1. Barillari P, Aurello P, De Angelis R, et al. Management and survival of patients affected with obstructive colorectal cancer. Int Surg. 1992; 77:251–255. PMID:
1335999.
2. Phillips RK, Hittinger R, Fry JS, Fielding LP. Malignant large bowel obstruction. Br J Surg. 1985; 72:296–302. PMID:
3986481.

3. Deans GT, Krukowski ZH, Irwin ST. Malignant obstruction of the left colon. Br J Surg. 1994; 81:1270–1276. PMID:
7953385.

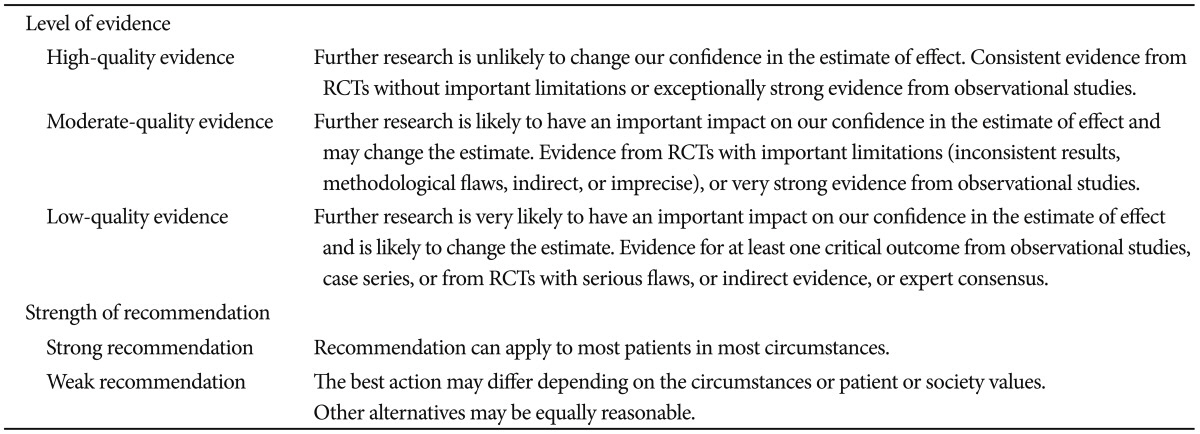
4. Guyatt GH, Cook DJ, Jaeschke R, Pauker SG, Schünemann HJ. Grades of recommendation for antithrombotic agents: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines (8th Edition). Chest. 2008; 133(6 Suppl):123S–131S. PMID:
18574262.
5. Schunemann HJ, Oxman AD, Brozek J, et al. Grading quality of evidence and strength of recommendations for diagnostic tests and strategies. BMJ. 2008; 336:1106–1110. PMID:
18483053.

6. Watt AM, Faragher IG, Griffin TT, Rieger NA, Maddern GJ. Self-expanding metallic stents for relieving malignant colorectal obstruction: a systematic review. Ann Surg. 2007; 246:24–30. PMID:
17592286.
7. Tilney HS, Lovegrove RE, Purkayastha S, et al. Comparison of colonic stenting and open surgery for malignant large bowel obstruction. Surg Endosc. 2007; 21:225–233. PMID:
17160651.

8. Cheung HY, Chung CC, Tsang WW, Wong JC, Yau KK, Li MK. Endolaparoscopic approach vs conventional open surgery in the treatment of obstructing left-sided colon cancer: a randomized controlled trial. Arch Surg. 2009; 144:1127–1132. PMID:
20026830.
9. Sagar J. Colorectal stents for the management of malignant colonic obstructions. Cochrane Database Syst Rev. 2011; (11):CD007378. PMID:
22071835.

