Abstract
Although endoscopic hemostasis remains initial treatment modality for nonvariceal gastrointestinal (GI) bleeding, severe bleeding despite endoscopic management occurs in 5% to 10% of the patients, requiring surgery or transcatheter arterial embolization (TAE). TAE is now considered the first-line therapy for massive GI bleeding refractory to endoscopic management. GI endoscopists need to be familiar with indications, principles, outcomes, and complications of TAE, as well as embolic materials available.
In gastrointestinal (GI) bleeding, endoscopic diagnosis and therapy is the initial treatment of choice as it is imperative to determine whether bleeding is variceal or arterial, and endoscopic treatments usually achieve primary hemostasis in the majority of patients. However, 10% to 30% of these patients have repeat bleeding.1 In a recent national audit in the UK, salvage surgery and transcatheter arterial embolization (TAE) were required in fewer than 4% of patients with nonvariceal upper GI bleeding.2
After the first report of selective TAE of gastroepiploic artery for the control of acute gastric bleeding,3 improvements in interventional devices and embolic materials and wider availability of skilled interventional radiologists have increased the utility of TAE procedures in the management of GI bleeding.4 TAE seems now accepted as the salvage treatment of choice over surgery for acute bleeding in the upper GI tract despite endoscopic treatment. Decision making to choose TAE or surgery depends on the condition of the patients or their availability.
A typical candidate patient presents with the followings: 1) endoscopy-refractory acute GI bleeding. In previous studies, endoscopy had been performed and failed in average 99% of the study patients: significant amount of blood in the stomach, large ulcer size, location of lesion at posterior bulbar duodenum, multiple lesions, and lesser curve were identified as causes of endoscopic failure.5 High risk patients tend to be directed toward TAE rather than surgery;5 2) massive bleeding (transfusion requirement of at least 4 U of blood over 24 hours) or hemodynamic compromise (systolic blood pressure <100 mm Hg and heart rate >100 beats per minute or clinical shock); and 3) recurrent bleeding after surgery.
It is important to do the angiography while the patient is bleeding. It is not necessary to wait until the patient is hypotensive or unstable.
There are no absolute contraindications because angiography and TAE may be needed as lifesaving procedures. Relative contraindications include renal insufficiency, contrast allergy, and uncorrectable coagulopathy. There is increased risk of gastric or duodenal infarction after TAE in patients with previous extensive upper GI surgery or radiotherapy. If the rate of bleeding is massive, surgery may be preferable to angiography, since angiography may not be able to control the bleeding as quickly as surgery.4
Digital subtraction angiography seems to have equivalent detection rate to scintigraphic images.4 The major limitation of angiography relates to the intermittent nature of bleeding, which can result in a negative result if the bleeding has temporarily stopped at the time of contrast injection.4
It is important to select a vessel that is most likely to supply the bleeding according to history, clinical signs, as well as localization provided by endoscopy, scintigraphic images or computed tomography scans. Thus, we can initiate treatment and stabilize the patient quickly. Aortograms are usually not performed, since only small percentage of contrast will get to the bleeding site and fill multiple overlapping vessels, making identification of the bleeding vessel difficult.
For upper GI bleeding, angiography is centered on the anatomy of the celiac artery; left gastric artery supplies superior lesser curvature and cardiac region, right gastric artery supplies inferior lesser curvature, short gastric artery from splenic artery supplies superior greater curvature and the fundus, and gastroduodenal artery supplies remainder of the stomach and duodenum. The superior mesenteric artery may supply portions of the duodenum, mostly by way of pancreaticoduodenal anastomoses, which are important as a rich collateral supply, but it also may be responsible for rebleeding after TAE.
For lower GI bleeding, angiography is centered on the superior and inferior mesenteric arteries; superior mesenteric artery supplies portions of the duodenum to transverse colon, and inferior mesenteric artery supplies the descending colon, sigmoid colon to superior portion of the rectum. When rectal bleeding is suspicious, both internal iliac arteries should be included because middle and inferior rectal branches come off internal iliac arteries.
1) Glucagon and Buscopan may be given before the procedure to decrease bowel motility and motion artifacts during digital subtraction angiography.
2) Provocative angiography such as infusion of tolazoline (vasodilator), heparin, or even thrombolytics (tissue plasminogen activator), can stimulate bleeding.
3) Longer injection durations or use of carbon dioxide for contrast medium can also improve sensitivity for small bleedings.5
4) Endoscopic clips placed around the area of bleeding during pre-embolization endoscopy can help localize the accurate bleeding vessels. If no extravasation is seen despite the injection of contrast, then the branches terminating at the clip are superselected using microcatheter techniques and embolized.6,7
5) Oblique views can provide clearer view of colic vessels in flexures. Right and left anterior oblique views open up hepatic and splenic flexures, respectively.
The only direct angiographic sign of GI bleeding is extravasation of contrast medium into the bowel lumen (Fig. 1). Indirect signs include aneurysms/pseudoaneurysms, vessel irregularity, vessel cutoff and arteriovenous/arterioportal shunting, neovascularity, and increased vascularity from dilated arterioles (as seen in angiodysplasia) (Fig. 2).4
