Abstract
Background/Aims
In recent years, endoscopic snare papillectomy has been performed to treat tumors of the ampulla of Vater. This procedure requires accurate preoperative evaluation. In this study, we diagnosed the focal extension of such tumors by using endoscopic ultrasonography (EUS) and intraductal ultrasonography (IDUS), and examined the indications for endoscopic snare papillectomy.
Methods
The subjects were 48 patients with a papillary tumor (13 patients, surgical resection; 35 patients, endoscopic snare papillectomy) who were evaluated preoperatively with EUS and IDUS. The tumor-node-metastasis classification was used for the endosonographic evaluation and pathological diagnosis of these tumors.
Results
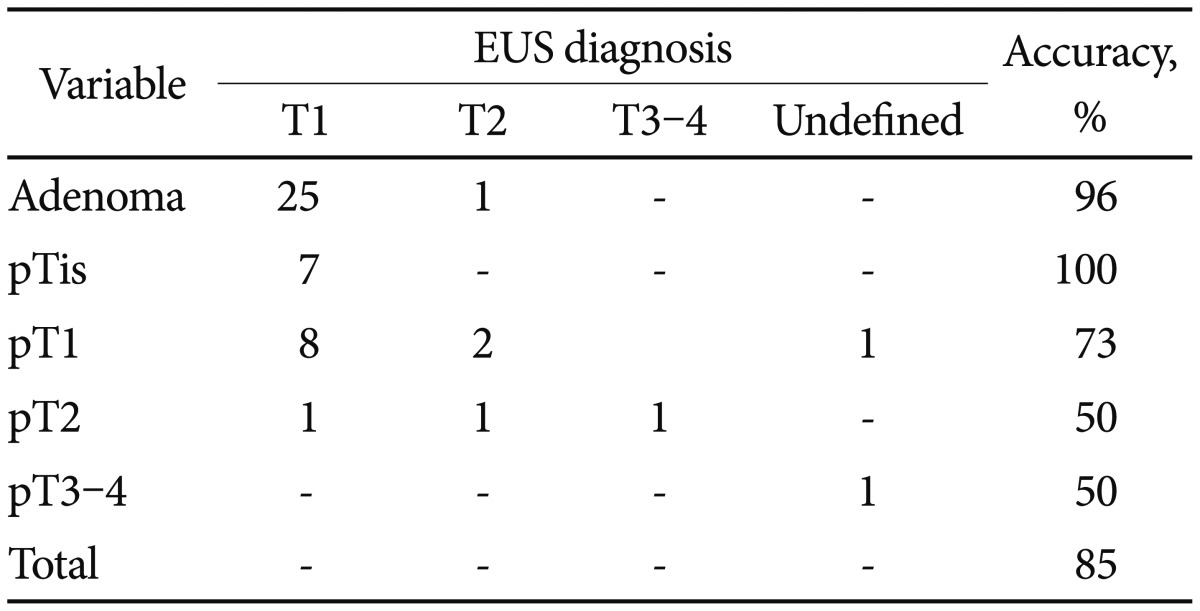
The diagnostic accuracy of EUS was 97% for diagnosing adenomas and pTis tumors, 73% for pT1 tumors, 50% for pT2 tumors, and 50% for pT3-4 tumors, for an overall accuracy of 85% for T-staging. The diagnostic accuracy of IDUS was 94% for adenomas and pTis tumors, 73% for pT1 tumors, 50% for pT2 tumors, and 100% for pT3-4 tumors, for an overall accuracy of 80% for T-staging.
Conclusions
EUS and IDUS are highly capable of evaluating tumors of the ampulla of Vater preoperatively. However, these techniques are not sufficient for evaluating the focal extension of carcinomas preoperatively. Currently, endoscopic snare papillectomy is adequate for treating adenomas and pTis tumors.