10. Tan CJ, Dasari BV, Gardiner K. Systematic review and meta-analysis of randomized clinical trials of self-expanding metallic stents as a bridge to surgery versus emergency surgery for malignant left-sided large bowel obstruction. Br J Surg. 2012; 99:469–476. PMID:
22261931.
11. van Hooft JE, Bemelman WA, Breumelhof R, et al. Colonic stenting as bridge to surgery versus emergency surgery for management of acute left-sided malignant colonic obstruction: a multicenter randomized trial (Stent-in 2 study). BMC Surg. 2007; 7:12. PMID:
17608947.

12. Elsberger B, Rourke K, Brush J, Glancy S, Collie M. Self-expanding metallic stent insertion in the proximal colon. Colorectal Dis. 2008; 10:194–196. PMID:
17784867.

13. Repici A, Adler DG, Gibbs CM, Malesci A, Preatoni P, Baron TH. Stenting of the proximal colon in patients with malignant large bowel obstruction: techniques and outcomes. Gastrointest Endosc. 2007; 66:940–944. PMID:
17963881.

14. Dronamraju SS, Ramamurthy S, Kelly SB, Hayat M. Role of self-expanding metallic stents in the management of malignant obstruction of the proximal colon. Dis Colon Rectum. 2009; 52:1657–1661. PMID:
19690497.

15. Kim JS, Oh SY, Seo KU, et al. Comparison of effects of preoperative stenting for obstructing colorectal cancers according to the location of the obstructing lesion. Korean J Gastroenterol. 2009; 54:384–389. PMID:
20026893.

16. de Gregorio MA, Mainar A, Tejero E, et al. Acute colorectal obstruction: stent placement for palliative treatment: results of a multicenter study. Radiology. 1998; 209:117–120. PMID:
9769821.
17. Fernández Lobato R, Pinto I, Paul L, et al. Self-expanding prostheses as a palliative method in treating advanced colorectal cancer. Int Surg. 1999; 84:159–162. PMID:
10408289.
18. Liberman H, Adams DR, Blatchford GJ, Ternent CA, Christensen MA, Thorson AG. Clinical use of the self-expanding metallic stent in the management of colorectal cancer. Am J Surg. 2000; 180:407–411. PMID:
11182388.

19. Carne PW, Frye JN, Robertson GM, Frizelle FA. Stents or open operation for palliation of colorectal cancer: a retrospective, cohort study of perioperative outcome and long-term survival. Dis Colon Rectum. 2004; 47:1455–1461. PMID:
15486741.

20. Ptok H, Marusch F, Steinert R, Meyer L, Lippert H, Gastinger I. Incurable stenosing colorectal carcinoma: endoscopic stent implantation or palliative surgery? World J Surg. 2006; 30:1481–1487. PMID:
16850152.

21. Karoui M, Charachon A, Delbaldo C, et al. Stents for palliation of obstructive metastatic colon cancer: impact on management and chemotherapy administration. Arch Surg. 2007; 142:619–623. PMID:
17638798.
22. Cennamo V, Fuccio L, Mutri V, et al. Does stent placement for advanced colon cancer increase the risk of perforation during bevacizumab-based therapy? Clin Gastroenterol Hepatol. 2009; 7:1174–1176. PMID:
19631290.

23. Súarez J, Jiménez J, Vera R, et al. Stent or surgery for incurable obstructive colorectal cancer: an individualized decision. Int J Colorectal Dis. 2010; 25:91–96. PMID:
19859722.
24. Lee HJ, Hong SP, Cheon JH, et al. Long-term outcome of palliative therapy for malignant colorectal obstruction in patients with unresectable metastatic colorectal cancers: endoscopic stenting versus surgery. Gastrointest Endosc. 2011; 73:535–542. PMID:
21257165.

25. Yoon JY, Jung YS, Hong SP, Kim TI, Kim WH, Cheon JH. Clinical outcomes and risk factors for technical and clinical failures of self-expandable metal stent insertion for malignant colorectal obstruction. Gastrointest Endosc. 2011; 74:858–868. PMID:
21862005.