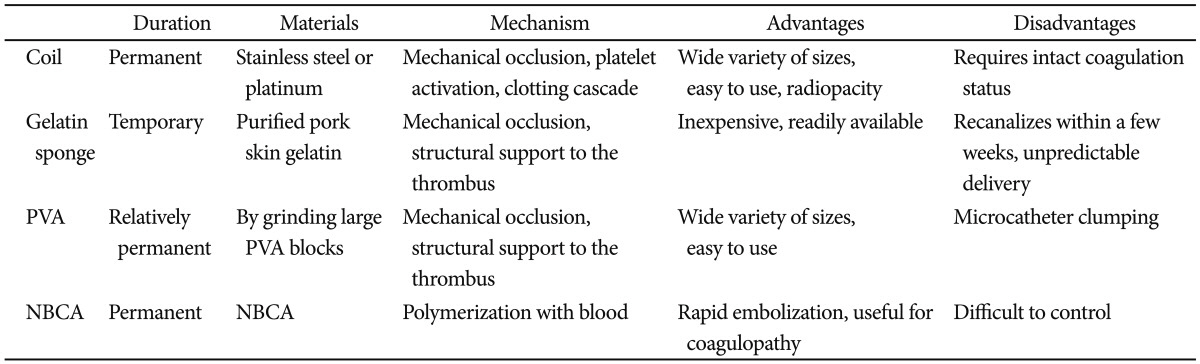
The choice of embolic agent depends on a combination of the vascular anatomy, angiographic findings, the achievable catheter position, and the operator's preference (Table 1). Vessel diameter and the nature of permanent or temporary embolization should be also considered. The most common embolic agents are metallic coils and gelfoam.8 Use of coils as the only embolic agent is significantly associated with early rebleeding, compared with the use of polyvinyl alcohol or gelatin sponge with coils.9,10 Use of N-butyl cyanoacrylate (NBCA) has gained acceptance recently (Fig. 1). It is a liquid embolic material with nonradiopaque nature and, therefore, it should be mixed with lipiodol to provide radiopacity and to control the viscosity. The more diluted NBCA concentration is, the deeper penetration to the distal is achieved. Usually NBCA: lipiodol ratio ranges from 1:1 to 1:4. It is advantageous for massive bleeding that requires urgent hemostasis, especially in patients with coagulopathy because of rapid polymerization with blood.
The tip of the microcatheter should be as distal as possible until the bleeding point (e.g., vasa recta in small and inferior mesenteric arteries). The distal location lowers blood pressure and facilitates clot formation, and risk of back flow to the bleeding point becomes lower. For example, in cases of small bowel branches, there is potential collateral supply when the microcatheter tip is in proximal arc. The best location of the microcatheter tip is vasa recta.
Five recent representative studies of TAE for nonvariceal GI bleeding in 228 patients showed technical success rates of 92% to 100% and clinical success rates of 51% to 83%.9,11-14 Inability to catheterize the bleeding branch as a result of difficult anatomy (e.g., tortuous hepatic artery) and occluded access (e.g., stenosed celiac trunk or common hepatic artery) were the most common reported cause of technical failure.8
Rebleeding rates were 9% to 47%, rates for surgery were 0% to 35%, and 30-day mortality rates were 3% to 27%. Such wide ranges in clinical success and rebleeding rates, rates for surgery, as well as 30-day mortality rates seem to have originated from different etiologies and clinical severities.
Because of the intermittent nature of many incidents of GI bleeding, the incidence of a normal angiogram in patients with acute upper and lower GI bleeding was 52% (75 out of 143 patients) in one recent report.15 In the latter study, the incidence of angiographically negative outcome was significantly higher in patients with a stable hemodynamic status, or in patients with lower GI bleeding.
If no evidence of bleeding is found on pre-TAE arteriogram, then empiric embolization (usually with gelatin sponge and/or coils), defined as embolization without angiographic evidence of active bleeding, could be an alternative and is typically guided by endoscopic information regarding the location of the bleeding vessel.5 Empiric embolization for the upper GI bleeding is advocated because GI bleeding is quite intermittent and accompanied by high rebleeding and mortality rate, if untreated. Angiographic confirmation of a bleeding site seems not a prerequisite for TAE in the upper GI bleeding. Several studies showed no difference in clinical outcomes between patients with negative and patients with positive angiography results when both were treated with TAE.14,16-19
The wide array of alternatives for the treatment of GI bleeding after endoscopic failure make the decision of when to resort to emergency surgery more difficult, especially in patients with high surgical risk.5
Controlled trials comparing TAE with surgery as a salvage procedure for failed endoscopic therapy is limited. Two retrospective comparative studies involving a total of 70 and 91 patients, showed at least similar efficacy in terms of the rate of rebleeding, morbidity, and mortality.20,21 Whereas, a recent retrospective comparative study including 93 patients showed significantly higher rebleeding rates in patients after TAE compared with surgery (46.7% vs. 12.7%), although the authors admitted that only coil or gelfoam use in the earlier cases could have contributed to the high rebleeding rates in TAE group.22
Nonetheless, TAE could not replace surgery. Although continuous bleeding demands emergency TAE, especially in high surgical risk patients, surgery is preferred in young and healthy patients, especially with large and/or multiple peptic ulcers, in the absence of an evidence proving the inferiority of TAE in such a setting.
Periprocedural complications are related to underlying conditions such as advanced age or comorbidities. Many technical complications are without clinical consequences and mostly preventable.
TAE in the upper GI tract above the ligament of Treitz is generally considered very safe because of the rich collateral supply to the stomach and duodenum. However, the risk of significant ischemia or stricture could be increased when potential collateral vessels are damaged from previous upper abdominal surgery, radiotherapy, or severe atherosclerosis, when TAE extent is wide (Fig. 2), or when liquid agents such as NBCA, or very small particles advance far into the vascular bed.4
Lang23 reported a 16% (9/57 patients) incidence rate of duodenal strictures following TAE. If true bowel infarction occurs, surgical resection is generally required (Fig. 2). For more chronic ischemic complications such as bowel stricture, balloon dilation may be possible, but surgical resection should be considered if the stricture is resistant to balloon dilation.
References
1. Loffroy R, Estivalet L, Cherblanc V, et al. Transcatheter embolization as the new reference standard for endoscopically unmanageable upper gastrointestinal bleeding. World J Gastrointest Surg. 2012; 4:223–227. PMID: 23467300.

