Abstract
Endoscopic stents have evolved dramatically over the past 20 years. With the introduction of uncovered self-expanding metal stents in the early 1990s, they are primarily used to palliate symptoms of malignant obstruction in patients with inoperable gastrointestinal (GI) cancer. At present, stents have emerged as an effective, safe, and less invasive alternative for the treatment of malignant GI obstruction. Clinical decisions about stent placement should be made based on the exact understanding of the patient's condition. These recommendations based on a critical review of the available data and expert consensus are made for the purpose of providing endoscopists with information about stent placement. These can be helpful for management of patients with inoperable cancer or various nonmalignant conditions in the upper GI tract.
This report presents the evidence-based recommendations for upper gastrointestinal tract (UGIT) stenting for benign and malignant conditions. It includes the current view of the Korean Society of Gastrointestinal Endoscopy on endoscopic UGIT stenting and describes the associated indications, outcomes, models of available stents and UGIT stenting techniques. Gastrointestinal (GI) stents have been developed for palliation of obstructive symptoms in patients with inoperable GI cancer. The role of stents in the UGIT is to relieve dysphagia, maintain oral intake, prevent aspiration, and improve quality of life. Considering that GI stent placement is emerging as a first-line modality for palliative care, it is very important to establish recommendations for the role of stents in UGIT in Korea.
This work began in June 2011 with the formation of the UGIT stenting working group. The working group consisted of five gastroenterologists who are active in clinical practice and research field of UGIT stenting. All these physicians are the members of the Stent Study Group of the Korean Society of Gastrointestinal Endoscopy. No participant declared a conflict of interest. The Korean Society of Gastrointestinal Endoscopy supported this work. The aim of this article is to help gastroenterologists make decisions in management of patients with UGIT lesion.
This report will be published in the official journal of the Korean Society of Gastrointestinal Endoscopy and will be provided free of charge on the website of the Korean Society of Gastrointestinal Endoscopy. The contents will be widely distributed through a summary book. Moreover, the contents will be periodically revised to reflect the latest knowledge.
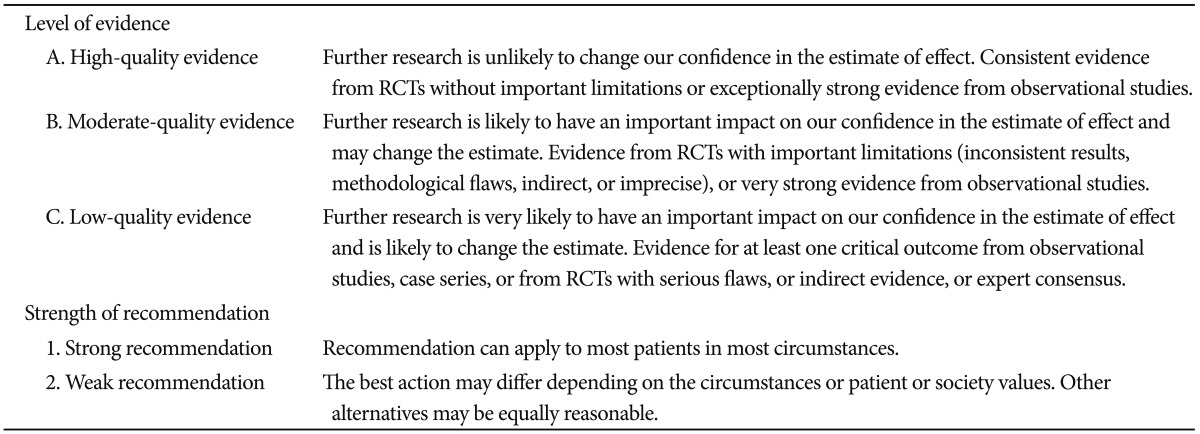
A literature search was conducted using the PubMed, Embase, KoreaMed, and the Cochrane Library databases to identify relevant articles published from January 2001 to June 2012. Keywords used in search of literature included "esophageal cancer, esophageal obstruction, esophageal malignant stricture, gastric outlet obstruction, and stents." The articles were included if they met the following criteria: 1) the manuscript was written in English or Korean; 2) the full manuscript was available; and 3) the study participants were older than 18 years of age. Five members of the working group performed the searches and summarized the data using standardized report forms. Subsequently, 17 key questions were identified and distributed to each member of the working group. Based on the relevant literature articles, the working group members rated the level of evidence and created the draft statements. The level of evidence and the strength of recommendation were defined and graded (Table 1).1 The working group members checked and revised the draft statements and their ratings after further review and discussion. On the basis of the modified Delphi process, the draft statements were circulated electronically to all participants prior to the face-to-face meeting. The first voting on the statements was conducted by email. Each statement was assessed on a 5-point Likert scale as follows: 1) accept completely; 2) accept with some reservation; 3) accept with major reservation; 4) reject with reservation; and 5) reject completely. Based on the voting results and comments, the statements were modified. The second voting was carried out during the face-to-face meeting, followed by the modification of the statement when the proportion of the working group answering 1 plus those answering 2 was <75%. Subsequently, participants voted again on the statement. When the proportion of the working group answering 1 plus those answering 2 was ≥75%, the statement was finally accepted. Korean Society of Gastrointestinal Endoscopy provided funding and any industrial influence on the process of consensus development was avoided. The funding source had no role in identifying statements, abstracting data, grading evidence, or preparing the manuscript. This manuscript was reviewed by the external reviewers (K.S.P. from the Department of Internal Medicine, Keimyung University School of Medicine, Y.J.J. from Department of Internal Medicine, Eulji Medical Center, Eulji University School of Medicine) prior to submission to Clinical Endoscopy and was approved by the Korean Society of Gastrointestinal Endoscopy.
Stent placement is the first-line treatment for palliation of dysphagia caused by esophageal or proximal gastric cancers (agreement, 100%; 1A, strong recommendation, high-quality evidence).
In two randomized controlled studies, chemotherapy showed no survival benefit in patients with metastatic carcinoma of the esophagus, compared with supportive care.2 For palliative care in patients with unresectable esophageal cancer, current treatment options include thermal ablation, photodynamic therapy, radiotherapy, chemotherapy, chemical injection, electrocoagulation, and stenting, with different success and complications rates. Endoscopic stent placement compares favorably to other techniques since it provides immediate and potentially long-lasting relief of obstructive symptoms.3,4 Self-expanding metal stents (SEMSs) placement is indicated for the palliation of obstructive symptoms due to esophageal cancer and extraluminal compression of the esophagus (e.g., from a lung tumor). SEMSs are superior to self-expandable plastic stents (SEPSs) in the management of obstruction caused by unresectable esophageal cancers as the use of SEPS is associated with significantly higher complications and more technical difficulties than SEMS.5-7
Covered SEMSs are superior to uncovered SEMSs to relieve the symptom of dysphagia in patients with unresectable esophageal cancer (agreement, 82%; 1B, strong recommendation, moderate-quality evidence).
According to results of several studies, partially or fully covered stents showed better long-term palliation of dysphagia than uncovered stents in patients with unresectable esophageal cancer.8-10 Epithelialization of uncovered stents occurs within 3 to 6 weeks and the risk of migration decreases afterward.11 Uncovered stents are more flexible and easier to deliver and deploy, but they are subject to tumor ingrowth through the open mesh of the stent.12 In contrast, covered SEMSs resist tumor ingrowth and therefore prevent restenosis. However, they are less stable and more rigid, requiring larger delivery systems, and they are more prone to migration.10 Recently, several covered stents with antimigration property were developed. They are designed to prevent migration with a partial cover or flared ends, or a double stent design.10,12 These newer covered stent designs are either partially covered in the middle with uncovered bare ends or are fully covered and have an extra outer self-expanding bare nitinol layer in the middle (double-covered Niti-S; Taewoong Medical, Seoul, Korea) to allow epithelialization or tumor ingrowth for effective anchoring in the esophageal wall.
At present, covered SEMSs are considered the first treatment modality for palliation of malignant esophageal stricture. In a multicenter trial by Vakil et al.,8 62 patients with inoperable gastroesophageal (GE) junction tumors were randomized to partially covered or uncovered SEMSs with the same design. Both types showed similar relief of dysphagia and stent migration rate; however, there was significant difference in the recurrence of obstruction and reintervention rate. After initial stenting, obstruction caused by tumor ingrowth occurs more frequently in the uncovered stents group (30%) than in the covered stents group (3%). Reintervention rate was higher in the uncovered stents group (27%) than in the covered stents group (0%). In a retrospective study, the efficacy of GI stenting was evaluated in 152 patients with inoperable malignant stricture of the esophagus and cardia. The proportion of patients with symptom relief during follow-up was significantly higher in partially covered stents group (88%) than in uncovered stents group (54%).10 Although stent migration rate was lower, recurrent dysphagia occurred more frequently in the uncovered stents group. In a recent prospective randomized trial, overall complication rate was significantly lower in the group using Niti-S double-layered covered stent with antimigration property (12%), in comparison with conventional covered stents group (58%).13