26. Jiménez-Pérez J, Casellas J, García-Cano J, et al. Colonic stenting as a bridge to surgery in malignant large-bowel obstruction: a report from two large multinational registries. Am J Gastroenterol. 2011; 106:2174–2180. PMID:
22085816.

27. Inaba Y, Arai Y, Yamaura H, et al. Phase II clinical study on stent therapy for unresectable malignant colorectal obstruction (JIVROSG-0206). Am J Clin Oncol. 2012; 35:73–76. PMID:
21293242.

28. Luigiano C, Ferrara F, Fabbri C, et al. Through-the-scope large diameter self-expanding metal stent placement as a safe and effective technique for palliation of malignant colorectal obstruction: a single center experience with a long-term follow-up. Scand J Gastroenterol. 2011; 46:591–596. PMID:
21271788.

29. Trompetas V, Saunders M, Gossage J, Anderson H. Shortcomings in colonic stenting to palliate large bowel obstruction from extracolonic malignancies. Int J Colorectal Dis. 2010; 25:851–854. PMID:
20390286.

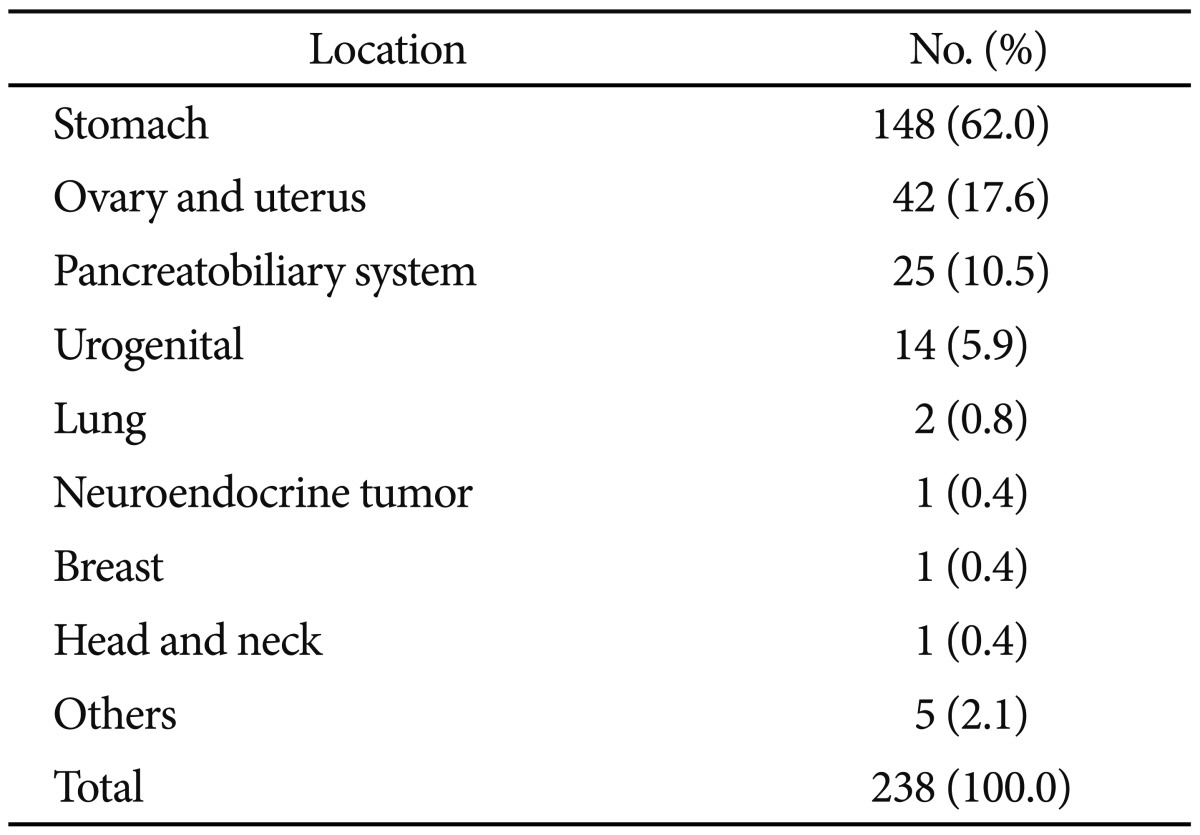
30. Shin SJ, Kim TI, Kim BC, Lee YC, Song SY, Kim WH. Clinical application of self-expandable metallic stent for treatment of colorectal obstruction caused by extrinsic invasive tumors. Dis Colon Rectum. 2008; 51:578–583. PMID:
18259816.
31. Caceres A, Zhou Q, Iasonos A, Gerdes H, Chi DS, Barakat RR. Colorectal stents for palliation of large-bowel obstructions in recurrent gynecologic cancer: an updated series. Gynecol Oncol. 2008; 108:482–485. PMID:
18190953.