2. Jairath V, Kahan BC, Logan RF, et al. National audit of the use of surgery and radiological embolization after failed endoscopic haemostasis for non-variceal upper gastrointestinal bleeding. Br J Surg. 2012; 99:1672–1680. PMID: 23023268.

3. Rösch J, Dotter CT, Brown MJ. Selective arterial embolization: a new method for control of acute gastrointestinal bleeding. Radiology. 1972; 102:303–306. PMID: 4536688.
4. Shin JH. Recent update of embolization of upper gastrointestinal tract bleeding. Korean J Radiol. 2012; 13(Suppl 1):S31–S39. PMID: 22563285.

5. Loffroy R, Rao P, Ota S, De Lin M, Kwak BK, Geschwind JF. Embolization of acute nonvariceal upper gastrointestinal hemorrhage resistant to endoscopic treatment: results and predictors of recurrent bleeding. Cardiovasc Intervent Radiol. 2010; 33:1088–1100. PMID: 20232200.

6. Song JS, Kwak HS, Chung GH. Nonvariceal upper gastrointestinal bleeding: the usefulness of rotational angiography after endoscopic marking with a metallic clip. Korean J Radiol. 2011; 12:473–480. PMID: 21852908.

7. Eriksson LG, Sundbom M, Gustavsson S, Nyman R. Endoscopic marking with a metallic clip facilitates transcatheter arterial embolization in upper peptic ulcer bleeding. J Vasc Interv Radiol. 2006; 17:959–964. PMID: 16778228.

8. Mirsadraee S, Tirukonda P, Nicholson A, Everett SM, McPherson SJ. Embolization for non-variceal upper gastrointestinal tract haemorrhage: a systematic review. Clin Radiol. 2011; 66:500–509. PMID: 21371695.