In a recent study comparing partially covered metal stents to fully covered metal and plastic stents, there was no difference in the improvement of dysphagia and overall complications between the two groups.14 However, the rate of recurrent dysphagia was higher in patients with partially covered Ultraflex stent (52%) than fully covered Niti-S stent (31%). Because only a few studies were conducted, the outcomes of partially covered SEMSs remain to be determined. On the basis of these data, covered and new double-layered covered SEMSs are preferred for the palliation of malignant dysphagia due to unresectable esophageal cancer. Instead, uncovered SEMSs can be considered in specific cases, such as extrinsic esophageal compression, severe dilated esophagus to avoid food entrapment between the proximal stent and the esophagus and recurrence after gastric pull-up surgery.15
Despite some differences in efficacy and complication rates among various SEMSs, the overall efficacy and complication rates among the currently available SEMSs are comparable (agreement, 82%; 1B, strong recommendation, moderate-quality evidence).
There are several studies that have compared stent types according to the manufacturing companies. In a study, 100 patients with inoperable esophageal or gastric cardiac cancer were randomized to one of three types of covered metal stents: the Ultraflex stent, the Flamingo Wallstent, and the Z-stent.16 There were no significant differences in the improvement of dysphagia, the overall complication rates or the recurrence of dysphagia. However, Z-stent showed higher frequency of overall complications. In another prospective trial, the Ultraflex stent and the Flamingo Wallstent were compared in patients with distal esophageal cancer.10 There were no significant differences in the improvement of dysphagia and complication rates between them. In a retrospective study, 87 patients with malignant esophageal strictures were enrolled. Three types of stents (uncovered Ultraflex, covered and uncovered versions of the Wallstent, and the covered Z-stent) were used, respectively.17 There were no differences in clinical outcomes and complication rates among them.
On the basis of the above studies, there were no significant differences in the same types of stent, manufactured by different companies. Therefore, stent can be selected by the location and anatomy of the malignant esophageal stricture within the same types of SEMS.18
Common complications after stent placement in esophageal cancer are perforation, migration, and tumor overgrowth. Aspiration pneumonia, esophago-tracheal fistula and chest pain can occur (agreement, 100%; 1A, strong recommendation, high-quality evidence).
When placing a stent in esophageal malignancies, related complications are various. These depend on the location of tumor,19-21 the presence of a fistula or tumor shelf,22-24 history of concomitant chemoirradiation,25 tumor vascularity.26 The characteristics of stents, including diameter and design, also affect the complication rate.6,8,10,16,26-33 Complications include postprocedural perforation, sustained dysphagia due to inadequate stent expansion, throat or chest pain, stent migration, esophageal erosions with bleeding or fistula formation. When stent is placed across the GE junction, significant reflux can occur. Patients with uncovered stents might complain of recurrent dysphagia, because of stent obstruction by tumor ingrowth or granulation tissue formation. In most cases, complication rate was 30% to 35% and it increased during follow-up. Complications also seem to be higher with SEPS (Polyflex).27,34 If European Z stents with midshaft barbs are placed across the GE junction, reflux symptoms mostly develop in patients who underwent concomitant irradiation.16,25,35-38 In a retrospective review, 338 patients with esophageal or gastric cardia cancer were treated by one of three types of SEMSs, such as Ultraflex (n=153), Gianturco Z stent (n=89), and Flamingo Wallstent (n=96).32 Small and large diameter stents were used in 265 and 73 patients, respectively. Both types were comparable in relief of dysphagia. There was an increased risk of major complications (hemorrhage, perforation, fistula, and fever) in patients with large diameter Gianturco Z stents, compared with smaller diameter stents of the same type (40% vs. 20% complication rate; adjusted hazard ratio [HR], 5.03; 95% confidence interval [CI], 1.33 to 19.11). In Ultraflex and Flamingo Wallstent, there was no difference in major complication rate according to the size of stent diameter. However, recurrent dysphagia due to food impaction, tissue overgrowth, and stent migration occurred more frequently in patients with small diameter stents than in those with large-diameter stents (Ultraflex 42% vs. 13%; HR, 0.16; 95% CI, 0.04 to 0.74) (Gianturco Z stent 27% vs. 10%; HR, 0.97; 95% CI, 0.11 to 8.67) (Flamingo Wallstent 37% vs. 15%; HR, 0.4; 95% CI, 0.03 to 4.79). In a recent study by Homann et al.,26 71 of 133 patients (53.4%) experienced delayed complications including recurrent dysphagia due to tumor ingrowth (22%), food impaction (21%), tumor overgrowth (15%), stent migration (9%), and esophago-airway fistulas (9%). The patients with reintervention had a significantly longer life expectancy (222±26 days vs. 86±14 days, p<0.001) than those without it. In another retrospective study of 97 patients with SEMS placement, dysphagia improved in 86% and tracheoesophageal fistula symptoms in 90% of the patients.39 Major complications (hematemesis, severe emesis, stent migration, tumor overgrowth, new stricture formation, food impaction, procedure-related death) occurred in 37%. These were significantly more common in females (p=0.008) and in patients with adenocarcinoma (p=0.03). Minor complications (pain, nausea, vomiting, and reflux) were noted in 47% of the patients.
Placement of covered SEMS is effective for the palliation of malignant tracheo-esophageal fistula (agreement, 92%; 1B, strong recommendation, moderate-quality evidence).
Malignant esophageal fistulas usually develop because of the cancerous infiltration into the respiratory tract (trachea or bronchi). Fistula formation rarely occurs between the esophagus and aorta, mediastinum, or pleura. In many case series, SEMSs were used for the closure of esophago-airway fistula. They have reported that technical success rate and complication rate were 70% to 100% and 10% to 30%, respectively.23,40-48 In a large series by Shin et al.,24 SEMS placements were performed in 61 patients with esophago-respiratory fistulas and 49 patients (80%) had successful closure of the fistula, although 10 patients also required additional airway prostheses. During follow-up, a third of the patients experienced recurrence of fistulas. Of these, eight patients received successful retreatment with SEMSs. The mean duration of overall survival was 3 months (range, 1 to 56 weeks). It was significantly longer in patients with complete fistula closure, compared with those with incomplete closure (15.1 weeks vs. 6.2 weeks, p<0.05). Therefore, endoscopic placement of covered SEMSs is the treatment of choice for malignant esophageal fistulas.
The use of SEMSs with antireflux valve for reducing GE reflux cannot be routinely recommended in the treatment of malignant dysphagia due to distal esophagus and gastric cardia cancer (agreement, 75%; 2C, weak recommendation, low-quality evidence).