32. Miyayama S, Matsui O, Kifune K, et al. Malignant colonic obstruction due to extrinsic tumor: palliative treatment with a self-expanding nitinol stent. AJR Am J Roentgenol. 2000; 175:1631–1637. PMID:
11090392.
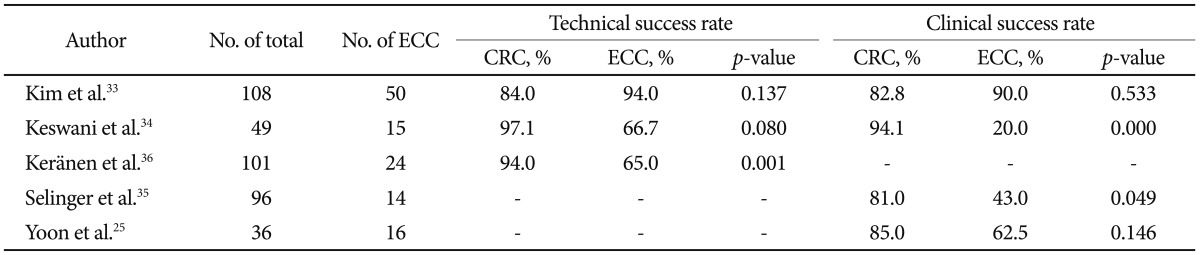
33. Kim JH, Song HY, Park JH, Ye BD, Yoon YS, Kim JC. Metallic stent placement in the palliative treatment of malignant colonic obstructions: primary colonic versus extracolonic malignancies. J Vasc Interv Radiol. 2011; 22:1727–1732. PMID:
21937243.

34. Keswani RN, Azar RR, Edmundowicz SA, et al. Stenting for malignant colonic obstruction: a comparison of efficacy and complications in colonic versus extracolonic malignancy. Gastrointest Endosc. 2009; 69(3 Pt 2):675–680. PMID:
19251009.

35. Selinger CP, Ramesh J, Martin DF. Long-term success of colonic stent insertion is influenced by indication but not by length of stent or site of obstruction. Int J Colorectal Dis. 2011; 26:215–218. PMID:
21207043.

36. Keränen I, Lepistö A, Udd M, Halttunen J, Kylänpää L. Stenting for malignant colorectal obstruction: a single-center experience with 101 patients. Surg Endosc. 2012; 26:423–430. PMID:
21909857.