A pancreaticoduodenectomy (PD) or pylorus-preserving PD (PpPD) has traditionally been performed to treat tumors of the ampulla of Vater. Since a report on the use of endoscopic snare papillectomy to treat tumors of the ampulla of Vater was published in 1983,1 reports about this procedure have gradually increased. Because it is minimally invasive, the procedure is used as a limited surgery and for complete biopsy; however, there is no consensus concerning its indications because of problems with the accuracy of preoperative evaluation. In the current study, we examined the indications for endoscopic snare papillectomy based on the focal extension of the tumor diagnosed with endoscopic ultrasonography (EUS) and intraductal ultrasonography (IDUS).
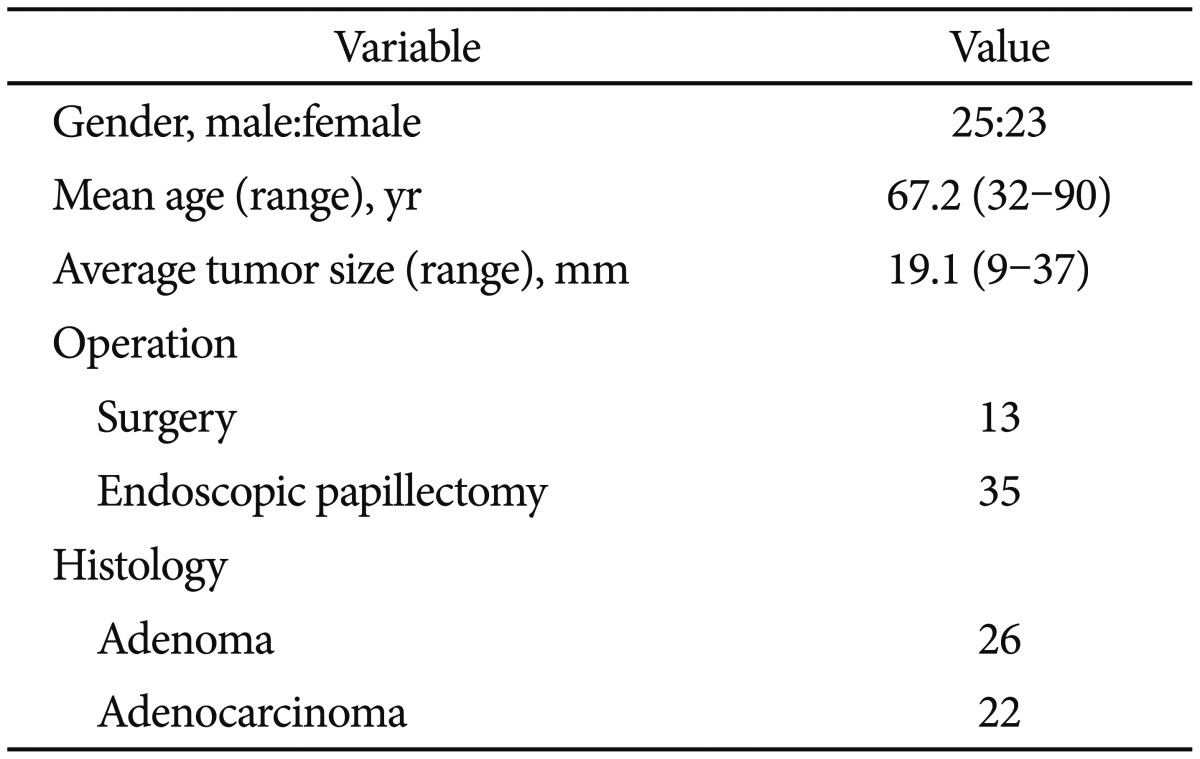
The subjects were 48 patients with tumors of the ampulla of Vater who underwent EUS and IDUS preoperatively from January 2006 to March 2013. Computed tomography (CT) and magnetic resonance cholangiopancreatography (MRCP) were performed before EUS or IDUS. The patients included 25 men and 23 women with a mean age of 67.2 years (range, 32 to 90 years). Thirteen patients underwent surgical resection (PpPD) and 35 underwent endoscopic snare papillectomy. The final pathological diagnosis was adenocarcinoma for 22 patients (including pTis tumor for 7) and adenoma for 26 patients. The mean tumor size was 19.1 mm (range, 9 to 37 mm) (Table 1).
