Abstract
Colorectal cancer (CRC) is a major cause of cancer mortality worldwide, and this has led to an increased use of screening colonoscopy. This screening has resulted in long-term risk reduction in asymptomatic individuals. However, endoscopists may fail to detect advanced adenomas or colon cancer during screening. The reasons that adenomas or cancers are missed are thought to be associated with the location of the lesions or the skills of the endoscopist. To address the limitations of white light endoscopy (WLE) for adenoma detection, advanced endoscopic images have recently been used. Image-enhanced endoscopies (IEEs), including the use of topical dyes, optical filtering, and ultramagnification, allow for gastrointestinal lesion analysis. Many studies have compared the adenoma detection rate (ADR) obtained by using WLE and IEE, but with different results. IEE can be used to help the endoscopist to improve their ADR in screening colonoscopy. This review examines the possible roles of image-enhanced colonoscopy in CRC screening.
Colorectal cancer (CRC) is a major cause of cancer mortality worldwide, with more than 1.2 million new cases diagnosed annually.1 In Korea, according to the statistical yearbook of the Ministry of Health and Welfare, the CRC incidence rates were 54.7 and 36.9 per 100,000 among men and women in 2008, respectively. Thus, CRC is the second most common cancer in men and the fourth most common in women.2
As the majority of CRC cases show the transformation of adenomas into carcinomas over time, early detection and removal of colorectal adenomas is vital for its prevention.3 The adenoma detection rate (ADR) is an independent predictor of the risk of interval CRC after colonoscopy, and it has been adopted as one of the main quality indicators for colonoscopy. The US Multi-Society Task Force on Colorectal Cancer has established target ADRs of ≥25% for men and ≥15% for women undergoing screening colonoscopy.4 This screening has resulted in long-term risk reduction in asymptomatic individuals. However, the role of colonoscopy in CRC prevention is limited by the presence of latent or missed polyps. A systematic review of 6 tandem colonoscopy studies with 465 patients reported a pooled adenoma miss rate for polyps of any size of 22% (95% confidence interval [CI], 19 to 26; 370/1,650 polyps). As expected, the miss rate by size was higher (26%) for small adenomas (1 to 5 mm), compared with those >10 mm (2.1%).5 In addition to missed lesions, another confounding factor in CRC prevention is the variability in ADR among endoscopists. A study that evaluated 2,664 screening colonoscopies found that ADR among different endoscopists ranged from 7% to 44% (p<0.001).6 Similarly, Kaminski et al.7 evaluated 45,026 subjects undergoing a colonoscopy-based CRC screening program and they found a significantly higher risk of interval CRC among subjects who underwent colonoscopy by endoscopists with an ADR of less than 20%, compared with those who had an ADR of 20% or more.
To overcome the limitations of conventional endoscopy for adenoma detection, and to improve and standardize ADRs among endoscopists, there has been a recent trend towards the use of advanced endoscopic techniques, including dye-assisted chromoendoscopy (CE), high-definition white light endoscopy (HD-WLE), and narrow band imaging (NBI) (Table 1).8
Indigo carmine is the most common dye used in image-enhanced endoscopy (IEE). CE with indigo carmine is a relatively classic procedure, but it is still one of the best procedures for evaluating lesions (Fig. 1). It is performed by using standard endoscopes. A diluted solution (0.1% to 0.4%) is sprayed onto the colonic mucosa by using a syringe via a spray catheter or the working channel of the endoscope.
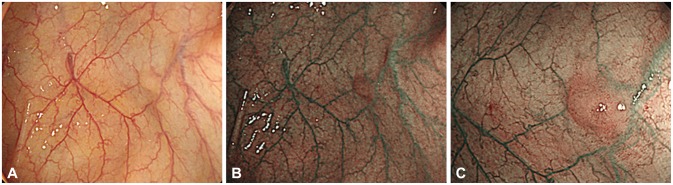
NBI illuminates the tissue surface by using optical filters that narrow the respective red-green-blue bands, while simultaneously increasing the relative intensity of the blue band.9 This spectrum of wavelengths has a decreased depth of penetration and corresponds to the peak absorption spectrum of hemoglobin. The NBI technique overcomes the disadvantages of conventional CE by obviating the need for dyes and allowing conversion from WLE to NBI, and vice versa, by the flick of a switch on the endoscope (Fig. 2). It is therefore considered a more time-efficient procedure than CE.10,11