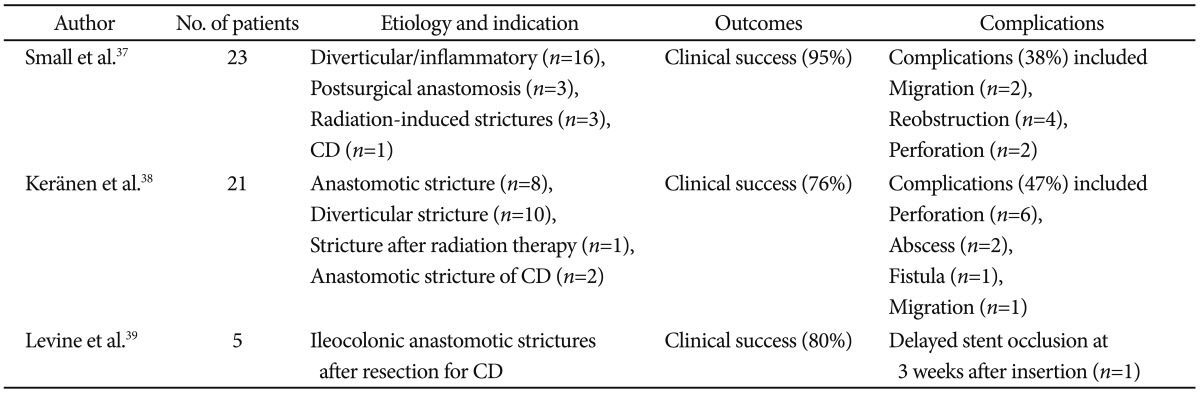
37. Small AJ, Young-Fadok TM, Baron TH. Expandable metal stent placement for benign colorectal obstruction: outcomes for 23 cases. Surg Endosc. 2008; 22:454–462. PMID:
17704890.

38. Keränen I, Lepistö A, Udd M, Halttunen J, Kylänpää L. Outcome of patients after endoluminal stent placement for benign colorectal obstruction. Scand J Gastroenterol. 2010; 45:725–731. PMID:
20205505.

39. Levine RA, Wasvary H, Kadro O. Endoprosthetic management of refractory ileocolonic anastomotic strictures after resection for Crohn's disease: report of nine-year follow-up and review of the literature. Inflamm Bowel Dis. 2012; 18:506–512. PMID:
21542067.

40. Stienecker K, Gleichmann D, Neumayer U, Glaser HJ, Tonus C. Long-term results of endoscopic balloon dilatation of lower gastrointestinal tract strictures in Crohn's disease: a prospective study. World J Gastroenterol. 2009; 15:2623–2627. PMID:
19496192.

41. Farrell JJ. Preoperative colonic stenting: how, when and why? Curr Opin Gastroenterol. 2007; 23:544–549. PMID:
17762561.

42. Keymling M. Colorectal stenting. Endoscopy. 2003; 35:234–238. PMID:
12584644.

43. Repici A, Pagano N, Hervoso CM, et al. Metal stents for malignant colorectal obstruction. Minim Invasive Ther Allied Technol. 2006; 15:331–338. PMID:
17190657.

44. Domingo S, Puértolas S, Gracia-Villa L, Puértolas JA. Mechanical comparative analysis of stents for colorectal obstruction. Minim Invasive Ther Allied Technol. 2007; 16:126–136. PMID:
17474056.

45. Repici A, De Caro G, Luigiano C, et al. WallFlex colonic stent placement for management of malignant colonic obstruction: a prospective study at two centers. Gastrointest Endosc. 2008; 67:77–84. PMID:
18155427.

46. Repici A, Fregonese D, Costamagna G, et al. Ultraflex precision colonic stent placement for palliation of malignant colonic obstruction: a prospective multicenter study. Gastrointest Endosc. 2007; 66:920–927. PMID:
17904133.

47. Fregonese D, Naspetti R, Ferrer S, et al. Ultraflex precision colonic stent placement as a bridge to surgery in patients with malignant colon obstruction. Gastrointest Endosc. 2008; 67:68–73. PMID:
18028916.

48. Small AJ, Baron TH. Comparison of Wallstent and Ultraflex stents for palliation of malignant left-sided colon obstruction: a retrospective, case-matched analysis. Gastrointest Endosc. 2008; 67:478–488. PMID:
18294511.
49. Kim JH, Song HY, Li YD, et al. Dual-design expandable colorectal stent for malignant colorectal obstruction: comparison of flared ends and bent ends. AJR Am J Roentgenol. 2009; 193:248–254. PMID:
19542421.