Endoscopic snare papillectomy was performed on patients when EUS/IDUS, CT, and MRCP indicated that the tumor was limited to the mucosa, had not extended into the bile and pancreatic ducts, and had not extended beyond the sphincter of Oddi. Surgical resection was performed on patients when either examination procedure indicated an evidence of extension.
EUS was performed with an electronic radial scanning scope (GF-UM200 or GF-UM2000; Olympus Medical Systems, Tokyo, Japan) at frequencies of 6, 7.5, and 10 MHz. The scope was first advanced into the descending part of the duodenum; a balloon at the end was inflated with distilled water; and then distilled water was infused into the duodenum through the working channel before observation. IDUS was performed with an ultrasound probe (UM-G20-29R; Olympus Medical Systems) at a frequency of 20 MHz. After cholangiopancreatography, the probe was inserted through the working channel of a TJF240 duodenoscope (Olympus Medical Systems) into the bile and pancreatic ducts, guided by a 0.889-mm guidewire before observation. All procedures were performed by 2 endoscopists with ≥10 years of experience in performing ERCP/EUS.
The tumor-node-metastasis (TNM) classification was used for preoperative endosonographic evaluation and pathological diagnosis with EUS and IDUS (T1, tumor limited to the ampulla of Vater; T2, tumor invading the duodenal wall; T3-4, tumor invading the pancreas).2 Extension into the bile and pancreatic ducts was also examined. EUS and IDUS results were considered positive when they revealed either an intraductal mass or wall thickening adjacent to a papillary tumor, and these results were compared with the pathological diagnosis. All patients gave written informed consent, and the study was approved by the Institutional Review Board of Toho University Omori Medical Center.
