Abstract
Radiation-induced vasculopathy is a rare occurrence, however, it is one of the most serious complications that can occur after gamma-knife radiosurgery (GKRS). The authors present two cases of incidentally found deep cerebral arteriovenous malformation (AVM), which were treated by GKRS, where subsequently there occurred delayed-onset cerebral infarction (11 and 17 months after GKRS) at an area adjacent to the AVM. In both cases, perforators of the M1 segment of the middle cerebral artery were included in the radiation field and delayed injury to these is suggested to be the mechanism of the ischemic event.
There is general consensus that radiosurgery is a preferred option to surgical removal for the treatment of an arteriovenous malformation in the basal ganglia, thalamus, and other deep brain areas. This is because surgical removal of a deep seated AVM is especially difficult, producing high mortality and morbidity rates.1)2)6)8) Consequently, gamma-knife radiosurgery (GKRS) has been employed for patients with a deep seated AVM. Although rare, radiation-induced vasculopathy is one of the most serious complications after GKRS.3)10) The basal ganglia and thalamus are extremely sensitive to radiation, therefore, GKRS for a deep seated AVM has increased risk of side effects during the latency period.9)14) Complication of large intracranial arteries related to GKRS has occasionally been reported.4)11) However, to the best of our knowledge, radiation induced ischemic injury to small arteries has never been reported. We report two cases of basal ganglia infarction after GKRS for deep seated AVM, which were located adjacent to the AVM. We suggested that radiation injury to the lenticulostriate artery could be one possible cause of the infarctions.
A 70-year-old male presented with an atypical headache for several months. There was no de finite history of underlying disease or medication such as hypertension and/or diabetes. Magnetic resonance imaging (MRI) and cerebral angiography showed a Spetzler-Martin grade 2 AVM, and the radiosurgery-based AVM score (RBAS) was 1.53, located in the right deep temporal lobe, adjacent to the basal ganglia (Fig 1A, B). There was no intra-nidal aneurysm. It was also drained to the basal vein of Rosenthal and straight sinus (Fig. 1C, D). GKRS was performed with a 9.6cc lesion volume and a 20 Gy marginal dose (Fig. 2). Gradual nidus regression was observed on serial follow-up brain MRI. One year later, a post-radiosurgical MRI follow-up showed nidus regression. Seventeen months after the radiosurgery procedure, the patient presented with acute-onset left hemiparesis (4/5) and sensory change. MRI showed an acute cerebral infarction at the right basal ganglia in the lenticulostriate artery territory, in an area adjacent to the GKRS (Fig. 3). The patient was administered 100 mg of aspirin from the stroke onset, and suffered no additional ischemic attack. Three months later, he recovered without prominent deficit (modified Rankin Scale, mRS = 0). It is interesting to note that complete obliteration of the AVM was confirmed at the 2-year follow-up angiography (Fig. 4A, B).
A 54-year-old male presented with an incidentally-detected AVM during his health examination. He had been diagnosed with hypertension and dosed angiotensin receptor blocker. MRI and cerebral angiography showed a Spetzler-Martin grade 3 AVM, and RBAS score was 1.78 in the right basal ganglia (Fig. 5A, B). It was mainly supplied by the Right M1 segment, and was drained into the internal cerebral vein (Fig. 5C, D). GKRS was performed with a 2.4 mL lesion volume and a 18 Gy marginal dose (Fig. 6). No immediate neurological deterioration was observed after GKRS. Eleven months after GKRS, the patient presented with sudden-onset left hemiparesis (2/5). Subsequent MRI showed an acute cerebral infarction in the right putamen, which probably originated by occlusion of the lateral lenticulostriate arteries (Fig. 7A, B). The patient received antiplatelet therapy of aspirin 100 mg and clopidogrel 75 mg. The patient suffered no additional stroke attack, he then recovered with slight disability (mRS = 2) at 3 months from onset. The patient underwent follow-up angiography 3 years after GKRS. Remarkably, the draining vein had decreased in diameter and most of the arteriovenous shunt including the nidus was no longer visible (Fig. 8A, B).
