Abstract
Objectives
The 5MAX ACE is a new large bore aspiration catheter available for vessel recanalization for treatment of acute ischemic stroke (AIS). We report our initial experience with its use.
Methods
A retrospective analysis of patients undergoing intra-arterial therapy for AIS using the 5MAX ACE reperfusion catheter at our institution was performed. Patient demographics, clinical characteristics and procedural data were obtained from chart review. Successful recanlization was defined as achievement of Thrombolysis in Cerebral Infarction score (TICI) 2b-3 and time to recanalization was defined as time from groin puncture to achievement of at least TICI 2b recanalization.
Results
The 5MAX ACE was used in 15 patients from July-October 2013. Direct aspiration was used as the primary technique in 10/15 (67%) patients. Out of these, aspiration alone was sufficient for recanalization in 3 (20%) patients. In the remaining 7 (47%) patients, additional devices were used. In 5/15 (33%) patients, combined aspiration/stentriever thrombectomy using Solitaire™ (3/5 patients) and Penumbra 3D Separator™ (2/5 patients) were used as the primary technique. Successful recanlization (TICI 2b-3) was achieved in 11/15 (73%) patients. Average time from groin puncture to successful recanalization was 46 +/- 30 minutes (range 14-98 minutes). There were no procedural complications.
Conclusion
The 5MAX ACE is a useful recanalization tool, either by direct aspiration or combined stentriever/aspiration. It may be most advantageous with large clots in the internal carotid artery. The potential for effective and faster recanalization using this device alone or in combination may be a good topic for future study.
Intra-arterial therapy (IAT) is a treatment option in patients with severe acute ischemic stroke (AIS) from arterial occlusion who do not respond to intravenous tissue plasminogen activator (tPA) or in whom tPA is contraindicated. Efficient and timely recanalization of the occluded vessel is an extremely important goal in IAT. With continuing advancements in the development of endovascular devices and techniques, more options are now available for management of AIS. Using newer thrombectomy devices, better recanalization rates can be achieved in much shorter times compared to older devices.5)6) The 5MAX ACE reperfusion catheter (Penumbra, Inc., Alameda, CA, USA), a new large bore aspiration catheter available for vessel recanalization, was launched in July 2013. We report on our initial experience with the use of this catheter.
This was a retrospective case series analysis study of patients undergoing IAT for AIS using the 5MAX ACE reperfusion catheter. The neuroendovascular procedure log of our institution was searched in order to identify all patients in whom the catheter was used since the time it became available. Patient demographics, clinical characteristics, and procedural data were obtained from chart review. Successful recanalization was defined as achievement of TICI score 2b-3. Time to recanalization was defined as time from groin puncture to achievement of at least TICI score 2b recanalization.
The 5MAX ACE reperfusion catheter can be used in several ways in the endovascular treatment of AIS. Direct aspiration involves placement of a large bore aspiration catheter at the face of the clot and aspirating until the device becomes occlusive.4) This technique has become increasingly feasible with modern, ultra-flexible intermediate lumen catheters, leading some centers to use the approach as a first line endovascular technique for IAT in AIS.8) Other techniques include catheter with mechanical disruption using the Penumbra Separator (Penumbra, Inc., Alameda, California, USA) or in conjunction with a stent-retriever, such as the Trevo® (Stryker, Kalamazoo, MI, USA) or Solitaire™ (Covidien, Plymouth, MN, USA) providing aspiration at the clot during device retrieval.2) There is no universal protocol for method of mechanical thrombectomy and the technique is operator dependent. In most cases of large vessel occlusion, direct aspiration technique is used as the primary method for mechanical thrombectomy. For MCA occlusions, some operators use stent-trievers in combination with direct aspiration as the primary technique. Two patients in our cohort were part of a clinical trial wherein in the Separator 3D device was used.
Patients who underwent IAT were selected per the AIS therapy protocols instituted in our hospital. Cerebral vessel access was established using a guide sheath; either a 6F Neuron™ Max 088 (Penumbra, Inc., Alameda, CA, USA) or a 6F/7F Shuttle (Cook, Inc., Bloomington, IN, USA). For extra support, the guide sheath was advanced as distal as possible in the internal carotid artery (ICA) for anterior circulation strokes, usually at the skull base or the petrous segment. For the two patients with basilar artery thrombus, the guide sheath was advanced up to the distal V2 segment.