50. Shim CS, Cho JY, Jung IS, et al. Through-the-scope double colonic stenting in the management of inoperable proximal malignant colonic obstruction: a pilot study. Endoscopy. 2004; 36:426–431. PMID:
15100952.

51. Li YD, Cheng YS, Li MH, et al. Management of acute malignant colorectal obstruction with a novel self-expanding metallic stent as a bridge to surgery. Eur J Radiol. 2010; 73:566–571. PMID:
19167177.

52. Small AJ, Coelho-Prabhu N, Baron TH. Endoscopic placement of self-expandable metal stents for malignant colonic obstruction: long-term outcomes and complication factors. Gastrointest Endosc. 2010; 71:560–572. PMID:
20189515.

53. Song HY, Kim JH, Shin JH, et al. A dual-design expandable colorectal stent for malignant colorectal obstruction: results of a multicenter study. Endoscopy. 2007; 39:448–454. PMID:
17516352.

54. van Hooft JE, Fockens P, Marinelli AW, et al. Early closure of a multicenter randomized clinical trial of endoscopic stenting versus surgery for stage IV left-sided colorectal cancer. Endoscopy. 2008; 40:184–191. PMID:
18322873.

55. Jung MK, Park SY, Jeon SW, et al. Factors associated with the long-term outcome of a self-expandable colon stent used for palliation of malignant colorectal obstruction. Surg Endosc. 2010; 24:525–530. PMID:
19597776.

56. Park S, Cheon JH, Park JJ, et al. Comparison of efficacies between stents for malignant colorectal obstruction: a randomized, prospective study. Gastrointest Endosc. 2010; 72:304–310. PMID:
20561619.

57. Moon CM, Kim TI, Lee MS, et al. Comparison of a newly designed double-layered combination covered stent and D-weave uncovered stent for decompression of obstructive colorectal cancer: a prospective multicenter study. Dis Colon Rectum. 2010; 53:1190–1196. PMID:
20628284.

58. Choi JS, Choo SW, Park KB, et al. Interventional management of malignant colorectal obstruction: use of covered and uncovered stents. Korean J Radiol. 2007; 8:57–63. PMID:
17277564.

59. Lee KM, Shin SJ, Hwang JC, et al. Comparison of uncovered stent with covered stent for treatment of malignant colorectal obstruction. Gastrointest Endosc. 2007; 66:931–936. PMID:
17767930.

60. Langevin JM, Nivatvongs S. The true incidence of synchronous cancer of the large bowel. A prospective study. Am J Surg. 1984; 147:330–333. PMID:
6703204.
61. Slater G, Aufses AH Jr, Szporn A. Synchronous carcinoma of the colon and rectum. Surg Gynecol Obstet. 1990; 171:283–287. PMID:
2218832.
62. Ekelund GR, Pihl B. Mutiple carcinomas of the colon and rectum. Cancer. 1974; 33:1630–1634. PMID:
4834157.
63. Adloff M, Arnaud JP, Bergamaschi R, Schloegel M. Synchronous carcinoma of the colon and rectum: prognostic and therapeutic implications. Am J Surg. 1989; 157:299–302. PMID:
2537586.

64. Pagana TJ, Ledesma EJ, Mittelman A, Nava HR. The use of colonoscopy in the study of synchronous colorectal neoplasms. Cancer. 1984; 53:356–359. PMID:
6690019.

65. Vitale MA, Villotti G, d'Alba L, Frontespezi S, Iacopini F, Iacopini G. Preoperative colonoscopy after self-expandable metallic stent placement in patients with acute neoplastic colon obstruction. Gastrointest Endosc. 2006; 63:814–819. PMID:
16650544.

