Abstract
Objectives
Metabolic syndrome components, insulin resistance and central obesity cause type 2 diabetes and hypertension. This will increase the risk of cardiovascular disease. Women after menopause are at increased risk of metabolic syndrome. Several researchers studied that in menopause, metabolic syndrome increased cardiovascular mortality. We studied the impact on cardiovascular mortality of postmenopausal women with metabolic syndrome in the Republic of Korea.
Methods
Twenty four thousand nine hundred forty nine postmenopausal women aged 40 years or older were enrolled at health promotion centers of national university hospital located in 18 regions during 1994-2004. Age, weights, height, body mass index (BMI), systolic blood pressure (SBP), diastolic blood pressure (DBP), fasting blood glucose (FBG), cholesterol, triglyceride (TG), high-density lipoprotein were evaluated and history taking about alcohol consumption, smoking, and exercise was performed. In addition, subjects who died of cardiac disease were analyzed from January 1995 to December 2009.
Results
Metabolic syndrome was higher in postmenopausal women with increased in age, BMI, blood pressure (BP), FBG, cholesterol, TG. Thirty cardiac deaths occurred during the observation period. Factors affecting cardiac death were age, smoking, FBG and when age and smoking were controlled. FBG was an important factor affecting cardiovascular mortality in our study. When controlling age, smoking, and alcohol consumption, metabolic syndrome caused an increased relative risk of cardiovascular mortality. Survival rate was much lower in postmenopausal women with metabolic syndrome than those without metabolic syndrome.
Figures and Tables
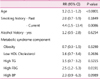
Fig. 1
Kaplan-Meier curves are illustrated for the subjects with metabolic syndrome and without metabolic syndrome in postmenopausal women. Metabolic syndrome poses a significant increase in cardiovascular mortality risk in postmenopausal women.
References
1. Levesque J, Lamarche B. The metabolic syndrome: definitions, prevalence and management. J Nutrigenet Nutrigenomics. 2008. 1:100–108.
2. Park YW, Zhu S, Palaniappan L, Heshka S, Carnethon MR, Heymsfield SB. The metabolic syndrome: prevalence and associated risk factor findings in the US population from the Third National Health and Nutrition Examination Survey, 1988-1994. Arch Intern Med. 2003. 163:427–436.
3. Mottillo S, Filion KB, Genest J, Joseph L, Pilote L, Poirier P, et al. The metabolic syndrome and cardiovascular risk a systematic review and meta-analysis. J Am Coll Cardiol. 2010. 56:1113–1132.
4. Hu G, Qiao Q, Tuomilehto J, Balkau B, Borch-Johnsen K, Pyorala K. Prevalence of the metabolic syndrome and its relation to all-cause and cardiovascular mortality in nondiabetic European men and women. Arch Intern Med. 2004. 164:1066–1076.
5. Lin JW, Caffrey JL, Chang MH, Lin YS. Sex, menopause, metabolic syndrome, and all-cause and cause-specific mortality--cohort analysis from the Third National Health and Nutrition Examination Survey. J Clin Endocrinol Metab. 2010. 95:4258–4267.
6. Wing RR, Matthews KA, Kuller LH, Meilahn EN, Plantinga PL. Weight gain at the time of menopause. Arch Intern Med. 1991. 151:97–102.
7. Torng PL, Su TC, Sung FC, Chien KL, Huang SC, Chow SN, et al. Effects of menopause and obesity on lipid profiles in middle-aged Taiwanese women: the Chin-Shan Community Cardiovascular Cohort Study. Atherosclerosis. 2000. 153:413–421.
8. Akahoshi M, Soda M, Nakashima E, Shimaoka K, Seto S, Yano K. Effects of menopause on trends of serum cholesterol, blood pressure, and body mass index. Circulation. 1996. 94:61–66.
9. Criqui MH, Cowan LD, Tyroler HA, Bangdiwala S, Heiss G, Wallace RB, et al. Lipoproteins as mediators for the effects of alcohol consumption and cigarette smoking on cardiovascular mortality: results form the Lipid Research Clinics Follow-up Study. Am J Epidemiol. 1987. 126:629–637.
10. Lisabeth L, Bushnell C. Stroke risk in women: the role of menopause and hormone therapy. Lancet Neurol. 2012. 11:82–91.
11. Alberti KG, Eckel RH, Grundy SM, Zimmet PZ, Cleeman JI, Donato KA, et al. Harmonizing the metabolic syndrome: a joint interim statement of the International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; and International Association for the Study of Obesity. Circulation. 2009. 120:1640–1645.
12. World Health Organization. Part 1: diagnosis and classification of diabetes mellitus. Definition, diagnosis and classification of diabetes mellitus and its complications: report of a WHO Consultation. 1999. Geneva, Switzerland: World Health Organization.
13. Ferrannini E, Natali A, Bell P, Cavallo-Perin P, Lalic N, Mingrone G. European Group for the Study of Insulin Resistance (EGIR). Insulin resistance and hypersecretion in obesity. J Clin Invest. 1997. 100:1166–1173.
14. Onat A, Can G, Hergenç G, Yazici M, Karabulut A, Albayrak S. Serum apolipoprotein B predicts dyslipidemia, metabolic syndrome and, in women, hypertension and diabetes, independent of markers of central obesity and inflammation. Int J Obes (Lond). 2007. 31:1119–1125.
15. Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults. Executive Summary of The Third Report of The National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, And Treatment of High Blood Cholesterol In Adults (Adult Treatment Panel III). JAMA. 2001. 285:2486–2497.
16. Grundy SM, Brewer HB Jr, Cleeman JI, Smith SC Jr, Lenfant C. Definition of metabolic syndrome: Report of the National Heart, Lung, and Blood Institute/American Heart Association conference on scientific issues related to definition. Circulation. 2004. 109:433–438.
17. International Diabetes Federation. The IDF consensus worldwide definition of the metabolic syndrome. 2006. Brussels, Belgium: IDF Communications.
18. Gupta R, Sarna M, Thanvi J, Sharma V, Gupta VP. Fasting glucose and cardiovascular risk factors in an urban population. J Assoc Physicians India. 2007. 55:705–709.
19. Gami AS, Witt BJ, Howard DE, Erwin PJ, Gami LA, Somers VK, et al. Metabolic syndrome and risk of incident cardiovascular events and death: a systematic review and meta-analysis of longitudinal studies. J Am Coll Cardiol. 2007. 49:403–414.
20. Galassi A, Reynolds K, He J. Metabolic syndrome and risk of cardiovascular disease: a meta-analysis. Am J Med. 2006. 119:812–819.
21. Donato GB, Fuchs SC, Oppermann K, Bastos C, Spritzer PM. Association between menopause status and central adiposity measured at different cutoffs of waist circumference and waist-to-hip ratio. Menopause. 2006. 13:280–285.
22. Blake GJ, Otvos JD, Rifai N, Ridker PM. Low-density lipoprotein particle concentration and size as determined by nuclear magnetic resonance spectroscopy as predictors of cardiovascular disease in women. Circulation. 2002. 106:1930–1937.
23. Hokanson JE, Austin MA. Plasma triglyceride level is a risk factor for cardiovascular disease independent of high-density lipoprotein cholesterol level: a meta-analysis of population-based prospective studies. J Cardiovasc Risk. 1996. 3:213–219.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download