GKRS is an important therapeutic modality for a deeply located cerebral AVM.6)8) At the expense of a latency period to cure of 2-3 years, successful angiographic obliteration of AVMs is generally seen in approximately 70% of cases following radiosurgical treatment.3)5)
Although GKRS is a widely accepted treatment modality, progressive intracranial artery occlusion due to radiation induced vasculopathy is a serious side effect of conventional radiation therapy for intracranial disease. As the follow-up lengthens in modern series, details of radiation-induced injury have become more clearly elucidated. Because the basal ganglia and thalamus are extremely sensitive to radiation side effects and hemorrhage during the latency period, deep AVMs have increased risks associated with radiosurgical therapy.9)12) In addition, one autopsy study reported that a normal surrounding blood vessel may also be affected by irradiation of 10 Gy or more, and remarkable intimal hypertrophy with fragmentation of the elastic laminae, or even complete occlusion, can occur in these arteries.13)
Vascular complication associated with GKRS for deep AVM has been noted in several case reports, including de novo aneurysm formation, venous varix formation or stenosis of major intracranial arteries. There have been occasional reports of stenosis or occlusion of major cerebral arteries occurring several years after stereotactic radiosurgery for cerebral arteriovenous malformations.4)7)11) Exposure of a major cerebral vessel to radiation doses of 15 to 25 Gy can potentially result in postradiosurgical stenosis or occlusion, although the incidence occurs in fewer than 1% of patients.11)
Some literature studies have reported that steno-occlusive complication could occur even at larger intracranial arteries after GKRS, in spite of low-dose radiation exposure.7)12) However, in the current study, in both cases the ischemic injury involved small perforating arteries (lateral lenticulostriate arteries), and those events occurred at 11 and 17 months after the GKRS.
A limitation to this case report is that there might be some debate about the etiology, because we present only 2 case reports and both patients had other risk factors for acute stroke. The patient in case 1 was old (70-year-old), and the patient in case 2 had underlying hypertension. Therefore, an alternative explanation of the underlying cause in each case may be a small vessel occlusion due to atherosclerosis. In addition, evidence of radiation induced vasculopathy has not been confirmed in our two cases. In this regard, future prospective studies and long-term follow-up are necessary to prove the relationship between delayed perilesional ischemic injury and GKRS for deep seated AVMs.
The authors present two cases of delayed perilesional ischemic events after GKRS for a deep seated AVM, which occurred at 11 and 17 months after the treatment and may have been caused by radiation injury to the lateral lenticulostriate arteries. Although alternative causes of the ischemic events are possible, awareness of the possibility of radiation-induced vasculopathy of small arteries will be helpful in establishing early and accurate diagnoses along with the appropriate therapy. Larger studies with longer, formal angiographic follow-up will be necessary to clarify these events and their clinical significance.
References
1. Betti OO, Munari C, Rosler R. Stereotactic radiosurgery with the linear accelerator: treatment of arteriovenous malformations. Neurosurgery. 1989; 3. 24(3):311–321. PMID: 2648180.