Fujinon intelligent color enhancement (FICE) is based on a computed spectral estimation technology that arithmetically processes the reflected photons to reconstitute virtual images for a choice of different wavelengths. The system allows the endoscopist to view the enhanced images based on a set of three predetermined, empirically chosen, narrowed wavelengths. Up to 10 variable settings are available through settings on the keyboard; the endoscopist selects the setting that best enhances visualization of microvessels, glands, and pits.10
Autofluorescence imaging (AFI) uses a sequential method composed of short wavelengths of blue light (390 to 470 nm) to excite endogenous fluorophores (emanating from a variety of constituent biomolecules) that then emit green light (540 to 560 nm). In AFI colonoscopy findings, nonneoplastic lesions seem green, whereas neoplastic lesions have a longer wavelength emission, appearing magenta (reddish-purple). The AFI colonoscope is equipped with two charge-coupled devices that can be easily operated by pushing a button on the scope handle; one is for standard high-resolution white light and the other is for autofluorescence.10
The Pentax i-Scan (Pentax, Tokyo, Japan) is a postcapture system with the following three types of enhancement: surface enhancement, contrast enhancement, and tone enhancement. An additional feature of the i-Scan includes the twin mode, which provides simultaneous side-by-side viewing of white light and enhanced images.10
Screening for CRC by using fecal occult blood testing, sigmoidoscopy, or colonoscopy is recommended in several countries, mostly for patients aged >50 years with an average risk, and earlier screening is recommended in people with a strong family history or other risk factors.
For colorectal neoplasia detection in asymptomatic and symptomatic patients, excluding inflammatory bowel disease (IBD), a recent Cochrane Database of Systemic Review of five randomized trials demonstrated that CE with indigo carmine yielded significantly more patients with at least one (odds ratio [OR], 1.67; 95% CI, 1.29 to 2.15) and three or more (OR, 2.55; 95% CI, 1.49 to 4.36) neoplastic lesions compared with standard colonoscopy.12 After the publication of the Cochrane Database of Systemic Review, four randomized controlled trials (RCTs) have compared HD-WLE with conventional CE for detecting adenomas.13,14,15,16 Only one RCT showed that conventional CE did not detect significantly more adenomas compared with HD-WLE (32.7% vs. 26.9%, p=0.47).15
Although dye-assisted CE has been established to be superior to conventional colonoscopy for the detection of colonic adenomas, the procedure is both cumbersome and time consuming. Several studies have compared ADR by WLE and NBI, but have shown conflicting results. This discrepancy in results is related to a lack of consistency in the modalities being compared (HD-NBI vs. HD-WLE and HD-NBI vs. standard definition [SD]-WLE), inadequately powered studies due to small sample size, in addition to differences in the number and experience of endoscopists involved in the studies.17
Several recent studies have reported the application of equipment-based IEE techniques for adenoma detection. In a meta-analysis by Dinesen et al.,18 data from seven studies with 2,936 patients were pooled. There was no statistically significant difference in the overall ADR with the use of NBI or WLE (36% vs. 34%, p=0.413 [relative risk, 1.06; 95% CI, 0.97 to 1.16]). This is consistent with a previous systemic review, which showed that the pooled OR of detecting adenomas by using NBI, compared with SD-WLE, was 1.23 (95% CI, 0.93 to 1.61), which was not statistically significant.19 Another meta-analysis of nine randomized studies comparing HD-NBI and HD-WLE showed no benefit of HD-NBI over HD-WLE for detection of polyps (six studies: n=2,275; OR, 1.15; 95% CI, 0.8 to 1.64), adenomas (four studies: n=2,177; OR, 1.0; 95% CI, 0.83 to 1.20), adenomas <10 mm (five studies: n=1,618; OR, 1.32; 95% CI, 0.92 to 1.88), or flat adenomas (five studies: n=1,675; OR, 1.26; 95% CI, 0.62 to 2.57).17 There was also no benefit of HD-NBI for lowering the miss rate of polyps or adenomas compared with HD-WLE. Pasha et al.17 found an improvement in adenoma detection and lower miss rates with both HD-WLE and HD-NBI, compared with SD-WLE, which may be attributable to the HD component of the colonoscopes.