There are conflicting data about usefulness of antireflux SEMS across the GE junction. Dua et al.35 demonstrated that modified Z stent could prevent reflux in patients with GE junction malignancy after stent placement. A randomized, controlled trial (RCT) by Laasch et al.36 showed similar results. Three of 25 patients (12%) with the antireflux Z stents had significant reflux, compared to 24 of 25 patients (96%) with a standard open Flamingo Wallstent (p<0.001). There were no differences in the degree of dysphagia improvement or complications between the two groups. Power et al.49 reported that antireflux stents could relieve reflux symptoms in relation to DeMeester score in 24 patients. Both standard and antireflux stents provided comparable relief from dysphagia and improved quality of life in patients. Several studies also have demonstrated the usefulness of stents with antireflux valve. Lee et al.50 demonstrated that acid and bile reflux into the esophagus were not detected in patients after placement with an antireflux SEMS. Davies et al.51 reported that antireflux Z stent can prevent gastroesophagel reflux. In a study by Shim et al.,37 36 patients with cancer at the GE junction were randomized to one of three types of stents: Hanarostent (MI Tech Co., Ltd., Incheon, Korea) with a S-shaped antireflux valve, Dostent (MI Tech Co., Ltd.) with a tricuspid antireflux valve, or a standard open SEMS. The fraction of the total recording time during which esophageal pH was <4 was 3%, using the Hanarostent, compared to 29% with the Dostent and 15% with the standard open SEMSs (p<0.001). However, these promising results were not reproduced in other studies. A RCT by Wenger et al.52 compared an antireflux stent with a standard open SEMS in 41 patients with inoperable distal esophageal or cardia cancers. There were no significant differences in esophageal reflux symptoms between the two groups. In another study including 30 patients, stents with a windsock-type antireflux valve (FerX-Ella; ELLA-CS, Hradec Kralove, Czech Republic) (n=15) were compared with standard open SEMSs without valve (n=15).22 Two weeks after stent placement, GE reflux symptoms were assessed by standardized questionnaire and 24-hour pH monitoring. Reflux symptoms were reported more frequently in patients treated with an antireflux stent (25%) compared to the patients with an open stent (14%). Paradoxically, the patients with antireflux stent showed increased esophageal acid exposure in 24-hour pH monitoring. In a meta-analysis by Sgourakis et al.,53 there was no difference between the antireflux stents and conventional stents in the relief of reflux symptoms. According to these conflicting results, the routine use of SEMSs with antireflux valve cannot be recommended in the management of malignant dysphagia due to distal esophageal and gastric cardia malignancy.
If newly designed SEMS is considered on the basis of the distance to upper esophageal sphincter, the patient's tolerance and respiratory status, it can be a good treatment modality in the palliation of dysphagia due to proximal esophageal malignancy (agreement, 75%; 1C, strong recommendation, low-quality evidence).
In the upper esophagus, use of stents may be limited due to patient intolerance, pain, globus sensation, increased risk of tracheoesophageal fistula, and aspiration pneumonia. Several retrospective series have demonstrated the feasibility of proximal esophageal stent placement for the palliative care.19,20,54 The largest retrospective one reviewed the clinical outcomes of 104 patients with a malignant stricture within 8 cm of the upper esophageal sphincter.54 Of these, 24 patients (23%) also had a tracheoesophageal fistula. The procedure was successfully performed in 96% of patients, and the dysphagia score improved from a mean of 3 to 1. Fistula closure was achieved in 79% (19/24 patients). Overall complications were noted in a third of the patients, including major complications in 21%. Recurrent dysphagia occurred in 28% (29/104) and the main causes were tissue ingrowth or overgrowth (n=10), food bolus obstruction (n=7), stent migration (n=3), persistent fistula (n=5), swallowing difficulty (n=4), and partial collapse of the upper rim of the stent (n=2). Although transient postprocedural pain was common, persistent globus sensation was noted in only 8% of the patients. However, no patients required stent retrieval. In a small series, the use of modified nitinol prostheses (Niti-S stent) showed similar results.21 During the stent placement, 2-cm distance should be maintained below the upper esophageal sphincter.
In selected cases, SEMSs and SEPSs can be considered in the treatment of esophageal perforation, leaks, and fistulas (agreement, 100%; 2C, weak recommendation, low-quality evidence).
Spontaneous or iatrogenic esophageal perforations, fistula and disruption of esophageal anastomosis are potentially life-threatening events that are associated with high morbidity and mortality rates.55-57 Successful management of perforations depends on early diagnosis and prompt intervention to prevent fulminant mediastinitis. The classic surgical treatments include repair, esophagectomy, or cervical exclusion along with clearance of mediastinal and peritoneal contamination, infection, and inflammation by successful drainage. Although surgical techniques are developed, the mortality rate remains high.58 Primary closure and mediastinal drainage within 24 hours of the injury were required to increase survival rate.59 In a delayed diagnosis and management, the patients could not avoid high morbidity and mortality, because of mediastinal and pleural contamination. In elderly and debilitated patients, anastomotic disruption after esophagectomy is associated with poor outcome. Surgical mortality is similar to that of conservative management in these patients.60
In recent years, esophageal stents have been introduced as a promising management of these conditions. The stent placement can be performed using only endoscopy in high risk patients for operation. However, the experience of stent placement in these situations is limited to case reports and case series. The use of esophageal stents in the management of spontaneous esophageal perforations (Boerhaave syndrome) has been described in several case reports.61-64 Results were various and complications included bleeding, stent-related strictures, tissue ingrowth, fistula formation, and migration. In a case series, three patients with Boerhaave syndrome were treated with SEMS (Song and Niti-S stents) and had favorable outcomes. Stents were placed between 4 and 30 days of the event and removed 2 to 6 months later.63 A similar result was seen in a patient with Boerhaave syndrome who underwent SEPS placement.64 Esophageal stent placements were also reported in the management of perforations secondary to endoscopic therapies such as esophageal dilation, tumor resection, or external blunt and sharp trauma. The favorable outcomes were associated with the perforation area of less than 50% to 70% in circumference. In one case series, 11 consecutive patients were presented as traumatic nonmalignant esophageal perforations. Diagnosis was delayed by >24 hours and they were managed by SEMS placement. Pleural cavities were drained with thoracostomy drains and antibiotics were administered. Stents were placed at a median time of 60 hours after the onset of symptoms. The stents completely sealed off the perforation in nine of 11 patients, whereas two patients still required esophagectomy because of inadequate closure of perforation and incomplete drainage. In seven patients, the stents were retrieved endoscopically.65 In another case series, three patients with iatrogenic esophageal perforations experienced successful closure using SEMSs. However, stent migration was reported in all three cases and esophageal stricture occurred in one case.66 In another prospective study, partially covered SEMSs were used in 22 patients with esophageal perforations or rupture (13 benign etiologies). Successful closure was achieved in 12 of 13 benign cases, and all stents were retrieved without complications after 3 weeks.67 In a recent retrospective study, 15 patients were treated with SEMSs due to benign spontaneous or iatrogenic esophageal perforations. One group underwent stent placement promptly (group 1, mean time, 45 minutes) and the other group received delayed management (group 2, mean time, 123 hours). Treatment was successful in all patients in group 1. In contrast, one patient in group 2 died of pneumonia and the remaining patients experienced long-term hospitalization due to sepsis and multiorgan failure. Immediate stent placement showed an excellent outcome with minimal morbidity, and management of esophageal perforation using SEMS was comparable to surgery.68