2. Chiou TS, Tsai CH, Lee YH. Unilateral Holmes tremor and focal dystonia after Gamma Knife surgery. J Neurosurg. 2006; 12. 105(Suppl):235–237. PMID: 18503362.

3. Gross BA, Ropper AE, Du R. Vascular complications of stereotactic radiosurgery for arteriovenous malformations. Clin Neurol Neurosurg. 2013; 6. 115(6):713–717. PMID: 22910397.

4. Lim YJ, Leem W, Park JT, Kim TS, Rhee BA, Kim GK. Cerebral infarction with ICA occlusion after Gamma Knife radiosurgery for pituitary adenoma: A case report. Stereotact Funct Neurosurg. 1999; 72(Suppl 1):132–139. PMID: 10681701.

5. Loeffler JS, Rossitch E Jr, Siddon R, Moore MR, Rockoff MA, Alexander E 3rd. Role of stereotactic radiosurgery with a linear accelerator in treatment of intracranial arteriovenous malformations and tumors in children. Pediatrics. 1990; 5. 85(5):774–782. PMID: 2184409.

6. Lunsford LD, Kondziolka D, Flickinger JC, Bissonette DJ, Jungreis CA, Maitz AH, et al. Stereotactic radiosurgery for arteriovenous malformations of the brain. J Neurosurg. 1991; 10. 75(4):512–524. PMID: 1885968.

7. Marks MP, Delapaz RL, Fabrikant JI, Frankel KA, Phillips MH, Levy RP, et al. Intracranial vascular malformations: imaging of charged-particle radiosurgery. Part II. Complications. Radiology. 1988; 8. 168(2):457–462. PMID: 3293113.

8. Pollock BE, Gorman DA, Brown PD. Radiosurgery for arteriovenous malformations of the basal ganglia, thalamus, and brainstem. J Neurosurg. 2004; 2. 100(2):210–214. PMID: 15086226.

9. Potts MB, Young WL, Lawton MT. UCSF Brain AVM Study Project. Deep arteriovenous malformations in the Basal Ganglia, thalamus, and insula: microsurgical management, techniques, and results. Neurosurgery. 2013; 9. 73(3):417–429. PMID: 23728451.
10. Uozumi Y, Sumitomo M, Maruwaka M, Araki Y, Izumi T, Miyachi S, et al. Moyamoya syndrome associated with gamma knife surgery for cerebral arteriovenous malformation: case report. Neurol Med Chir (Tokyo). 2012; 52(5):343–345. PMID: 22688073.
11. Yamamoto M, Ide M, Jimbo M, Ono Y. Middle cerebral artery stenosis caused by relatively low-dose irradiation with stereotactic radiosurgery for cerebral arteriovenous malformations: case report. Neurosurgery. 1997; 8. 41(2):474–477. PMID: 9257317.

12. Yamamoto M, Jimbo M, Hara M, Saito I, Mori K. Gamma knife radiosurgery for arteriovenous malformations: long-term follow-up results focusing on complications occurring more than 5 years after irradiation. Neurosurgery. 1996; 5. 38(5):906–914. PMID: 8727815.

13. Yamamoto M, Jimbo M, Ide M, Kobayashi M, Toyoda C, Lindquist C, et al. Gamma knife radiosurgery for cerebral arteriovenous malformations: an autopsy report focusing on irradiation-induced changes observed in nidus-unrelated arteries. Surg Neurol. 1995; 11. 44(5):421–427. PMID: 8629225.

14. Yen CP, Khaled MA, Schwyzer L, Vorsic M, Dumont AS, Steiner L. Early draining vein occlusion after gamma knife surgery for arteriovenous malformations. Neurosurgery. 2010; 11. 67(5):1293–1302. PMID: 20871437.