The following technique was used for most patients: under road map assistance, the 5MAX ACE was advanced to the face of the clot over a microcatheter (3MAX reperfusion catheter [Penumbra, Inc., Alameda, CA, USA]) and a 0.016 inch microwire (Fathom [Boston Scientific Corp., Naidich, MA, USA]). The wire and the microcatheter were advanced very gently across the clot into a bifurcation branch of the middle cerebral artery (MCA) followed by advancement of the 5MAX ACE. Once the 5MAX ACE was immediately adjacent to the clot, the microcatheter and microwire were removed. Manual suction was applied to the 5MAX ACE using a 0.6 dL syringe. Once a good seal was obtained, the 5MAX ACE catheter was slowly pulled out, maintaining the aspiration. During removal, simultaneous suction to the side port of the guide sheath was applied using a 0.6 dL syringe. Once the 5MAX ACE was removed from the body, the guide sheath was opened to allow back bleeding of possible clots, and then flushed forward once it was confirmed that there were no more clots (Fig. 1). This process using the tri-axial unit was repeated if necessary. Additional devices including stent-retriever, separator with aspiration or direct aspiration through smaller sized catheters (4MAX or 3MAX reperfusion Penumbra catheters) were used for persistent clots or embolization into smaller caliber arteries (Figs. 2 and 3).
The second technique involving the use of 5MAX ACE was combined aspiration/stentriever thrombectomy using Solitaire™ (ev3/Covidien, Plymouth, MN, USA). After establishing cerebral vascular access as described above, a microcatheter for Solitaire delivery was placed within the 5MAX ACE and advanced to the site of occlusion under road map assistance. The 5MAX ACE was advanced as distally as safely possible. The microwire and microcatheter were advanced through and beyond the thrombus. The microwire was then removed and the stent was deployed over the site of the thrombus. Once satisfactorily deployed, the microcatheter was removed. After 5 minutes, aspiration/stent thrombectomy was performed by pulling the stent into the distal access catheter while applying simultaneous aspiration to the 5MAX ACE using a 0.6 dL syringe. Additional thrombectomy attempts were performed as needed (Fig. 4).
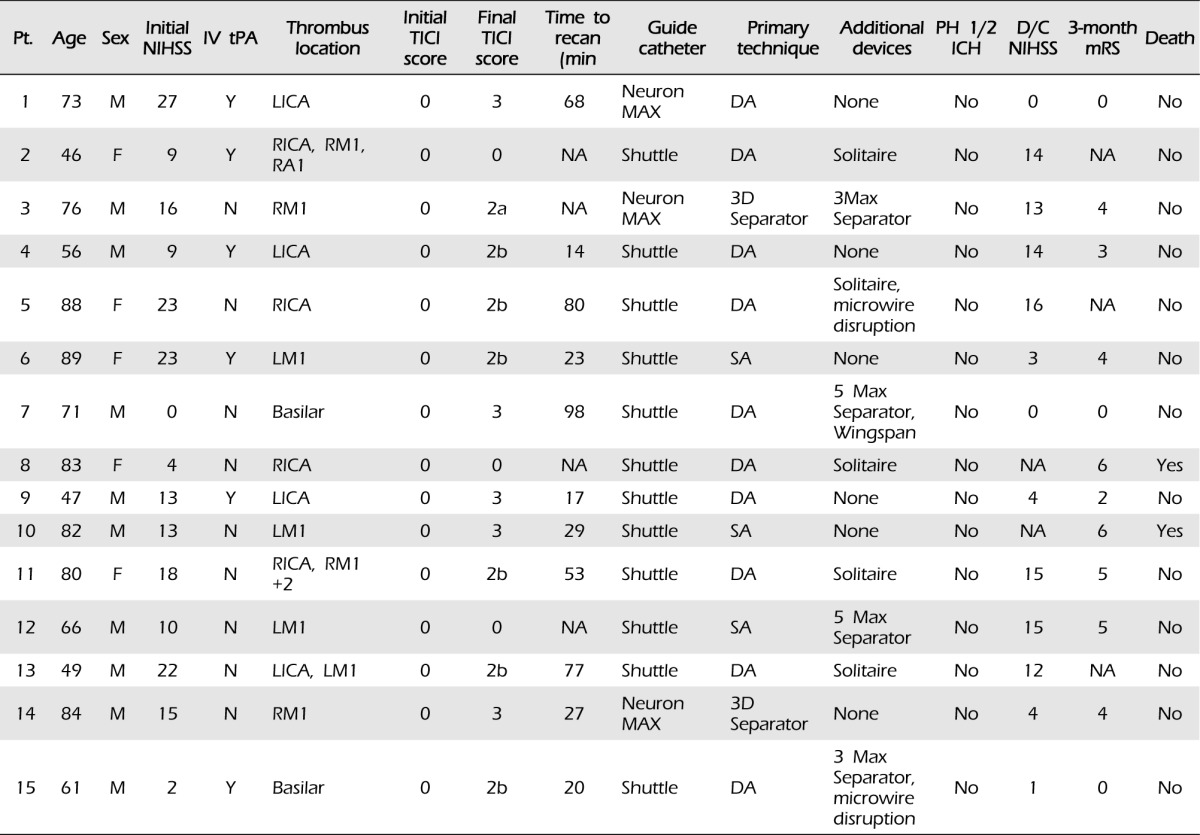
Fifteen patients who underwent IAT for AIS from July to October 2013, in whom the 5MAX ACE reperfusion catheter was used as described above, were included in the study. The characteristics of the patients are shown in Table 1. The cohort included 10 males (67%), with a median age of 73 years (range 46-89). The median National Institutes of Health Stroke Scale (NIHSS) score at admission was 13 (range 0-27). Six (40%) patients received intravenous tPA prior to undergoing IAT. Thirteen (87%) patients had vessel occlusion in the anterior circulation (ICA 8 [53%], M1 5 [33%]), and 2 (13%) had basilar artery thrombus. Direct aspiration through the 5MAX ACE was used