Recently, placement of SEPSs has also been adopted in the management of esophageal perforations.69-72 A prospective case series reported the use of SEPSs in 17 patients with iatrogenic esophageal perforation at a tertiary care medical center. Esophagogram confirmed leak occlusion in 16 patients (94%), and stent migration occurred in three patients (17.6%).72 A case series using SEMSs reported clinical success in three patients with postoperative anastomotic leaks.73 Similarly, another recent case series described the management of six patients with postoperative anastomotic leaks using SEMSs. Leaks were successfully closed in all patients and oral feeding was resumed 2 days after the procedure. Stent migration was observed in two patients.74 A case series reported the usefulness of SEMSs in patients (n=12) with acquired benign tracheoesophageal fistulas. They were ventilated mechanically and fistula occlusion was successfully achieved in all cases after stent placement. No stent migration was reported and fistulas remained sealed off until patient's death or stent removal. Nine patients died of the underlying disease and three patients were referred for additional surgery, before which the stents were removed easily.75 In a case series including 19 patients with anastomotic leaks after esophagectomy, the initial 10 patients underwent re-exploration or conservative management, and following nine patients received the placement of a large-diameter SEPS a median of 8 days after operation. Leak occlusion was achieved in eight of nine patients (89%). The mean time until stent removal was 4 weeks and the patients receiving stent placement experienced earlier oral intake and shorter hospital stay.76 In another study, SEPSs were placed in nine patients with anastomotic leaks after esophageal resection or perforation. The leaks were completely closed in seven of nine patients (78%). Stent migration was observed in 33% of the cases.77 In another study, 24 patients with esophageal anastomotic leaks underwent SEPS placement. Stent placement was successful in 22 of 24 patients and clinical success was achieved in 16 of 22 patients (72%).78 Finally, in a case series of 12 patients with esophageal anastomotic leaks, large-diameter SEPS was used along with perianastomotic mediastinal drainage. Complete closure of the leakage was achieved in 11 of 12 patients (91.6%).79 The management strategy was suggested according to areas of leak in circumference. In patients with small leaks (<30% of circumference), endoscopic fibrin glue injection or clipping can be used. In patients with 30% to 70% circumferential dehiscence, stent placement can be considered. In patients with >70% dehiscence, surgery is recommended. However, prospective trials are needed to confirm these recommendations in the future.
SEMS cannot be routinely recommended for benign esophageal stricture due to high complication rates and it should only be used in selected patients. The use of full covered, retrievable SEMS has shown some efficacy for the management of benign esophageal stricture and its removal is relatively safe. However, long-term controlled trials are needed to confirm its safety and feasibility (agreement, 100%; 2C, weak recommendation, low-quality evidence).
Although SEMS might have several theoretical advantages in patients with refractory benign esophageal strictures, permanent placement of stent was not yet recommended. All studies about the role of SEMS in benign esophageal strictures are limited to retrospective case series and case reports.80-91 In management of benign esophageal stricture, the use of SEMSs caused significant complications, such as bleeding, frequent stent migration, fistula, and recurrent stricture.80-85 After placement, hyperplastic tissue growth is possible in uncovered portion and both ends of the stent. It may be related to the mechanical radial force of the stent on the esophageal wall, the type of metal used in the stent, the size of stent and the duration of stenting.92 Because hyperplastic tissue growth prevents the stent removal, the use of SEMS is limited.
Recently, temporary placement of retrievable, full covered SEMS has become a new modality for the treatment of refractory benign esophageal strictures. In an earlier study of 25 patients, the stent was electively removed at 8 weeks in only five patients (20%). In the remaining 18 patients, the stent removal was performed 1 to 8 weeks (mean, 3 weeks) after placement because of complications. New stricture formation was seen in 12 patients (48%) and a small esophago-bronchial fistula developed in one patient.90 A recent study also presented disappointing results.93 During a mean follow-up period of 38 months, only 31% of patients had long-term relief of obstructive symptoms. The common complications were granulation tissue formation (31%), stent-related chest pain (24%), and stent migration (25%). Several studies demonstrated that long-term success of SEMS treatment was associated with short length of stricture and etiology of stricture. In patients with radiation-induced strictures, clinical outcomes were better than in peptic or postoperative anastomotic strictures.81,90 Also, the use of smaller diameter of stent could reduce the rate of new stricture formation.91
Therefore, the routine use of SEMS should not be recommended in patients with benign esophageal strictures. Until further long-term data are obtained from controlled trials, it should only be used in carefully selected patients.
SEPS cannot be routinely recommended in treatment of refractory benign esophageal stricture due to high complication rates (agreement, 92%; 2C, weak recommendation, low-quality evidence).
As mentioned earlier, SEMS showed discouraging results and high incidence of new stricture due to hyperplastic tissue growth. Therefore, SEPS were introduced for the management of benign esophageal stricture. There are several advantages of SEPSs over SEMSs in the treatment of benign esophageal lesions, including the easier retrieval of stent, less local tissue reaction, and possibly lower costs.94-98 The completely covered Polyflex stent are made of silicone and polyester to prevent recurrence due to hyperplastic tissue ingrowth.99
Most studies have reported high success rates in SEPS placement with immediate improvement in dysphagia (26% to 40%). In published data, overall success rates of SEPSs ranged from 17% to 95%. SEPS-related complications were similar to those in SEMSs.33 Early complications were aspiration, airway disturbance, stent malposition, stent-related chest pain, bleeding, and perforation. Late complications were stricture recurrence or new stricture formation, fistula, esophageal ulceration, bleeding, GE reflux, food impaction, and stent migration. After placement of Polyflex stent, incidence of new stricture formation was lower than that in SEMS.71,95-101 This outcome implies that decrease in hyperplastic tissue reaction may result from less expandable radial force of material in Polyflex stent. However, the migration rate of SEPSs seems to be higher than that of SEMS, ranging from 7% to 100% according to the reported literature.71,95-101 The frequency of SEPS migration was associated with the length of stricture, the location of stricture (proximal or distal esophagus), and etiology of stricture (more often in peptic strictures, followed in order by anastomotic strictures, fistulas/leaks, and postradiation strictures).69,71,94-100,102,103 The need for repeated placement of SEPS ranged from 24% to 100% of the reported cases. Another disadvantage of SEPSs is that the stent applicator is larger and stiffer compared with that in SEMSs. Therefore, esophageal dilation before stent placement is often required.104
SEPSs have been considered a promising modality of treatment in patients with refractory benign stricture. However, recent experience shows limited efficacy and high complication rates. Further studies are required to find the most optimal indication. Therefore, the use of SEPSs cannot be routinely recommended in treatment of refractory benign esophageal strictures.
Biodegradable stents and drug-eluting stents showed promising results in case reports and several studies. However, further large, controlled studies are required to confirm the efficacy of these stents (agreement, 100%; 2C, weak recommendation, low-quality evidence).
Biodegradable stents have recently been developed. Polylactide was considered to be a candidate material for synthetic biodegradable stent, because it can provide good mechanical strength and show slower degradation rate.105 The prolonged dilatory effect before stent absorption and the progressive stent degradation are required as a more ideal material, compared to SEMSs and SEPSs for refractory benign esophageal strictures.106,107 Recent prospective preliminary study showed that nine of 20 patients (45%) recovered from dysphagia at the end of the follow-up. At 3-month endoscopy, the stent appeared to be almost fragmented in all patients. Complications were stent migration (9.5%), stent-related chest pain (14.3%), and minor bleeding (4.8%).108 Several another case series also showed similar results.109-111