66. Cha EY, Park SH, Lee SS, et al. CT colonography after metallic stent placement for acute malignant colonic obstruction. Radiology. 2010; 254:774–782. PMID:
20177092.

67. Datye A, Hersh J. Colonic perforation after stent placement for malignant colorectal obstruction: causes and contributing factors. Minim Invasive Ther Allied Technol. 2011; 20:133–140. PMID:
20929424.
68. Donnellan F, Cullen G, Cagney D, et al. Efficacy and safety of colonic stenting for malignant disease in the elderly. Int J Colorectal Dis. 2010; 25:747–750. PMID:
20213457.

69. Sagar J. Colorectal stents for the management of malignant colonic obstructions. Cochrane Database Syst Rev. 2011; (11):CD007378. PMID:
22071835.

70. Lopera JE, De Gregorio MA. Fluoroscopic management of complications after colorectal stent placement. Gut Liver. 2010; 4(Suppl 1):S9–S18. PMID:
21103302.

71. Repici A, de Paula Pessoa Ferreira D. Expandable metal stents for malignant colorectal strictures. Gastrointest Endosc Clin N Am. 2011; 21:511–533. PMID:
21684468.

72. Suh JP, Kim SW, Cho YK, et al. Effectiveness of stent placement for palliative treatment in malignant colorectal obstruction and predictive factors for stent occlusion. Surg Endosc. 2010; 24:400–406. PMID:
19551432.

73. Park JK, Lee MS, Ko BM, et al. Outcome of palliative self-expanding metal stent placement in malignant colorectal obstruction according to stent type and manufacturer. Surg Endosc. 2011; 25:1293–1299. PMID:
20976501.

74. Branger F, Thibaudeau E, Mucci-Hennekinne S, et al. Management of acute malignant large-bowel obstruction with self-expanding metal stent. Int J Colorectal Dis. 2010; 25:1481–1485. PMID:
20607252.

75. Fernández-Esparrach G, Bordas JM, Giráldez MD, et al. Severe complications limit long-term clinical success of self-expanding metal stents in patients with obstructive colorectal cancer. Am J Gastroenterol. 2010; 105:1087–1093. PMID:
19935785.

76. Baron TH. Colonic stenting: technique, technology, and outcomes for malignant and benign disease. Gastrointest Endosc Clin N Am. 2005; 15:757–771. PMID:
16278137.

77. Park JH, Oh SH, Lee WY, Choo SW, Do YS, Chun HK. Flexible rectal stent for obstructing colonic neoplasms. J Korean Soc Coloproctol. 2000; 16:267–273.
78. Song HY, Kim JH, Kim KR, et al. Malignant rectal obstruction within 5 cm of the anal verge: is there a role for expandable metallic stent placement? Gastrointest Endosc. 2008; 68:713–720. PMID:
18561924.

79. Rao VS, Al-Mukhtar A, Rayan F, Stojkovic S, Moore PJ, Ahmad SM. Endoscopic laser ablation of advanced rectal carcinoma: a DGH experience. Colorectal Dis. 2005; 7:58–60. PMID:
15606586.
80. Courtney ED, Raja A, Leicester RJ. Eight years experience of high-powered endoscopic diode laser therapy for palliation of colorectal carcinoma. Dis Colon Rectum. 2005; 48:845–850. PMID:
15747077.

81. Eickhoff A, Jakobs R, Schilling D, et al. Prospective nonrandomized comparison of two modes of argon beamer (APC) tumor desobstruction: effectiveness of the new pulsed APC versus forced APC. Endoscopy. 2007; 39:637–642. PMID:
17611919.

82. Horiuchi A, Nakayama Y, Tanaka N, et al. Acute colorectal obstruction treated by means of transanal drainage tube: effectiveness before surgery and stenting. Am J Gastroenterol. 2005; 100:2765–2770. PMID:
16393233.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download