as the first thrombectomy technique in 10/15 (67%) patients. Out of these 10 patients, direct aspiration alone was sufficient for recanalization in 3 (20%) patients. In the remaining 7 (47%) patients, additional devices were used for recanalization (Solitaire in 5 patients and Penumbra separator in 2 patients). One patient with a basilar artery thrombus also had severe atherosclerotic stenotic disease that was stented with a Wingspan™ stent (Stryker, Kalamazoo, MI, USA). In 5/15 (33%) patients, combined aspiration/stentriever thrombectomy was performed using Solitaire (3/5 patients) and Penumbra 3D separator (2/5 patients) as the primary thrombectomy techniques. Successful recanalization (TICI score 2b-3) was achieved in 11/15 (73%) patients. TICI score 3 recanalization was achieved in 5 (33%) patients. Average time from groin puncture to successful recanalization was 46 +/- 30 minutes (range 14-98 minutes). There were no procedural complications in any of the patients who underwent IAT. There were no parenchymal hematomas (PH1 and PH2) as defined by European Cooperative Acute Stroke Study definitions in any patients post procedure. Two (13%) patients passed away during hospitalization. From a stroke standpoint (NIHSS), both of these patients showed significant improvement post procedure, but passed away later from complications of premorbid medical illnesses, and subsequent withdrawal of care in one case. Of the remaining 13 patients, 10 (77%) showed an improvement in NIHSS at the time of discharge. Modified rankin scale (mRS) score at 3-month follow-up was available for 12 patients. Four (33%) patients achieved good outcome of mRS 0-2.
The 5MAX ACE reperfusion catheter, a new flexible large bore aspiration catheter from Penumbra, increases aspiration force at the catheter tip, and can be used for direct aspiration, aspiration with clot maceration, or with stent-retrievers and analogues for clot in-situ aspiration during device retrieval. The direct aspiration technique and the combined use of stent retriever and direct aspiration for thrombectomy represent substantial improvements in endovascular technique for treatment of AIS and the 5MAX ACE facilitates the use of these techniques enabling effective recanalization in significantly shorter periods of time.4)8) With regard to clinical outcomes, a high percentage of patients (77%) showed improvement in NIHSS at discharge. Two patients with unsuccessful recanalization expectedly showed worsening of NIHSS, and in the last patient who had worsening NIHSS, recanalization was achieved along with improvement in examination post procedure, but worsening developed later due to additional infarcts. Despite improvements in NIHSS, only 33% of patients with follow-up achieved good outcome of 0-2 as measured by the mRS. Patients in our small cohort were older with multiple medical co-morbidities, which might explain the outcomes. This should be further examined in larger studies using the device.