AFI for the detection of colorectal neoplasia in average-risk patients has produced conflicting results. AFI technology, in a modified back-to-back colonoscopy pilot study, showed high detection rates of right-sided colonic polyps, especially flat and/or diminutive adenomatous lesions, compared with conventional WLE.20
Data on the use of i-Scan or FICE for the detection of adenomas are scarce. A large, prospective, randomized multicenter trial reported similar adenoma detection properties of FICE compared with conventional colonoscopy, with targeted indigo carmine.21
Patients with IBD have a high risk of colitis-associated dysplasia and cancer. Colitis-associated neoplasms can be difficult to detect because the growth pattern of colitic dysplastic tissue is often multifocal and flat. Most neoplastic and dysplastic lesions in patients with ulcerative colitis (UC) are nonpolypoid, and surveillance colonoscopy with IEE is recommended.22,23 Rutter et al.24 showed a higher sensitivity of pancolonic CE with indigo carmine dye spraying for the detection of intraepithelial neoplasias in patients with long-standing UC. No dysplasia was detected in 2,904 nontargeted biopsies. In comparison, a targeted biopsy protocol with pancolonic CE required fewer biopsies (157), but yet, it detected nine dysplastic lesions, seven of which were only visible after indigo carmine application.24
The use of CE in IBD patients has been recently reviewed in a meta-analysis by Subramanian et al.25 who pooled data from six studies involving 1,277 patients. They reported that CE increased the proportion of detected dysplastic flat lesions by 27% when compared with SD-WLE. They also reported a 44% increase in the proportion of detected dysplastic lesions by using CE compared with SD-WLE.25
The use of equipment-based IEE to detect and diagnose neoplasia in UC has been reported. Dekker et al.26 performed a prospective crossover trial in which patients with UC underwent both NBI and HD-WLE randomly. It was shown that NBI does not improve the detection of neoplasia in patients with UC when compared with HD-WLE. The same research group reported that AFI improved neoplasia detection and decreased the number of random biopsies required when compared with WLE.27
IEE, compared with conventional colonoscopy, can significantly improve adenoma detection in patients with hereditary non-polyposis colorectal cancer (HNPCC) syndrome. Several studies showed higher ADRs with conventional CE compared with SD-WLE or HD-WLE in patients with Lynch syndrome.28,29,30 The role of IEE in patients with HNPCC was assessed in two prospective cohort studies.30,31 East et al.31 performed NBI after WLE in all patients and concluded that the use of NBI in the proximal colon appeared to improve adenoma detection, especially in nonpolypoid lesions. However, this study design did not incorporate a comparative control.
A RCT specifically compared AFI with HD-WLE in patients with Lynch syndrome.32 The sensitivity for the detection of adenomas was significantly higher by using AFI compared with HD-WLE (92% vs. 68%, p=0.01). However, the AFI system used in this study is not widely commercially available.
Advanced images designed to improve polyp detection include the use of dye and equipment-based IEE. The goal of such technology developments should be to improve the quality of colonoscopy, including a focus on increasing ADR. Several of these new technologies can be used to assist the endoscopist to improve their ADR in screening colonoscopy. Ultimately, careful examination of mucosal folds and flexures, meticulous washing of the mucosa, and being vigilant for the presence of adenomas can improve ADR in screening colonoscopy, and help decrease the rate of interval CRC.
References
1. Ferlay J, Shin HR, Bray F, Forman D, Mathers C, Parkin DM. Estimates of worldwide burden of cancer in 2008: GLOBOCAN 2008. Int J Cancer. 2010; 127:2893–2917. PMID: 21351269.

