
We hereby report a case of total occlusion of parent artery without neurologic deficit. If neurologic deficit is not developed during the BOT for approximately 30 minutes, a sufficient collateral circulation is assumed. In our case, neurologic deficit was not developed during the BOT. Based on this result, the coil embolization of parent middle cerebral artery was performed under SSEP monitoring. Unfortunately, our patient developed Gerstmann syndrome after the procedure. The possibility of insufficient BOT cannot be excluded.
Although a BOT was performed without any neurologic deficit, a post-operative infarction was developed after the endovascular treatment of giant serpentine aneurysm arising from middle cerebral artery. If a sufficient BOT was performed, a successful outcome without neurologic sequelae may be expected. Nonetheless, endovascular embolization of a parent artery can become one of the potential treatment options with more acceptable outcomes. Further clinical studies and multi-center data collection are required to address the issues of endovascular treatment of this specific disease.
Notes
References
1. Aletich VA, Debrun GM, Monsein LH, Nauta HJ, Spetzler RF. Giant serpentine aneurysms: a review and presentation of five cases. AJNR Am J Neuroradiol. 1995; 5. 16(5):1061–1072. PMID: 7639128.
2. Anson JA, Lawton MT, Spetzler RF. Characteristics and surgical treatment of dolichoectatic and fusiform aneurysms. J Neurosurg. 1996; 2. 84(2):185–193. PMID: 8592220.

3. Kumabe T, Kaneko U, Ishibashi T, Kaneko K, Uchigasaki S. Two cases of giant serpentine aneurysm. Neurosurgery. 1990; 6. 26(6):1027–1032. discussion 1032-3. PMID: 2362659.

4. Lee SJ, Ahn JS, Kwun BD, Kim CJ. Giant serpentine aneurysm of the middle cerebral artery. J Korean Neurosurg Soc. 2010; 8. 48(2):177–180. PMID: 20856671.

5. Mahadevan A, Tagore R, Siddappa NB, Santosh V, Yasha TC, Ranga U, et al. Giant serpentine aneurysm of vertebrobasilar artery mimicking dolichoectasia--an unusual complication of pediatric AIDS. Report of a case with review of the literature. Clin Neuropathol. 2008; Jan-Feb. 27(1):37–52. PMID: 18257473.
6. Park JS, Lee MS, Kim MS, Kim DJ, Park JW, Whang K. Giant serpentine intracranial aneurysm: a case report. Korean J Radiol. 2001; Jul-Sep. 2(3):179–182. PMID: 11752991.