Recently, endoscopic submucosal dissection (ESD) has become a major treatment option for superficial esophageal cancer and post-ESD strictures can occur in several patients. A mucosal resection over three-fourths of the circumference may cause stenotic changes and require balloon dilatation. If repetitive balloon dilation fails to improve post-ESD stricture, other interventional techniques may be needed for management of refractory esophageal strictures. Saito et al.106,107 reported that biodegradable stents were useful to achieve clinical improvements in two patients with post-ESD stricture and seven patients for prevention of stricture after ESD. Stent migration occurred in 77% of the cases within 10 to 21 days of placement. The follow-up period of these patients was between 7 months and 2 years. No patient complained of restenosis-related symptoms and additional endoscopic therapies were not required.
Although several studies showed some promising results, the long-term outcomes and safety of biodegradable stents remain to be determined.
Drug-eluting stents in animal studies showed very little tissue reaction, and they were easily separated from the esophageal tissue.112 However, drug-eluting stents have been rarely used in human cases. Until prospective long-term data were obtained from controlled trials, it is not recommended in patients with benign esophageal strictures.
There are no significant differences in technical success rate, stent patency, and overall survival between covered and uncovered stent. In complication, stent migration is common in covered stent, and restenosis is common in uncovered stent (agreement, 100%; 1A, strong recommendation, high-quality evidence).
Technical and clinical success rates were 95% to 100% and 85% to 90%, respectively. No significant differences were found between covered and uncovered stents in malignant gastric outlet obstruction. Technical success means successful stent insertion through the malignant obstruction, adequate placement and expansion in the exact site. Usually, endoscopic stent insertion using guide wire with or without fluoroscopy is not difficult in treatment of malignant gastric outlet obstruction. However, it may be difficult in patient with acute angulation of obstructive lesion or complete obstruction. Although initial stent insertion is successfully performed, several points should be considered before diet intake. They are incomplete expansion of stent, acute angulation of stent, shorter stent in longer obstruction in length. Therefore, clinical success rates are usually lower than technical success rates in most studies. Whether stent type was covered or uncovered did not influence technical or clinical success rate in most studies.
Stent migration rate was 10% to 25% in covered stent and 2% to 6% in uncovered stent. Stent migration is more frequent in covered type than in uncovered type because migration of uncovered type is prevented by the tissue embedding through the stent meshwork. In covered type, late migration is not common due to fibrotic reaction between the stent and tumor tissue, whereas early migration can occur before stent is attached to tumor tissue. Although newly developed double layered type may have less migration rate than covered type, further large scale trials are needed to confirm it.
Restenosis rate was 3% to 15% in covered stent and 10% to 42% in uncovered stent. Restenosis is more common in uncovered type than in covered type because the cover can prevent tumor ingrowth through the meshwork of stent. However, tumor overgrowh can occur at both ends of stent and tumor ingrowth is also possible due to degradation of cover portion after a long time.113-124
There are no significant differences in technical success rate, stent patency, complication, and overall patient survival, according to manufacturing companies (agreement, 100%; 1B, strong recommendation, moderate-quality evidence).
According to manufacturing companies, no significant differences have been found in clinical outcomes including technical success rate, overall patients' survival, duration of stent patency, and complications.125-130 Although prospective randomized controlled trials were not performed, most retrospective studies presented similar clinical outcomes in the same types of different manufacturers.
Endoscopic stent is a feasible alternative to surgical bypass for palliation of malignant gastric outlet obstruction with a high clinical success, low morbidity, low cost, and comparable survival (agreement, 100%; 1A, strong recommendation, high-quality evidence).
Endoscopic stent placement showed comparable outcomes to surgical bypass in terms of technical success rate, overall patients' survival, duration of stent patency, and complications. It also showed lower morbidity, lower cost, and shorter hospital stay in most studies, compared to surgical bypass.131-134 Early symptom improvement was better in stent group, whereas long-term relief was better in surgical bypass group. Early complication and mortality rate was lower in stent group except restenosis. Late complication and patients' survival were comparable between both groups. In stent group, the duration of hospital stay was shorter and total cost was lower in comparison with surgical bypass group.
Endoscopic stent is a feasible alternative to surgical bypass for recurrent unresectable or inoperable gastric outlet obstruction with a high clinical success rate, low morbidity, and low cost (agreement, 92%; 2C, weak recommendation, low-quality evidence).
Endoscopic stent placement can be considered for palliation of obstructive symptoms in recurrent unresectable or inoperable gastric outlet obstruction. Compared to surgical bypass, it showed high clinical success, lower morbidity, and lower cost. However, these results are from single-arm observational studies with small sample size. In the future, large prospective randomized controlled studies are needed to confirm the efficacy of stent placement.137-139
Temporary endoscopic stent can be a feasible alternative to surgical bypass or endoscopic dilatation for benign gastric outlet obstruction caused by recurrent duodenal ulcer, postoperative stricture after gastroduodenostomy or iatrogenic stricture after endoscopic resection. However, the efficacy or complication of the stent has not been demonstrated in the previous studies (agreement, 92%; 2C, weak recommendation, low-quality evidence).
Temporary removable endoscopic stent might be an effective treatment for benign gastric outlet obstruction caused by recurrent duodenal ulcer, postoperative stricture after gastroduodenostomy, or iatrogenic stricture after endoscopic resection.140,141 However, routine use of stent placement cannot be recommended for benign gastric outlet obstruction due to lack of data from large prospective randomized controlled studies.
Currently, stent placement is considered to be a first-line treatment for palliation of malignant obstruction in UGIT. Covered type of SEMS is superior to uncovered type to relieve obstructive symptoms in patients with unresectable esophageal cancer. No significant differences have been found in the efficacy and complication rates according to types of available SEMS. The routine use of SEMS is limited to the management of benign esophageal conditions, such as stricture, perforation, leak, and fistula. Endoscopic stents in malignant gastric outlet obstruction show comparable clinical outcomes to surgical bypass, although its use is also limited to benign gastric outlet obstruction. Endoscopic stent is feasible and effective in the management of various lesions in the upper GI tract. The development of newly-designed stents is required to expand its roles in clinical practice.
Acknowledgments
We thank Professor Kyung Sik Park and Yun Ju Jo for playing the role of external reviewers for this manuscript.
References
1. Guyatt GH, Cook DJ, Jaeschke R, Pauker SG, Schünemann HJ. Grades of recommendation for antithrombotic agents: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines (8th Edition). Chest. 2008; 133(6 Suppl):123S–131S. PMID: 18574262.
2. Homs MY, van der Gaast A, Siersema PD, Steyerberg EW, Kuipers EJ. Chemotherapy for metastatic carcinoma of the esophagus and gastroesophageal junction. Cochrane Database Syst Rev. 2006; (4):CD004063. PMID: 17054195.