TICI score 2b-3 recanalization was achieved in 73% of patients. In analysis by the involved vessel, successful recanalization was achieved in 75% of ICA, 60% of M1, and 100% of basilar artery occlusion. We felt that the direct aspiration technique was particularly effective in patients with an extensive clot burden in the ICA extending to the MCA. Direct aspiration alone resulted in successful extraction of clot in three patients with ICA thrombus. In cases where additional devices were used, direct aspiration resulted in successful recanalization of the ICA, proximal M1 and basilar artery but subsequent Solitaire, Penumbra separator device or microwire thrombus disruption was used for distal M1, M2, and M3 segments of MCA and P2 segment of posterior cerebral artery recanalization. In cases where direct aspiration failed as the primary thrombectomy method, use of additional devices also did not result in successful recanalization of the vessel. Combined stent retriever/aspiration with Solitaire or Penumbra Separator 3D as the first thrombectomy method was used only in patients with M1 thrombus. Distal embolization in the territory of the affected vessel was seen more commonly with the later methods using Solitaire or Penumbra separator. Distal aspiration attributable to direct aspiration occurred in three patients. This likely occurred when crossing the clot with the microwire and microcatheter and as such this step should be performed with extreme care.
Compared to previously reported thrombectomy experiences, recanalization using the 5MAX ACE was achieved at significantly faster rates, at a mean of 46 minutes and as early as 14 minutes. Despite its size, the 5MAX ACE was easy to navigate and showed superior trackability. The Penumbra aspiration catheters have undergone multiple iterations, and the newer generation catheters have superior trackability, especially at the tip. Compared to its predecessors, this allows for easy navigation over obdurating the microcatheter across the ophthalmic bend, and the authors have not experienced significant trouble with navigation. The 5MAX ACE has an inner lumen diameter of 0.068" proximally and a tapered distal lumen with a diameter of 0.060". This is in comparison to its predecessor, the 5MAX, which has a proximal and distal inner lumen diameter of 0.064" and 0.054", respectively. The design specification of the catheter implies increased suction transmission to the catheter tip, as flow impedance varies by the reciprocal of the luminal radius cubed. Given the large inner lumen, large pieces of clot could be extracted, and often times the clot was extracted in toto. The lumen can fit the 5MAX ACE or 3MAX separator and the Separator 3D in cases where the vessel cannot be recanalized by direct aspiration.
Although head to head comparisons are inaccurate, recanalization rates using the 5MAX ACE, using either direct aspiration or as an adjunct to other devices, were comparable to the rates observed in TREVO 25) or the Penumbra Pivotal Stroke trial, and7) or superior to those observed in the SWIFT trial.6) Recently, a multi-center case series on the use of the 5MAX, 3MAX, and Neuron Max reperfusion catheters using direct aspiration as the primary thrombectomy method in 37 patients reported 100% successful recanalization at an even faster rate (mean 28.1 minutes) compared to our current series.4) This series described patients in whom only direct aspiration was used. In addition, an important factor to note is the location of thrombus that included ICA in 19% of patients and MCA in 62% of patients. The MCA occlusions also included some M2 and M3 segment thrombi. Despite the limitation of small numbers in our series, it contained significantly more ICA occlusions (53%) and only included M1 segment thrombus. Rates of basilar artery thrombus were comparable between the two series - although one of our cases included underlying stenosis. The difference in rates and times of recanalization is likely related to a number of factors, but may importantly be related to greater difficulty in recanalizing ICA and M1 occlusions due to larger thrombus burden. Even so, the rates of ICA (75%) and M1 (60%) recanalization were significantly higher than the rates achieved in the Interventional Management of Stroke III trial, which recorded 38% and 44%, respectively.1) The result observed in our small sample using the 5 MAX ACE is comparable to that reported in the SPEED study using the Penumbra 054 Reperfusion Catheter System. The 5 MAX ACE, with a distal lumen diameter of 0.060", is 0.006" more than the 054 system, which translates to a gain in cross sectional area of approximately 23%.3)
We feel that the greatest advantage of the 5MAX ACE is its use in recanalizing ICA occlusions from large thrombus using direct aspiration. When compared to the disadvantages of the stent retriever technique including proximal/distal embolization, stent fracture, and poor navigability, the simple technique of direct aspiration combined with the large inner lumen and easy navigability of the 5MAX ACE makes this an attractive first option for use in IAT. Direct aspiration as a first line maneuver confers lower cost of materials, and may actually be faster, as no clot intercalation time is necessary. If the large bore aspiration catheter can be safely advanced to M1 segments and the like, it does not take much time to attempt direct aspiration, which can be quickly followed by stent-retrieval as the operator deems necessary. However, the clinical benefits beyond the intra-procedural savings of reduced number of devices can only be determined by a head to head trial comparing a number of permutations of single and combined techniques and device combinations.