2. Jung KW, Park S, Kong HJ, et al. Cancer statistics in Korea: incidence, mortality, survival, and prevalence in 2008. Cancer Res Treat. 2011; 43:1–11. PMID: 21509157.

3. Winawer SJ, Zauber AG, Ho MN, et al. The National Polyp Study Workgroup. Prevention of colorectal cancer by colonoscopic polypectomy. N Engl J Med. 1993; 329:1977–1981. PMID: 8247072.

4. Rex DK, Bond JH, Winawer S, et al. Multi-Society Task Force on Colorectal Cancer. Quality in the technical performance of colonoscopy and the continuous quality improvement process for colonoscopy: recommendations of the U.S. Am J Gastroenterol. 2002; 97:1296–1308. PMID: 12094842.
5. van Rijn JC, Reitsma JB, Stoker J, Bossuyt PM, van Deventer SJ, Dekker E. Polyp miss rate determined by tandem colonoscopy: a systematic review. Am J Gastroenterol. 2006; 101:343–350. PMID: 16454841.

6. Imperiale TF, Glowinski EA, Juliar BE, Azzouz F, Ransohoff DF. Variation in polyp detection rates at screening colonoscopy. Gastrointest Endosc. 2009; 69:1288–1295. PMID: 19481649.

7. Kaminski MF, Regula J, Kraszewska E, et al. Quality indicators for colonoscopy and the risk of interval cancer. N Engl J Med. 2010; 362:1795–1803. PMID: 20463339.

8. Kaltenbach T, Sano Y, Friedland S, Soetikno R. American Gastroenterological Association. American Gastroenterological Association (AGA) Institute technology assessment on image-enhanced endoscopy. Gastroenterology. 2008; 134:327–340. PMID: 18061178.

9. Gono K, Obi T, Yamaguchi M, et al. Appearance of enhanced tissue features in narrow-band endoscopic imaging. J Biomed Opt. 2004; 9:568–577. PMID: 15189095.

10. Kaltenbach T, Soetikno R. Image-enhanced endoscopy is critical in the detection, diagnosis, and treatment of non-polypoid colorectal neoplasms. Gastrointest Endosc Clin N Am. 2010; 20:471–485. PMID: 20656245.

11. Johanson JF. Practicality of high-resolution chromoendoscopy during routine screening colonoscopy. Gastrointest Endosc. 2006; 63:829–830. PMID: 16650547.

12. Brown SR, Baraza W. Chromoscopy versus conventional endoscopy for the detection of polyps in the colon and rectum. Cochrane Database Syst Rev. 2010; (10):CD006439. PMID: 20927746.

13. Pohl J, Schneider A, Vogell H, Mayer G, Kaiser G, Ell C. Pancolonic chromoendoscopy with indigo carmine versus standard colonoscopy for detection of neoplastic lesions: a randomised two-centre trial. Gut. 2011; 60:485–490. PMID: 21159889.

14. Togashi K, Hewett DG, Radford-Smith GL, Francis L, Leggett BA, Appleyard MN. The use of indigocarmine spray increases the colonoscopic detection rate of adenomas. J Gastroenterol. 2009; 44:826–833. PMID: 19448968.

15. Hashimoto K, Higaki S, Nishiahi M, Fujiwara K, Gondo T, Sakaida I. Does chromoendoscopy improve the colonoscopic adenoma detection rate? Hepatogastroenterology. 2010; 57:1399–1404. PMID: 21443093.
16. Kahi CJ, Anderson JC, Waxman I, et al. High-definition chromocolonoscopy vs. high-definition white light colonoscopy for average-risk colorectal cancer screening. Am J Gastroenterol. 2010; 105:1301–1307. PMID: 20179689.

17. Pasha SF, Leighton JA, Das A, et al. Comparison of the yield and miss rate of narrow band imaging and white light endoscopy in patients undergoing screening or surveillance colonoscopy: a meta-analysis. Am J Gastroenterol. 2012; 107:363–370. PMID: 22186978.

18. Dinesen L, Chua TJ, Kaffes AJ. Meta-analysis of narrow-band imaging versus conventional colonoscopy for adenoma detection. Gastrointest Endosc. 2012; 75:604–611. PMID: 22341105.

19. van den Broek FJ, Reitsma JB, Curvers WL, Fockens P, Dekker E. Systematic review of narrow-band imaging for the detection and differentiation of neoplastic and nonneoplastic lesions in the colon (with videos). Gastrointest Endosc. 2009; 69:124–135. PMID: 19111693.