3. Frenken M. Best palliation in esophageal cancer: surgery, stenting, radiation, or what? Dis Esophagus. 2001; 14:120–123. PMID: 11553221.

4. Homs MY, Kuipers EJ, Siersema PD. Palliative therapy. J Surg Oncol. 2005; 92:246–256. PMID: 16299791.

5. De Palma GD, di Matteo E, Romano G, Fimmano A, Rondinone G, Catanzano C. Plastic prosthesis versus expandable metal stents for palliation of inoperable esophageal thoracic carcinoma: a controlled prospective study. Gastrointest Endosc. 1996; 43:478–482. PMID: 8726762.

6. Knyrim K, Wagner HJ, Bethge N, Keymling M, Vakil N. A controlled trial of an expansile metal stent for palliation of esophageal obstruction due to inoperable cancer. N Engl J Med. 1993; 329:1302–1307. PMID: 7692297.

7. Mosca F, Consoli A, Stracqualursi A, Persi A, Portale TR. Comparative retrospective study on the use of plastic prostheses and self-expanding metal stents in the palliative treatment of malignant strictures of the esophagus and cardia. Dis Esophagus. 2003; 16:119–125. PMID: 12823210.

8. Vakil N, Morris AI, Marcon N, et al. A prospective, randomized, controlled trial of covered expandable metal stents in the palliation of malignant esophageal obstruction at the gastroesophageal junction. Am J Gastroenterol. 2001; 96:1791–1796. PMID: 11419831.

9. Saranovic D, Djuric-Stefanovic A, Ivanovic A, Masulovic D, Pesko P. Fluoroscopically guided insertion of self-expandable metal esophageal stents for palliative treatment of patients with malignant stenosis of esophagus and cardia: comparison of uncovered and covered stent types. Dis Esophagus. 2005; 18:230–238. PMID: 16128779.

10. Sabharwal T, Hamady MS, Chui S, Atkinson S, Mason R, Adam A. A randomised prospective comparison of the Flamingo Wallstent and Ultraflex stent for palliation of dysphagia associated with lower third oesophageal carcinoma. Gut. 2003; 52:922–926. PMID: 12801944.

11. Baerlocher MO, Asch MR, Dixon P, et al. Interdisciplinary Canadian guidelines on the use of metal stents in the gastrointestinal tract for oncological indications. Can Assoc Radiol J. 2008; 59:107–122. PMID: 18697717.
12. Sabharwal T, Morales JP, Salter R, Adam A. Esophageal cancer: self-expanding metallic stents. Abdom Imaging. 2005; 30:456–464. PMID: 15688108.

13. Kim ES, Jeon SW, Park SY, et al. Comparison of double-layered and covered Niti-S stents for palliation of malignant dysphagia. J Gastroenterol Hepatol. 2009; 24:114–119. PMID: 19054264.

14. Verschuur EM, Homs MY, Steyerberg EW, et al. A new esophageal stent design (Niti-S stent) for the prevention of migration: a prospective study in 42 patients. Gastrointest Endosc. 2006; 63:134–140. PMID: 16377330.

15. Sabharwal T, Morales JP, Irani FG, Adam A. CIRSE Cardiovascular and Interventional Radiological Society of Europe. Quality improvement guidelines for placement of esophageal stents. Cardiovasc Intervent Radiol. 2005; 28:284–288. PMID: 15886931.

16. Siersema PD, Hop WC, van Blankenstein M, et al. A comparison of 3 types of covered metal stents for the palliation of patients with dysphagia caused by esophagogastric carcinoma: a prospective, randomized study. Gastrointest Endosc. 2001; 54:145–153. PMID: 11474382.

17. May A, Hahn EG, Ell C. Self-expanding metal stents for palliation of malignant obstruction in the upper gastrointestinal tract. Comparative assessment of three stent types implemented in 96 implantations. J Clin Gastroenterol. 1996; 22:261–266. PMID: 8771419.
18. Siersema PD. New developments in palliative therapy. Best Pract Res Clin Gastroenterol. 2006; 20:959–978. PMID: 16997172.