This study has multiple limitations, particularly the small sample size and the retrospective nature of the study. A further limitation is the heterogeneity of the clinical scenarios, including sub-acute strokes, underlying atherosclerotic lesions and tandem lesions. Angiographic recanalization rates and time to recanalization were both derived by self-adjudicated results. Beyond recanalization end points, we have incomplete clinical end points due to the short follow-up period.
The 5MAX ACE is a useful tool in the armamentarium of neurointerventionlists for treatment of AIS, either by direct aspiration or combined stent retriever/aspiration. Our review of our initial experience suggests that there were no procedural complications directly attributable to the device in our series. Its use as a standalone technique seems feasible, and it may be advantageous with large clots in the ICA. The potential for effective and faster recanalization using this device alone or in combination may be a good topic for future study.
References
1. Broderick JP, Palesch YY, Demchuk AM, Yeatts SD, Khatri P, Hill MD, et al. Interventional Management of Stroke (IMS) III Investigators. Endovascular therapy after intravenous t-PA versus t-PA alone for stroke. N Engl J Med. 2013; 3. 368(10):893–903. PMID: 23390923.
2. Dumont TM, Mokin M, Sorkin GC, Levy EI, Siddiqui AH. Aspiration thrombectomy in concert with stent thrombectomy. J Neurointerv Surg. 2014; 5. 6(4):e26. PMID: 23868216.

3. Frei D, Gerber J, Turk A, McPherson M, Heck D, Hui F, et al. The SPEED study: initial clinical evaluation of the Penumbra novel 054 Reperfusion Catheter. J Neurointerv Surg. 2013; 5. 5(Suppl 1):i74–i76. PMID: 23299104.

4. Kang DH, Hwang YH, Kim YS, Park J, Kwon O, Jung C. Direct Thrombus Retrieval Using the Reperfusion Catheter of the Penumbra System: Forced-Suction Thrombectomy in Acute Ischemic Stroke. AJNR Am J Neuroradiol. 2011; 2. 32(2):283–287. PMID: 21087940.

5. Nogueira RG, Lutsep HL, Gupta R, Jovin TG, Albers GW, Walker GA, et al. Trevo versus Merci retrievers for thrombectomy revascularisation of large vessel occlusions in acute ischaemic stroke (TREVO 2): a randomised trial. Lancet. 2012; 10. 380(9849):1231–1240. PMID: 22932714.

6. Saver JL, Jahan R, Levy EI, Jovin TG, Baxter B, Nogueira RG, et al. Solitaire flow restoration device versus the Merci retriever in patients with acute ischaemic stroke (SWIFT): a randomised, parallel-group, non-inferiority trial. Lancet. 2012; 10. 380(9849):1241–1249. PMID: 22932715.

7. Penumbra Pivotal Stroke Trial Investigators. The penumbra pivotal stroke trial: Safety and effectiveness of a new generation of mechanical devices for clot removal in intracranial large vessel occlusive disease. Stroke. 2009; 8. 40(8):2761–2768. PMID: 19590057.
8. Turk AS, Spiotta A, Frei D, Mocco J, Baxter B, Fiorella D, et al. Initial clinical experience with the ADAPT technique: A direct aspiration first pass technique for stroke thrombectomy. J Neurointerv Surg. 2014; 4. 6(3):231–237. PMID: 23624315.