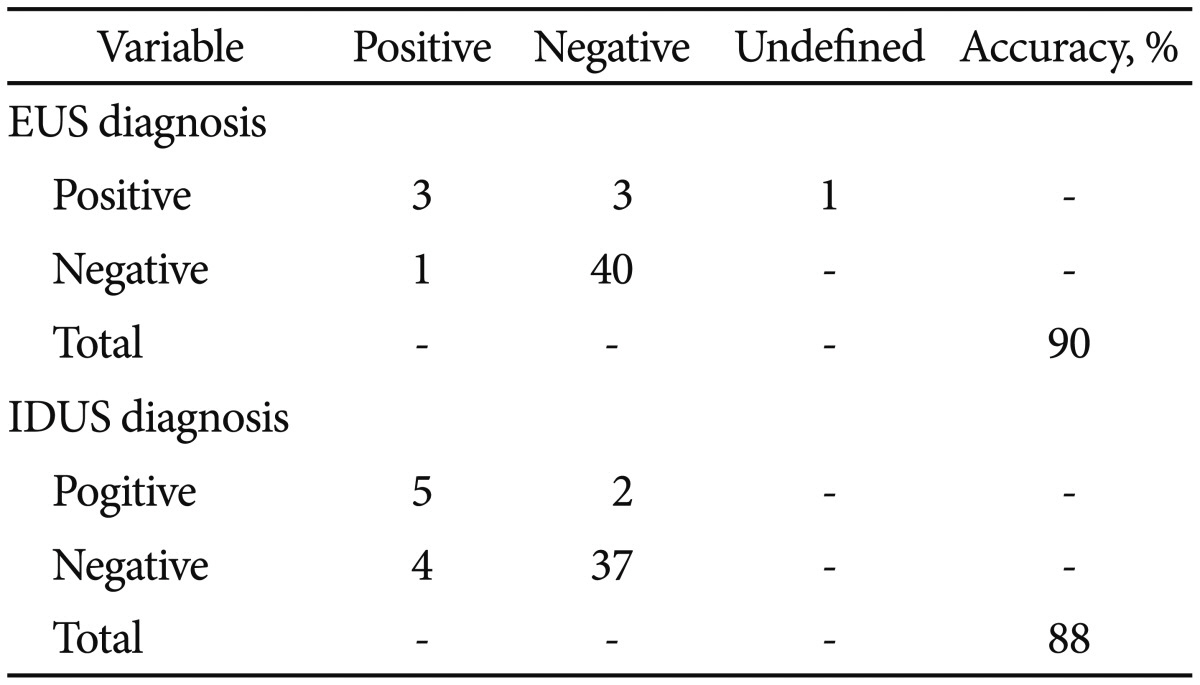
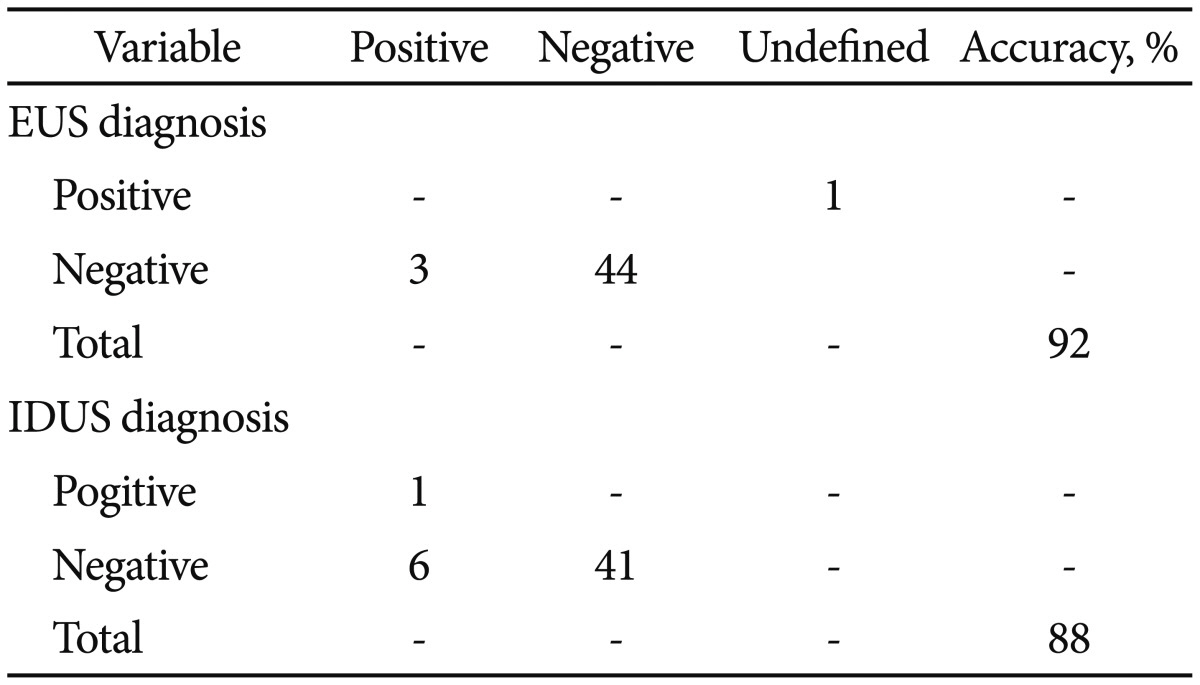
Two of 41 patients could not be evaluated because of poor visualization of the muscularis propria of the duodenum. The T category according to EUS had a diagnostic accuracy of 97% for adenoma and pTis tumor, 73% for pT1 tumor, 50% for pT2 tumor, and 50% for pT3-4 tumor, for an overall accuracy of 85% (Table 2). Results were overestimated in 1 patient with an adenoma and 2 patients with a pT1 tumor; all 3 patients were considered to have evidence of thickness of the muscularis propria. Results were underestimated in one patient with a pT2 tumor of the duodenum; determination of invasion of the muscularis propria was difficult because of attenuation within the tumor. Extension into the bile duct could not be evaluated in one patient owing to poor visualization of the bile duct. Extension into the bile duct was evaluated with an accuracy of 90% (Table 3). The result was overestimated in one patient considered to have extension, with the tumor protruding into the bile duct. Results were underestimated in three patients, and invasion of the duodenal wall was discriminated in none of them. Concerning extension into the pancreatic ducts, visualization of the pancreatic ducts was difficult in one patient. Extension into the pancreatic ducts was evaluated with an accuracy of 92% (Table 4).