19. Eleftheriadis E, Kotzampassi K. Endoprosthesis implantation at the pharyngo-esophageal level: problems, limitations and challenges. World J Gastroenterol. 2006; 12:2103–2108. PMID: 16610065.

20. Macdonald S, Edwards RD, Moss JG. Patient tolerance of cervical esophageal metallic stents. J Vasc Interv Radiol. 2000; 11:891–898. PMID: 10928528.

21. Shim CS, Jung IS, Bhandari S, et al. Management of malignant strictures of the cervical esophagus with a newly-designed self-expanding metal stent. Endoscopy. 2004; 36:554–557. PMID: 15202054.

22. Homs MY, Wahab PJ, Kuipers EJ, et al. Esophageal stents with antireflux valve for tumors of the distal esophagus and gastric cardia: a randomized trial. Gastrointest Endosc. 2004; 60:695–702. PMID: 15557944.

23. May A, Ell C. Palliative treatment of malignant esophagorespiratory fistulas with Gianturco-Z stents. A prospective clinical trial and review of the literature on covered metal stents. Am J Gastroenterol. 1998; 93:532–535. PMID: 9576443.

24. Shin JH, Song HY, Ko GY, Lim JO, Yoon HK, Sung KB. Esophagorespiratory fistula: long-term results of palliative treatment with covered expandable metallic stents in 61 patients. Radiology. 2004; 232:252–259. PMID: 15166325.

25. Lecleire S, Di Fiore F, Ben-Soussan E, et al. Prior chemoradiotherapy is associated with a higher life-threatening complication rate after palliative insertion of metal stents in patients with oesophageal cancer. Aliment Pharmacol Ther. 2006; 23:1693–1702. PMID: 16817912.

26. Homann N, Noftz MR, Klingenberg-Noftz RD, Ludwig D. Delayed complications after placement of self-expanding stents in malignant esophageal obstruction: treatment strategies and survival rate. Dig Dis Sci. 2008; 53:334–340. PMID: 17597412.

27. Conio M, Repici A, Battaglia G, et al. A randomized prospective comparison of self-expandable plastic stents and partially covered self-expandable metal stents in the palliation of malignant esophageal dysphagia. Am J Gastroenterol. 2007; 102:2667–2677. PMID: 18042102.

28. Conigliaro R, Battaglia G, Repici A, et al. Polyflex stents for malignant oesophageal and oesophagogastric stricture: a prospective, multicentric study. Eur J Gastroenterol Hepatol. 2007; 19:195–203. PMID: 17301645.

29. Siersema PD, Schrauwen SL, van Blankenstein M, et al. Self-expanding metal stents for complicated and recurrent esophagogastric cancer. Gastrointest Endosc. 2001; 54:579–586. PMID: 11677473.

30. Kozarek RA, Raltz S, Marcon N, et al. Use of the 25 mm flanged esoph ageal Z stent for malignant dysphagia: a prospective multicenter trial. Gastrointest Endosc. 1997; 46:156–160. PMID: 9283867.
31. Bartelsman JF, Bruno MJ, Jensema AJ, Haringsma J, Reeders JW, Tytgat GN. Palliation of patients with esophagogastric neoplasms by insertion of a covered expandable modified Gianturco-Z endoprosthesis: experiences in 153 patients. Gastrointest Endosc. 2000; 51:134–138. PMID: 10650253.

32. Verschuur EM, Steyerberg EW, Kuipers EJ, Siersema PD. Effect of stent size on complications and recurrent dysphagia in patients with esophageal or gastric cardia cancer. Gastrointest Endosc. 2007; 65:592–601. PMID: 17383456.

33. Baron TH. Minimizing endoscopic complications: endoluminal stents. Gastrointest Endosc Clin N Am. 2007; 17:83–104. PMID: 17397778.

34. Verschuur EM, Repici A, Kuipers EJ, Steyerberg EW, Siersema PD. New design esophageal stents for the palliation of dysphagia from esophageal or gastric cardia cancer: a randomized trial. Am J Gastroenterol. 2008; 103:304–312. PMID: 17900325.

35. Dua KS, Kozarek R, Kim J, et al. Self-expanding metal esophageal stent with anti-reflux mechanism. Gastrointest Endosc. 2001; 53:603–613. PMID: 11323586.

36. Laasch HU, Marriott A, Wilbraham L, Tunnah S, England RE, Martin DF. Effectiveness of open versus antireflux stents for palliation of distal esophageal carcinoma and prevention of symptomatic gastroesophageal reflux. Radiology. 2002; 225:359–365. PMID: 12409567.

37. Shim CS, Jung IS, Cheon YK, et al. Management of malignant stricture of the esophagogastric junction with a newly designed self-expanding metal stent with an antireflux mechanism. Endoscopy. 2005; 37:335–339. PMID: 15824943.

38. Shin JH, Song HY, Kim JH, et al. Comparison of temporary and permanent stent placement with concurrent radiation therapy in patients with esophageal carcinoma. J Vasc Interv Radiol. 2005; 16:67–74. PMID: 15640412.

39. Ross WA, Alkassab F, Lynch PM, et al. Evolving role of self-expanding metal stents in the treatment of malignant dysphagia and fistulas. Gastrointest Endosc. 2007; 65:70–76. PMID: 17185082.

40. Low DE, Kozarek RA. Comparison of conventional and wire mesh expandable prostheses and surgical bypass in patients with malignant esophagorespiratory fistulas. Ann Thorac Surg. 1998; 65:919–923. PMID: 9564901.

41. Saxon RR, Morrison KE, Lakin PC, et al. Malignant esophageal obstruction and esophagorespiratory fistula: palliation with a polyethylene-covered Z-stent. Radiology. 1997; 202:349–354. PMID: 9015055.

42. Sarper A, Oz N, Cihangir C, Demircan A, Isin E. The efficacy of self-expanding metal stents for palliation of malignant esophageal strictures and fistulas. Eur J Cardiothorac Surg. 2003; 23:794–798. PMID: 12754035.

43. Morgan RA, Ellul JP, Denton ER, Glynos M, Mason RC, Adam A. Malignant esophageal fistulas and perforations: management with plastic-covered metallic endoprostheses. Radiology. 1997; 204:527–532. PMID: 9240548.

44. Dumonceau JM, Cremer M, Lalmand B, Devière J. Esophageal fistula sealing: choice of stent, practical management, and cost. Gastrointest Endosc. 1999; 49:70–78. PMID: 9869726.

45. Do YS, Song HY, Lee BH, et al. Esophagorespiratory fistula associated with esophageal cancer: treatment with a Gianturco stent tube. Radiology. 1993; 187:673–677. PMID: 7684529.