9. Loffroy R, Guiu B, D'Athis P, et al. Arterial embolotherapy for endoscopically unmanageable acute gastroduodenal hemorrhage: predictors of early rebleeding. Clin Gastroenterol Hepatol. 2009; 7:515–523. PMID: 19418601.

10. Aina R, Oliva VL, Therasse E, et al. Arterial embolotherapy for upper gastrointestinal hemorrhage: outcome assessment. J Vasc Interv Radiol. 2001; 12:195–200. PMID: 11265883.

11. Loffroy R, Guiu B, Cercueil JP, et al. Refractory bleeding from gastroduodenal ulcers: arterial embolization in high-operative-risk patients. J Clin Gastroenterol. 2008; 42:361–367. PMID: 18277904.
12. Holme JB, Nielsen DT, Funch-Jensen P, Mortensen FV. Transcatheter arterial embolization in patients with bleeding duodenal ulcer: an alternative to surgery. Acta Radiol. 2006; 47:244–247. PMID: 16613304.

13. Larssen L, Moger T, Bjørnbeth BA, Lygren I, Kløw NE. Transcatheter arterial embolization in the management of bleeding duodenal ulcers: a 5.5-year retrospective study of treatment and outcome. Scand J Gastroenterol. 2008; 43:217–222. PMID: 18224566.

14. Poultsides GA, Kim CJ, Orlando R 3rd, Peros G, Hallisey MJ, Vignati PV. Angiographic embolization for gastroduodenal hemorrhage: safety, efficacy, and predictors of outcome. Arch Surg. 2008; 143:457–461. PMID: 18490553.
15. Kim JH, Shin JH, Yoon HK, et al. Angiographically negative acute arterial upper and lower gastrointestinal bleeding: incidence, predictive factors, and clinical outcomes. Korean J Radiol. 2009; 10:384–390. PMID: 19568467.

16. Ichiro I, Shushi H, Akihiko I, Yasuhiko I, Yasuyuki Y. Empiric transcatheter arterial embolization for massive bleeding from duodenal ulcers: efficacy and complications. J Vasc Interv Radiol. 2011; 22:911–916. PMID: 21571546.

17. Loffroy R, Lin M, Thompson C, Harsha A, Rao P. A comparison of the results of arterial embolization for bleeding and non-bleeding gastroduodenal ulcers. Acta Radiol. 2011; 52:1076–1082. PMID: 22006986.

18. Schenker MP, Duszak R Jr, Soulen MC, et al. Upper gastrointestinal hemorrhage and transcatheter embolotherapy: clinical and technical factors impacting success and survival. J Vasc Interv Radiol. 2001; 12:1263–1271. PMID: 11698624.

19. Arrayeh E, Fidelman N, Gordon RL, et al. Transcatheter arterial embolization for upper gastrointestinal nonvariceal hemorrhage: is empiric embolization warranted? Cardiovasc Intervent Radiol. 2012; 35:1346–1354. PMID: 22302348.

20. Eriksson LG, Ljungdahl M, Sundbom M, Nyman R. Transcatheter arterial embolization versus surgery in the treatment of upper gastrointestinal bleeding after therapeutic endoscopy failure. J Vasc Interv Radiol. 2008; 19:1413–1418. PMID: 18755604.

21. Ripoll C, Bañares R, Beceiro I, et al. Comparison of transcatheter arterial embolization and surgery for treatment of bleeding peptic ulcer after endoscopic treatment failure. J Vasc Interv Radiol. 2004; 15:447–450. PMID: 15126653.

22. Ang D, Teo EK, Tan A, et al. A comparison of surgery versus transcatheter angiographic embolization in the treatment of nonvariceal upper gastrointestinal bleeding uncontrolled by endoscopy. Eur J Gastroenterol Hepatol. 2012; 24:929–938. PMID: 22617363.

23. Lang EK. Transcatheter embolization in management of hemorrhage from duodenal ulcer: long-term results and complications. Radiology. 1992; 182:703–707. PMID: 1535883.