7. Sari A, Kandemir S, Kuzeyli K, Dinc H. Giant serpentine aneurysm with acute spontaneous complete thrombosis. AJNR Am J Neuroradiol. 2006; 4. 27(4):766–768. PMID: 16611761.
8. Scott M, Skwarok E. The treatment of cerebral aneurysms by ligation of the common carotid artery. Surg Gynecol Obstet. 1961; 7. 113:54–61. PMID: 13749376.
9. Segal HD, McLaurin RL. Giant serpentine aneurysm. Report of two cases. J Neurosurg. 1977; 1. 46(1):115–120. PMID: 830809.
10. van Rooij WJ, Sluzewski M, Beute GN. Endovascular treatment of giant serpentine aneurysms. AJNR Am J Neuroradiol. 2008; 8. 29(7):1418–1419. PMID: 18388210.
Fig. 1
Computed tomography (CT) images. (A) Pre-contrast CT shows scattered high density along the right bifurcation level of middle cerebral artery (MCA) and surrounding oval shaped, about 3.5 × 3.2 cm in size. (B) Post-contrast images shows heterogeneous high attenuation with tadpole like contrast enhancement along the right side Sylvian fissure. (C) CT angiography shows a feeding artery with a dilatation of right inferior division of MCA and an oval-shaped contrast pooling mass with considerable dilated outflow drainage and a mass effect.
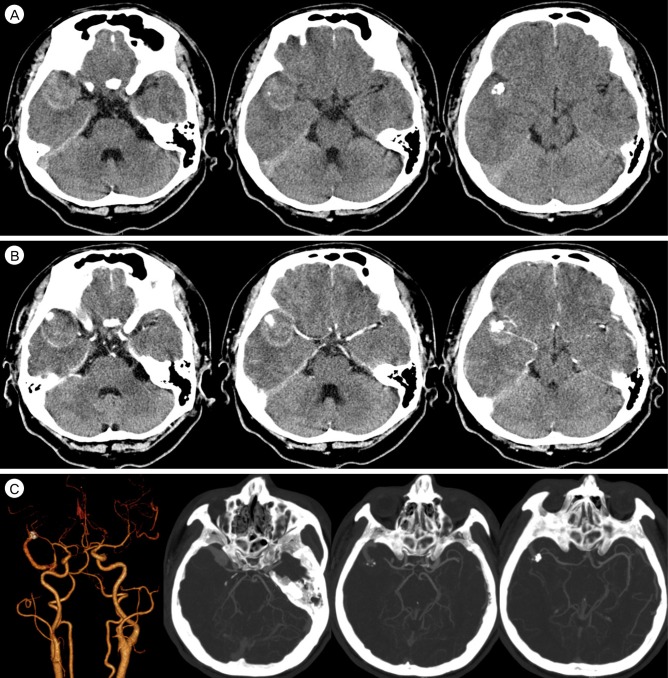
Fig. 2
Magnetic resonance imaging (MRI) images. (A) T1-weighted images (B) T2-weighted images. MRI shows a mass-like lesion with heterogenous signal intensity suggesting a formation of thrombus.
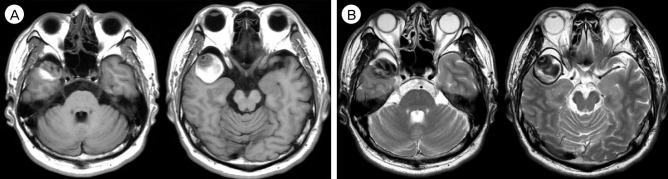
Fig. 3
Digital subtracted angiography (DSA) images. (A, B) Antero-posterior view (early, late), (C, D) Laterial views (early, late), (E) 3D-reconstructed images. DSA shows a giant aneurysm arising from the right middle cerebral artery (MCA) inferior trunk. The dilated outflow is seen as serpentine morphology which is continued to be drained to the distal MCA branches.
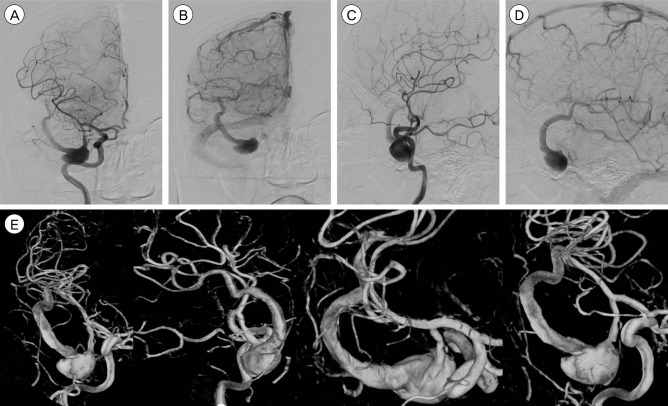
Fig. 4
BOT images. (A) Pre-test image, (B) Post-ballooning image. Balloon was located in the right MCA inferior trunk. After balloon inflation, an aneurysmal sac and its distal outflow was not seen. BOT = balloon occlusion test; MCA = middle cerebral artery.
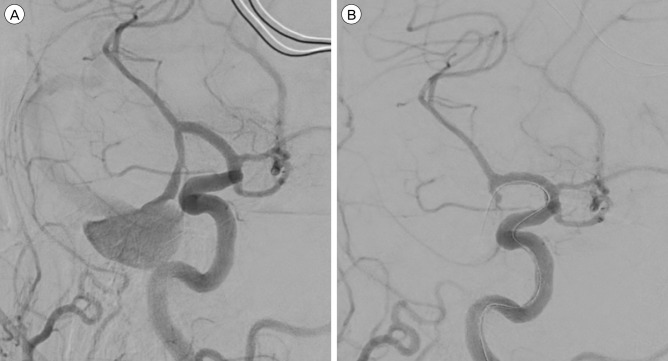
Fig. 5
Endovascular embolization. (A) Working view, (B) Double catheter technique. Catheter tip was placed in the proximal artery (black arrow), (C) Coil embolization, (D) Post-operative image, (E) Post-operative image of 3D reconstruction. Proximal artery was totally occluded by coiling (white arrow).




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download