20. Matsuda T, Saito Y, Fu KI, et al. Does autofluorescence imaging videoendoscopy system improve the colonoscopic polyp detection rate?: a pilot study. Am J Gastroenterol. 2008; 103:1926–1932. PMID: 18647285.
21. Pohl J, Lotterer E, Balzer C, et al. Computed virtual chromoendoscopy versus standard colonoscopy with targeted indigocarmine chromoscopy: a randomised multicentre trial. Gut. 2009; 58:73–78. PMID: 18838485.

22. Jaramillo E, Watanabe M, Slezak P, Rubio C. Flat neoplastic lesions of the colon and rectum detected by high-resolution video endoscopy and chromoscopy. Gastrointest Endosc. 1995; 42:114–122. PMID: 7590045.

23. Farraye FA, Odze RD, Eaden J, Itzkowitz SH. AGA technical review on the diagnosis and management of colorectal neoplasia in inflammatory bowel disease. Gastroenterology. 2010; 138:746–774. PMID: 20141809.

24. Rutter MD, Saunders BP, Schofield G, Forbes A, Price AB, Talbot IC. Pancolonic indigo carmine dye spraying for the detection of dysplasia in ulcerative colitis. Gut. 2004; 53:256–260. PMID: 14724160.

25. Subramanian V, Mannath J, Ragunath K, Hawkey CJ. Meta-analysis: the diagnostic yield of chromoendoscopy for detecting dysplasia in patients with colonic inflammatory bowel disease. Aliment Pharmacol Ther. 2011; 33:304–312. PMID: 21128987.

26. Dekker E, van den Broek FJ, Reitsma JB, et al. Narrow-band imaging compared with conventional colonoscopy for the detection of dysplasia in patients with longstanding ulcerative colitis. Endoscopy. 2007; 39:216–221. PMID: 17385106.

27. van den Broek FJ, Fockens P, van Eeden S, et al. Endoscopic tri-modal imaging for surveillance in ulcerative colitis: randomised comparison of high-resolution endoscopy and autofluorescence imaging for neoplasia detection; and evaluation of narrow-band imaging for classification of lesions. Gut. 2008; 57:1083–1089. PMID: 18367559.

28. Lecomte T, Cellier C, Meatchi T, et al. Chromoendoscopic colonoscopy for detecting preneoplastic lesions in hereditary nonpolyposis colorectal cancer syndrome. Clin Gastroenterol Hepatol. 2005; 3:897–902. PMID: 16234028.

29. Hurlstone DP, Karajeh M, Cross SS, et al. The role of high-magnification-chromoscopic colonoscopy in hereditary nonpolyposis colorectal cancer screening: a prospective "back-to-back" endoscopic study. Am J Gastroenterol. 2005; 100:2167–2173. PMID: 16181364.

30. Hüneburg R, Lammert F, Rabe C, et al. Chromocolonoscopy detects more adenomas than white light colonoscopy or narrow band imaging colonoscopy in hereditary nonpolyposis colorectal cancer screening. Endoscopy. 2009; 41:316–322. PMID: 19340735.

31. East JE, Suzuki N, Stavrinidis M, Guenther T, Thomas HJ, Saunders BP. Narrow band imaging for colonoscopic surveillance in hereditary non-polyposis colorectal cancer. Gut. 2008; 57:65–70. PMID: 17682000.

32. Ramsoekh D, Haringsma J, Poley JW, et al. A back-to-back comparison of white light video endoscopy with autofluorescence endoscopy for adenoma detection in high-risk subjects. Gut. 2010; 59:785–793. PMID: 20551463.