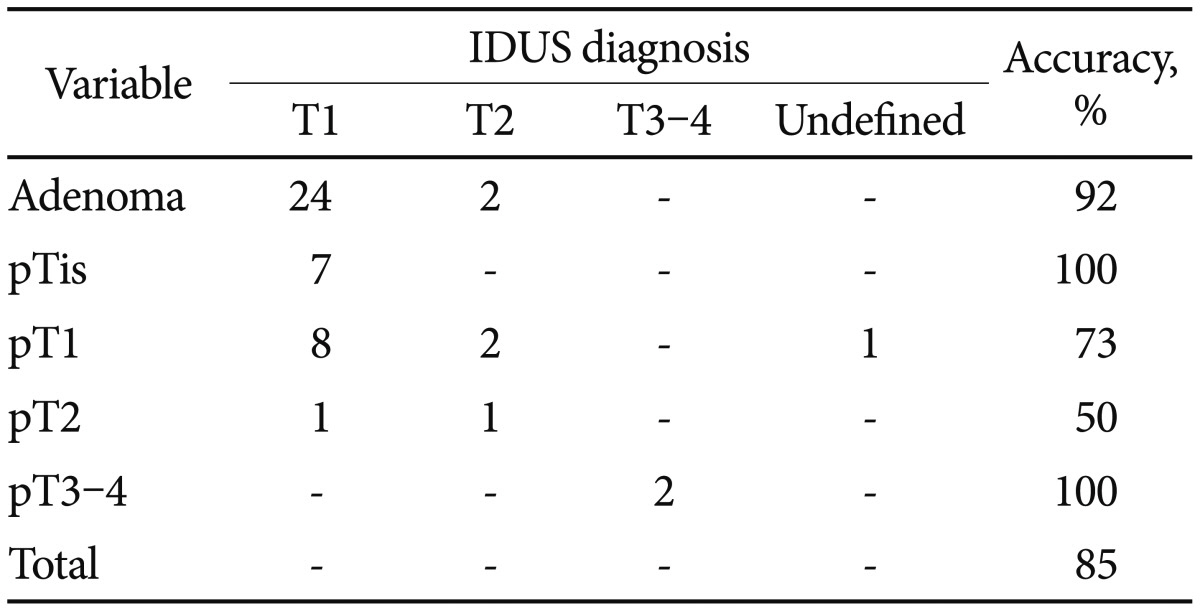
One of 41 patients could not be evaluated because of poor visualization of the sphincter of Oddi. The T category according to IDUS had an accuracy of 94% for diagnosing adenomas and pTis tumors, 73% for pT1 tumors, 50% for pT2 tumors, and 100% for pT3-4 tumors, for an overall accuracy of 85% (Table 5). Results were overestimated in four patients who were considered to have evidence of displacement of the muscularis propria of the duodenum by a tumor. The result was underestimated in one patient in whom invasion of the muscularis propria of the duodenum was not discriminated. Extension into the bile and pancreatic ducts was successfully evaluated in all patients. Extension into the bile duct was evaluated with an accuracy of 88%. Results were overestimated in four patients: one patient was considered to have evidence of tumor protrusion into the bile duct, and three were considered to have evidence of displacement of the bile duct by a tumor (Table 3). Extension into the pancreatic ducts was evaluated with an accuracy of 88%. Results were overestimated in six patients who were all considered to have evidence of displacement of a pancreatic duct by a tumor (Table 4). No complications of EUS and IDUS were noted in any of the patients.
The prevalence of upper gastrointestinal endoscopy has facilitated the observation of the descending part of the duodenum and increased the chances of detecting tumors of the ampulla of Vater. Surgical resection with a procedure such as PD or PpPD has traditionally been used to treat tumors of the ampulla of Vater. A consensus has been reached about the standard use of the procedures for treating tumors of the ampulla of Vater. However, their invasiveness is a problem for elderly patients and patients with any complications. Thanks to recent advances in endoscopic therapy, reports of endoscopic snare papillectomy have increased because of its minimal invasiveness.3,4 The general view is that endoscopic snare papillectomy can be performed on a tumor that has not invaded the muscularis propria of the duodenum but is not indicated when the tumor extends into the hepatic and pancreatic ducts.5 Thus, accurate preoperative evaluation is needed to perform an endoscopic snare papillectomy. A correlation between invasion of the duodenum or pancreas and prognosis has been noted,6 and preoperative evaluation with EUS or IDUS is crucial.