Fig. 1
Diagram showing the direct aspiration technique. First (A), the microwire is advanced past the clot and the microcatheter is advanced to the face of the clot. The 5MAX ACE is then advanced over the microcatheter to the face of the clot (B). The microwire and microcatheter are then removed (C), and suction is applied to the 5MAX ACE (D).
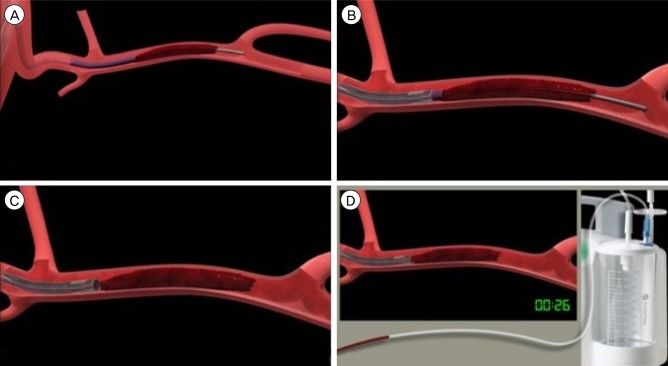
Fig. 2
Patient No 1. Left internal carotid artery (LICA) thrombus with thrombolysis in cerebral infarction (TICI) score 0 flow. After the first attempt with direct aspiration, flow was restored in the LICA. Post intervention angiogram shows TICI score 3 recanalization.
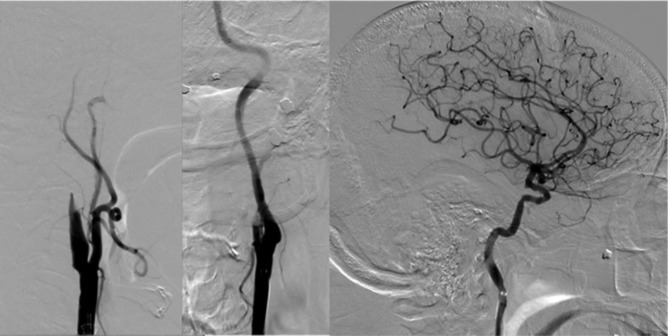
Fig. 3
Patient No. 15. Basilar apex is occluded with absence of opacification of bilateral posterior cerebral arteries. First two attempts at direct aspiration were unsuccessful. After the third attempt at direct aspiration, the basilar occlusion was recanalized with establishment of thrombolysis in cerebral infarction score 2b flow.
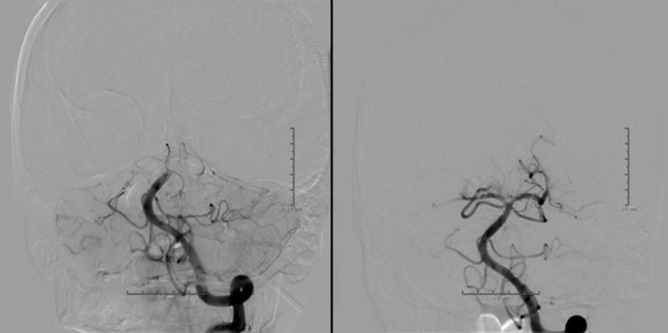
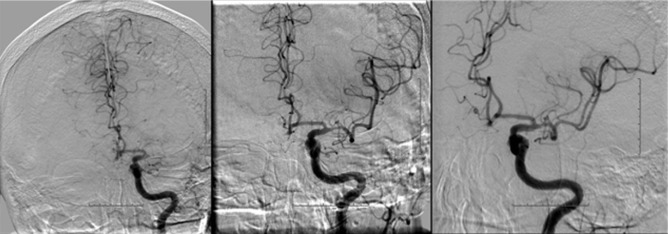
Fig. 4
Patient No 6. Left middle cerebral artery is occluded in the proximal segment with thrombolysis in cerebral infarction (TICI) score 0 flow. After the first attempt at combined stent retriever thrombectomy and aspiration, the LM1 was recanalized, with TICI score 2b flow subsequently established.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download