Fig. 1
Magnetic resonance imaging and cerebral angiography shows a Spetzler-Martin grade 2 arteriovenous malformation (AVM) located in the right deep temporal lobe, adjacent to the basal ganglia (A and B). This AVM is supplied by a perforator of A1 segment and M1 segment, drained by the basal vein of Rosenthal (C and D).
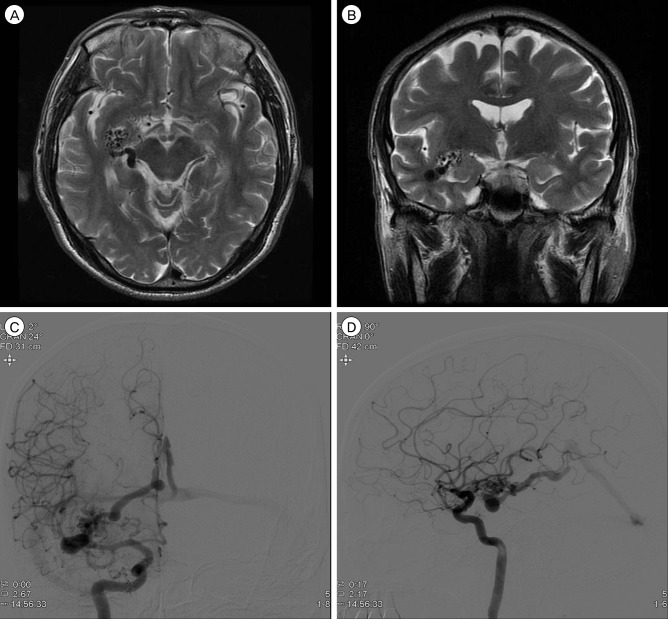
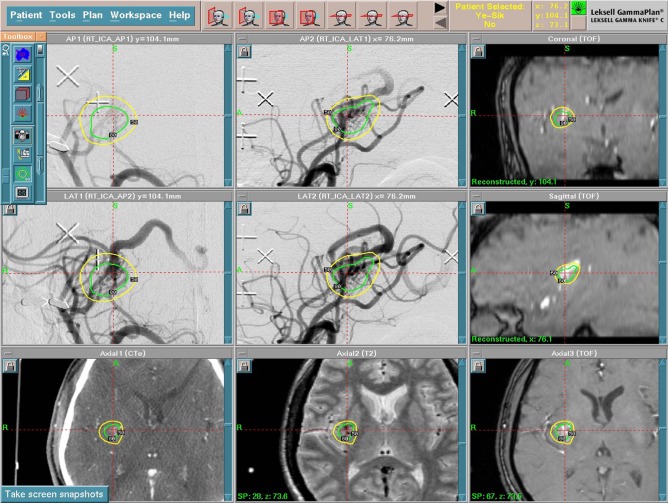
Fig. 2
Gamma-knife radiosurgery was performed with a 9.6 mL lesion volume and a 20 Gy marginal dose.
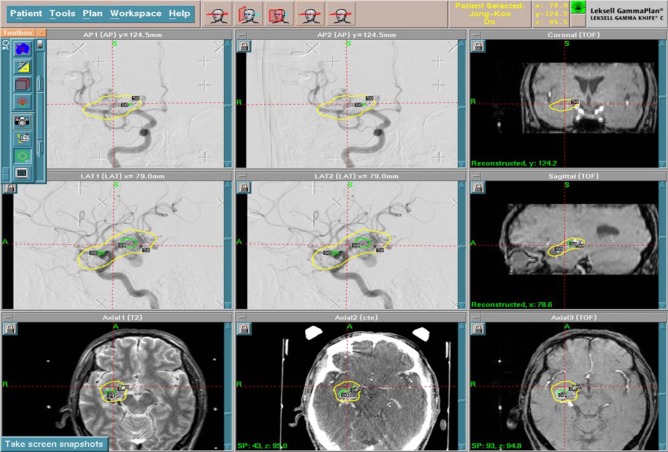
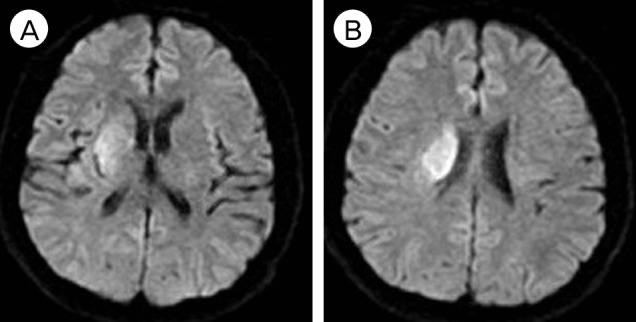
Fig. 3
Seventeen months after gamma-knife radiosurgery. magnetic resonance imaging showed acute cerebral infarction at the right basal ganglia.