EUS is helpful in diagnosing the extent of papillary tumors because of its high spatial resolution;7 also, it allows better evaluation of focal extension than CT or magnetic resonance imaging.8,9,10 Previous reports have indicated that the T category according to EUS had a 62% to 90% ability to diagnose focal extension.8,9,10,11,12,13,14,15 In the current study, the T category had a diagnostic accuracy of 85%. It had a diagnostic accuracy of 100% in 35 patients undergoing endoscopic snare papillectomy (12 with adenocarcinoma, including pTis tumor for 7, and 23 with adenoma) and an accuracy of 70% in 13 patients undergoing surgical resection (10 with carcinoma, 3 with adenoma). In Ito et al.'s report,15 15% of the patients could not be evaluated because the muscularis propria of the duodenum was not clearly visualized. Similarly, 4% of the current patients (2 of 48) could not be evaluated. The current study also noted a diagnostic accuracy of 97% for diagnosing adenomas and pTis tumors but an accuracy of 67% for diagnosing adenocarcinomas (>pT1). An adenoma can be uniformly hypoechoic inside, whereas an adenocarcinoma can have heterogeneous internal echoes. Extensive evaluation can be difficult owing to echo attenuation disturbing the focal evaluation of an adenocarcinoma. Electronic radial scanning scopes have just recently been developed, and their diagnostic accuracy needs to further improve. Itoh et al.13 reported an accuracy of 85.7% and 76.9% with regard to diagnosing extension into the bile duct and pancreatic ducts, respectively, whereas Ito et al.15 reported an accuracy of 88% and 90%, respectively. Similarly, the current study noted a high diagnostic accuracy of 90% and 92% for the bile duct and pancreas, respectively.
IDUS uses high frequencies and thus provides higher-resolution images than EUS. It also helps in diagnosing the extent of small tumors, i.e., reaching the sphincter of Oddi, as well as the extent of extension into the hepatic and pancreatic ducts. Previous reports indicated that the T category according to IDUS had a 78% to 93% ability to diagnose focal extension.12,13,15 The current study noted an overall accuracy of 85%. Concerning the type of tumor, the accuracy of the T category was 94% for adenomas and pTis tumors, 73% for pT1 tumors, 50% for pT2 tumors, and 100% for pT3-4 tumors; thus, its accuracy tended to decrease in proportion to the extent of the tumor. This is due to the limitations on extensive evaluation (approximately 20 mm) because it uses a high frequency (20 MHz); evaluation of the muscularis propria of the duodenum is disturbed by attenuation within a larger tumor. One of the current patients who could not be evaluated had a large tumor (37 mm). However, IDUS allows visualization of the sphincter of Oddi; thus, a tumor located as far as the sphincter of Oddi can be evaluated. In the current patients who underwent endoscopic snare papillectomy, focal extension was discerned with a high accuracy of 97%. In previous reports, IDUS diagnosed extension into the bile duct and pancreatic ducts with an accuracy of 90% to 95% and 90% to 100%, respectively,13,15 and in the current study, it had a high accuracy of 88% for both.
In this study, there was no significant difference in the accuracy of EUS and IDUS for evaluating focal extension. For preoperative evaluation of tumors of the ampulla of Vater, either EUS or IDUS is necessary. Furthermore, this study provides sufficient ground for the use of EUS or IDUS to preoperatively evaluate adenomas and pTis tumors; however, there is insufficient ground for using these procedures to evaluate adenocarcinomas. Currently, these procedures are not sufficient for an exact preoperative evaluation of the focal extension of adenocarcinomas. However, from the viewpoint of preoperative evaluation, endoscopic snare papillectomy should now be indicated for adenomas and pTis tumors.
In conclusion, in this study, we examined the ability of EUS and IDUS to diagnose the focal extension of tumors of the ampulla of Vater. These procedures help in diagnosing focal extension and are essential when considering limited surgery. Preoperative diagnosis of the focal extension of a carcinoma may prove difficult under the current circumstances; however, endoscopic snare papillectomy is adequate at treating adenomas and pTis tumors.