Fig. 1
A 56-year-old man with pancreatic cancer with duodenal invasion. He had undergone biliary and duodenal stents and presented with hematemesis which was uncontrollable by endoscopy. (A, B) Superior mesenteric artery (SMA, arrows) angiograms show active massive bleeding (arrowheads) into the duodenum. (C) N-butyl-cyanoacrylate (NBCA) embolization (NBCA:lipiodol=1:2) was performed to control the bleeding. NBCA cast (arrows) is seen in the SMA. (D) Celiac angiogram shows no further bleeding through collaterals. There was collateral supply to the distal branches of the SMA on inferior mesenteric angiogram (not shown).
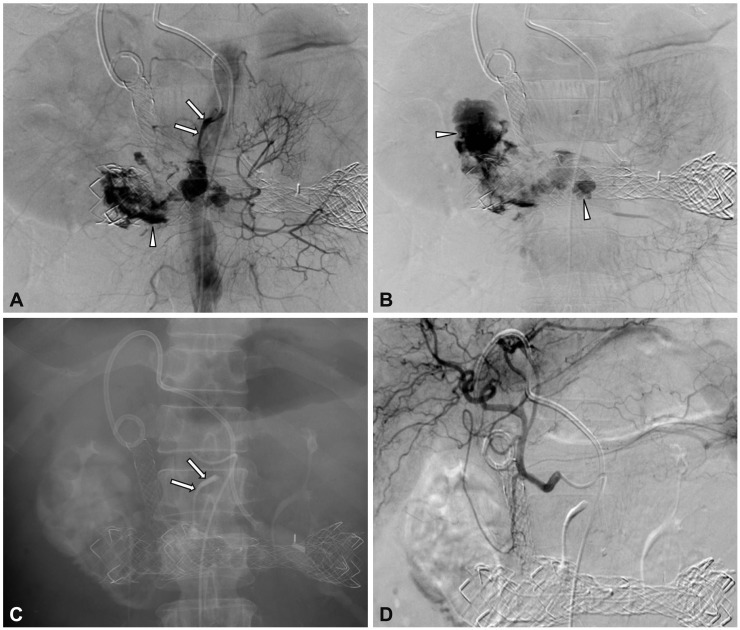
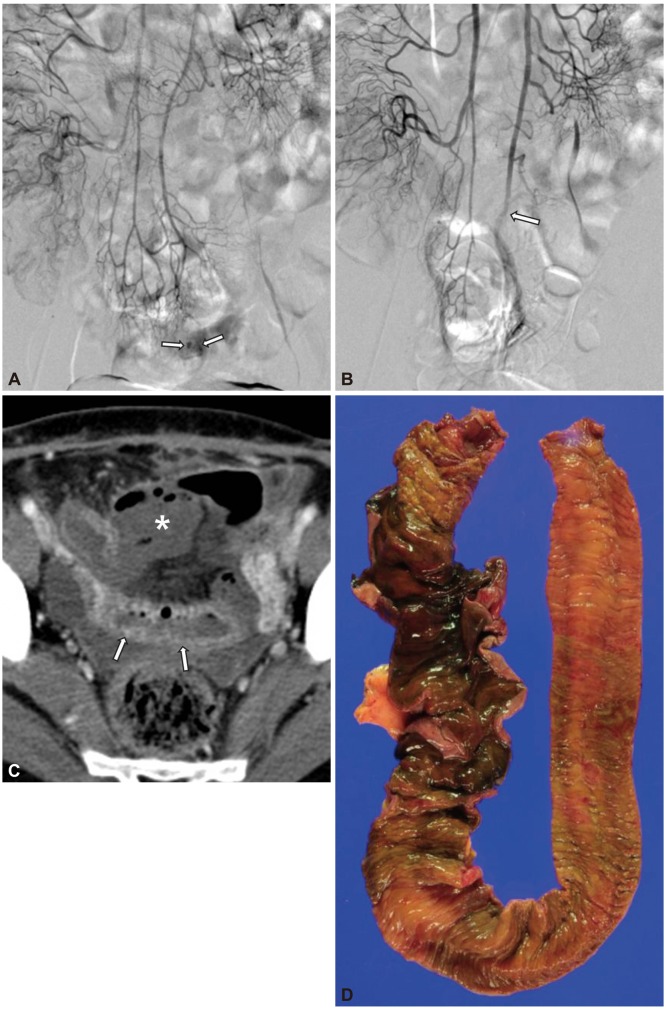
Fig. 2
A 56-year-old woman with ileal angiodysplasia. (A) Superior mesenteric artery (SMA) angiogram shows increased vascularity (arrows) of the ileum. There was early venous drainage on delayed image (not shown). (B) SMA angiogram after embolization with polyvinyl alcohol shows embolization at the proximal arc level (arrow). The ileal branches distal to the embolization level are not seen. (C) Computed tomography (CT) scan 2 days later shows bowel ischemic change (arrows) and complicated fluid collection (asterisk) with air, suggesting bowel perforation. (D) Exploration was done the next day after CT scans with resection of the ileal segment with transmural necrosis.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download