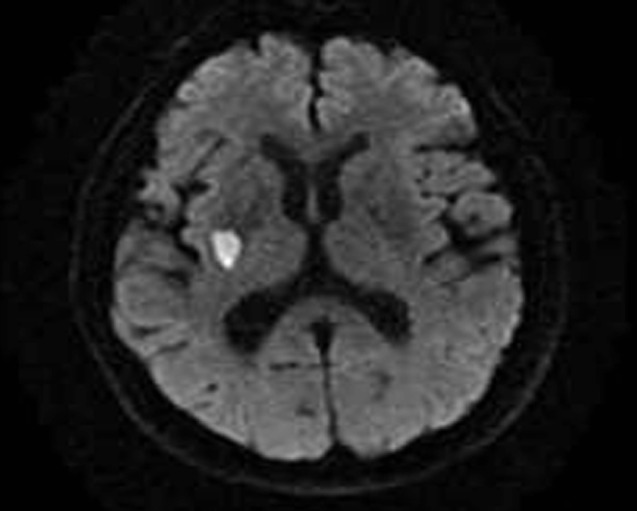
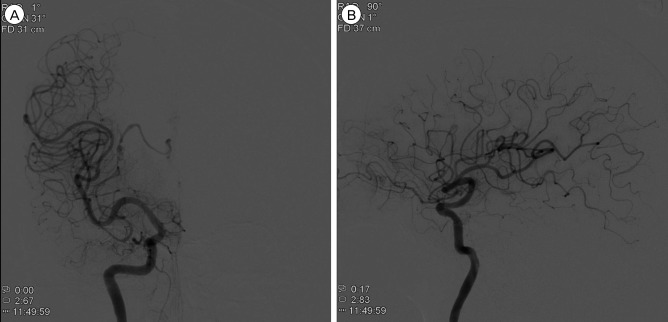
Fig. 4
At 2 years after gamma-knife radiosurgery, follow-up angiography showed complete obliteration of the arteriovenous malformation (A and B).
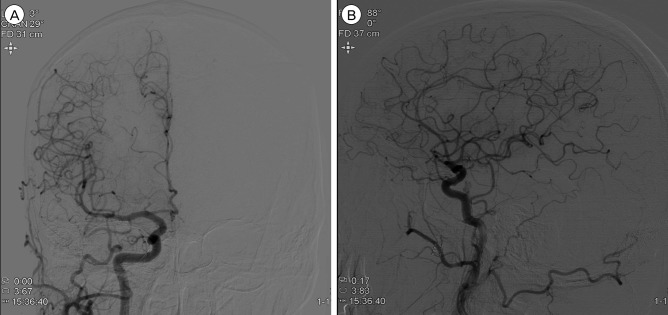
Fig. 5
Baseline magnetic resonance imaging showed an arteriovenous malformation (AVM) at the right Basal ganglia (A and B). This AVM is supplied by middle cerebral artery M1 segment, drained by an internal cerebral vein (C and D).
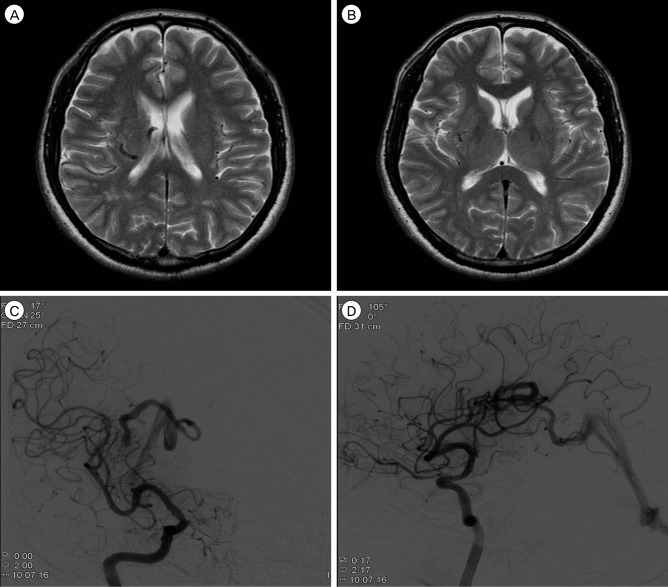
Fig. 6
Gamma-knife radiosurgery was performed with a 2.4 mL lesion volume and an 18 Gy marginal dose.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download