References
1. Suzuki K, Kantou U, Murakami Y. Two cases with ampullary cancer who underwent endoscopic excision. Prog Dig Endosc. 1983; 23:236–239.
2. Hamilton SR, Aaltonen LA. Pathology and genetics of tumours of the digestive system. Lyon: International Agency for Research on Cancer Press;2000.
3. Norton ID, Gostout CJ, Baron TH, Geller A, Petersen BT, Wiersema MJ. Safety and outcome of endoscopic snare excision of the major duodenal papilla. Gastrointest Endosc. 2002; 56:239–243. PMID: 12145603.

4. Okano N, Igarashi Y, Tomihiro M, Miki K. The study of early complications of endoscopic papillectomy of the tumor with duodenal major papilla. Tando. 2007; 21:623–629.
5. Binmoeller KF, Boaventura S, Ramsperger K, Soehendra N. Endoscopic snare excision of benign adenomas of the papilla of Vater. Gastrointest Endosc. 1993; 39:127–131. PMID: 8495831.

6. Nakao A, Harada A, Nonami T, et al. Prognosis of cancer of the duodenal papilla of Vater in relation to clinicopathological tumor extension. Hepatogastroenterology. 1994; 41:73–78. PMID: 8175122.
7. Yasuda K, Mukai H, Cho E, Nakajima M, Kawai K. The use of endoscopic ultrasonography in the diagnosis and staging of carcinoma of the papilla of Vater. Endoscopy. 1988; 20(Suppl 1):218–222. PMID: 3049060.

8. Cannon ME, Carpenter SL, Elta GH, et al. EUS compared with CT, magnetic resonance imaging, and angiography and the influence of biliary stenting on staging accuracy of ampullary neoplasms. Gastrointest Endosc. 1999; 50:27–33. PMID: 10385718.

9. Chen CH, Tseng LJ, Yang CC, Yeh YH, Mo LR. The accuracy of endoscopic ultrasound, endoscopic retrograde cholangiopancreatography, computed tomography, and transabdominal ultrasound in the detection and staging of primary ampullary tumors. Hepatogastroenterology. 2001; 48:1750–1753. PMID: 11813616.
10. Artifon EL, Couto D Jr, Sakai P, da Silveira EB. Prospective evaluation of EUS versus CT scan for staging of ampullary cancer. Gastrointest Endosc. 2009; 70:290–296. PMID: 19523619.

11. Kubo H, Chijiiwa Y, Akahoshi K, Hamada S, Matsui N, Nawata H. Preoperative staging of ampullary tumours by endoscopic ultrasound. Br J Radiol. 1999; 72:443–447. PMID: 10505006.

12. Menzel J, Hoepffner N, Sulkowski U, et al. Polypoid tumors of the major duodenal papilla: preoperative staging with intraductal US, EUS, and CT: a prospective, histopathologically controlled study. Gastrointest Endosc. 1999; 49(3 Pt 1):349–357. PMID: 10049419.
13. Itoh A, Goto H, Naitoh Y, Hirooka Y, Furukawa T, Hayakawa T. Intraductal ultrasonography in diagnosing tumor extension of cancer of the papilla of Vater. Gastrointest Endosc. 1997; 45:251–260. PMID: 9087831.

14. Skordilis P, Mouzas IA, Dimoulios PD, Alexandrakis G, Moschandrea J, Kouroumalis E. Is endosonography an effective method for detection and local staging of the ampullary carcinoma? A prospective study. BMC Surg. 2002; 2:1. PMID: 11914153.

15. Ito K, Fujita N, Noda Y, et al. Preoperative evaluation of ampullary neoplasm with EUS and transpapillary intraductal US: a prospective and histopathologically controlled study. Gastrointest Endosc. 2007; 66:740–747. PMID: 17905017.

Table 3
Results of Pathological by Endoscopic Ultrasonography and Intraductal Ultrasonography Evaluation for Infiltration into Bile Duct




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download