Fig. 1
A superficial elevated flat neoplasm detected on white light endoscopy (A) and chromoendoscopy with indigo carmine (B).
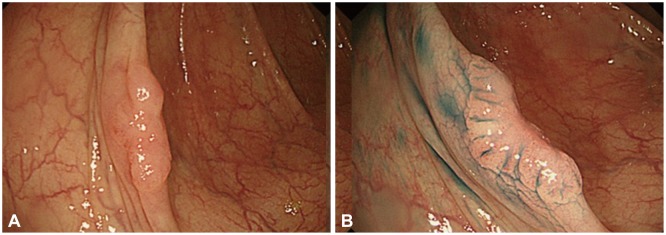
Table 1
Image-Enhanced Endoscopy
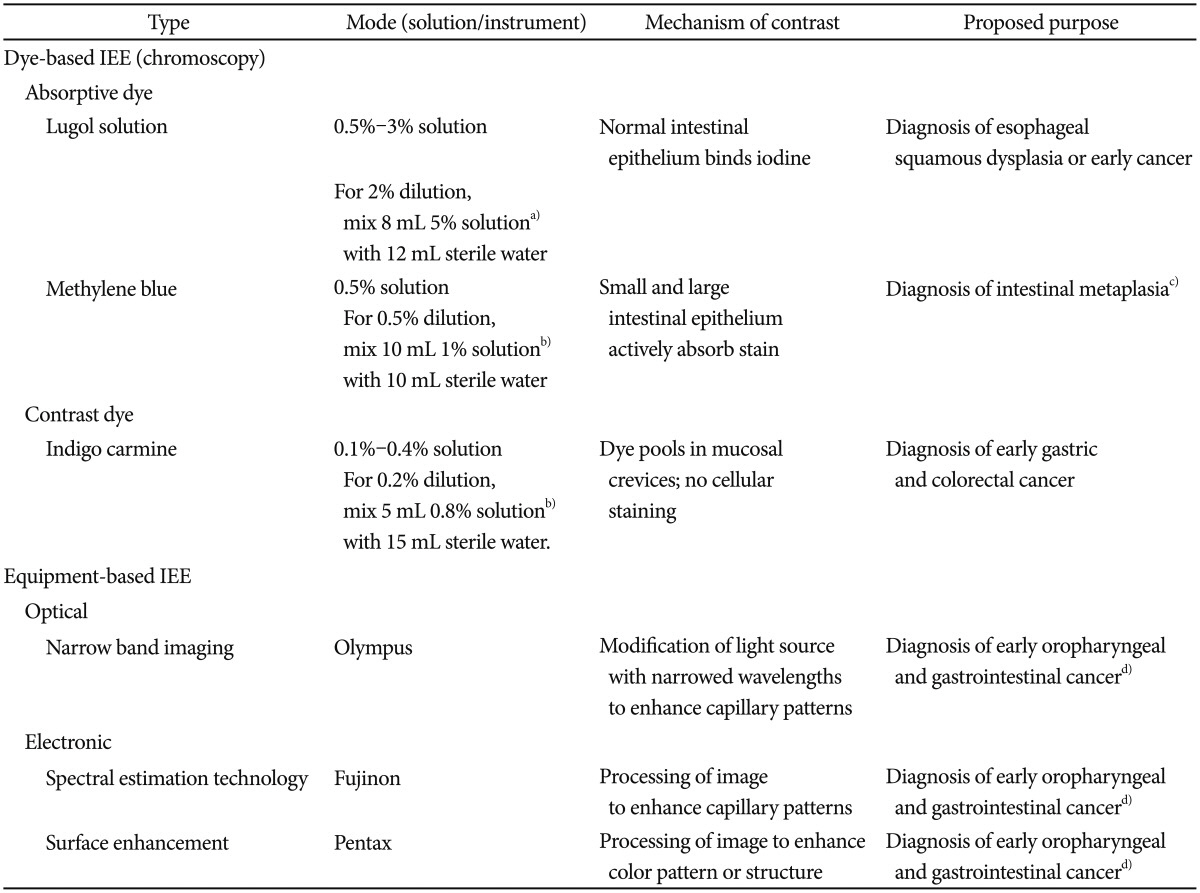
a)Humcon Co., Texarkana, TX, USA; b)American Regent Laboratories Inc., Shirley, NY, USA; c)Methylene blue has also been proposed to improve endoscopic detection of Barrett esophagus, although there is currently insufficient evidence to support its routine use in this setting; d)There are currently limited data on equipment-based image-enhanced endoscopy (IEE), most of which relates to narrow band imaging.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download