46. Bethge N, Sommer A, Vakil N. Treatment of esophageal fistulas with a new polyurethane-covered, self-expanding mesh stent: a prospective study. Am J Gastroenterol. 1995; 90:2143–2146. PMID: 8540504.
47. Kozarek RA, Raltz S, Brugge WR, et al. Prospective multicenter trial of esophageal Z-stent placement for malignant dysphagia and tracheoesophageal fistula. Gastrointest Endosc. 1996; 44:562–567. PMID: 8934162.

48. Raijman I, Siddique I, Ajani J, Lynch P. Palliation of malignant dysphagia and fistulae with coated expandable metal stents: experience with 101 patients. Gastrointest Endosc. 1998; 48:172–179. PMID: 9717783.

49. Power C, Byrne PJ, Lim K, et al. Superiority of anti-reflux stent compared with conventional stents in the palliative management of patients with cancer of the lower esophagus and esophago-gastric junction: results of a randomized clinical trial. Dis Esophagus. 2007; 20:466–470. PMID: 17958720.

50. Lee S, Osugi H, Tokuhara T, et al. Self-expandable metallic stent for unresectable malignant strictures in the esophagus and cardia. Jpn J Thorac Cardiovasc Surg. 2005; 53:470–476. PMID: 16200886.

51. Davies RP, Kew J, Byrne PD. Treatment of post-stent gastroesophageal reflux by anti-reflux Z-stent. Cardiovasc Intervent Radiol. 2000; 23:487–489. PMID: 11232903.

52. Wenger U, Johnsson E, Arnelo U, Lundell L, Lagergren J. An antireflux stent versus conventional stents for palliation of distal esophageal or cardia cancer: a randomized clinical study. Surg Endosc. 2006; 20:1675–1680. PMID: 16960663.

53. Sgourakis G, Gockel I, Radtke A, et al. The use of self-expanding stents in esophageal and gastroesophageal junction cancer palliation: a meta-analysis and meta-regression analysis of outcomes. Dig Dis Sci. 2010; 55:3018–3030. PMID: 20440646.

54. Verschuur EM, Kuipers EJ, Siersema PD. Esophageal stents for malignant strictures close to the upper esophageal sphincter. Gastrointest Endosc. 2007; 66:1082–1090. PMID: 17826774.

55. Raju GS, Thompson C, Zwischenberger JB. Emerging endoscopic options in the management of esophageal leaks (videos). Gastrointest Endosc. 2005; 62:278–286. PMID: 16046996.

56. Pate JW, Walker WA, Cole FH Jr, Owen EW, Johnson WH. Spontaneous rupture of the esophagus: a 30-year experience. Ann Thorac Surg. 1989; 47:689–692. PMID: 2730190.

57. Attar S, Hankins JR, Suter CM, Coughlin TR, Sequeira A, McLaughlin JS. Esophageal perforation: a therapeutic challenge. Ann Thorac Surg. 1990; 50:45–49. PMID: 2369229.

58. Brinster CJ, Singhal S, Lee L, Marshall MB, Kaiser LR, Kucharczuk JC. Evolving options in the management of esophageal perforation. Ann Thorac Surg. 2004; 77:1475–1483. PMID: 15063302.

59. Zwischenberger JB, Savage C, Bidani A. Surgical aspects of esophageal disease: perforation and caustic injury. Am J Respir Crit Care Med. 2002; 165:1037–1040. PMID: 11956041.
60. Tilanus HW, Bossuyt P, Schattenkerk ME, Obertop H. Treatment of oesophageal perforation: a multivariate analysis. Br J Surg. 1991; 78:582–585. PMID: 2059811.

61. Adam A, Watkinson AF, Dussek J. Boerhaave syndrome: to treat or not to treat by means of insertion of a metallic stent. J Vasc Interv Radiol. 1995; 6:741–743. PMID: 8541678.

62. Eubanks PJ, Hu E, Nguyen D, Procaccino F, Eysselein VE, Klein SR. Case of Boerhaave's syndrome successfully treated with a self-expandable metallic stent. Gastrointest Endosc. 1999; 49:780–783. PMID: 10343228.

63. Chung MG, Kang DH, Park DK, Park JJ, Park HC, Kim JH. Successful treatment of Boerhaave's syndrome with endoscopic insertion of a self-expandable metallic stent: report of three cases and a review of the literature. Endoscopy. 2001; 33:894–897. PMID: 11571689.

64. Petruzziello L, Tringali A, Riccioni ME, et al. Successful early treatment of Boerhaave's syndrome by endoscopic placement of a temporary self-expandable plastic stent without fluoroscopy. Gastrointest Endosc. 2003; 58:608–612. PMID: 14520304.

65. Siersema PD, Homs MY, Haringsma J, Tilanus HW, Kuipers EJ. Use of large-diameter metallic stents to seal traumatic nonmalignant perforations of the esophagus. Gastrointest Endosc. 2003; 58:356–361. PMID: 14528208.

66. Koch S, Weber A, Fein F, et al. Esophageal stents as a salvage therapy for non-malignant iatrogenic esophageal perforations. Gastroenterol Clin Biol. 2005; 29:735–739. PMID: 16142010.

67. Johnsson E, Lundell L, Liedman B. Sealing of esophageal perforation or ruptures with expandable metallic stents: a prospective controlled study on treatment efficacy and limitations. Dis Esophagus. 2005; 18:262–266. PMID: 16128784.

68. Fischer A, Thomusch O, Benz S, von Dobschuetz E, Baier P, Hopt UT. Nonoperative treatment of 15 benign esophageal perforations with self-expandable covered metal stents. Ann Thorac Surg. 2006; 81:467–472. PMID: 16427833.

69. Radecke K, Gerken G, Treichel U. Impact of a self-expanding, plastic esophageal stent on various esophageal stenoses, fistulas, and leakages: a single-center experience in 39 patients. Gastrointest Endosc. 2005; 61:812–818. PMID: 15933681.

70. Ott C, Ratiu N, Endlicher E, et al. Self-expanding Polyflex plastic stents in esophageal disease: various indications, complications, and outcomes. Surg Endosc. 2007; 21:889–896. PMID: 17177084.

71. Karbowski M, Schembre D, Kozarek R, Ayub K, Low D. Polyflex self-expanding, removable plastic stents: assessment of treatment efficacy and safety in a variety of benign and malignant conditions of the esophagus. Surg Endosc. 2008; 22:1326–1333. PMID: 18027044.

72. Freeman RK, Van Woerkom JM, Ascioti AJ. Esophageal stent placement for the treatment of iatrogenic intrathoracic esophageal perforation. Ann Thorac Surg. 2007; 83:2003–2007. PMID: 17532387.

73. Profili S, Feo CF, Cossu ML, et al. Effective management of intrathoracic anastomotic leak with covered self-expandable metal stents. Report on three cases. Emerg Radiol. 2008; 15:57–60. PMID: 17570002.

74. Nowakowski P, Ziaja K, Ludyga T, et al. Self-expandable metallic stents in the treatment of post-esophagogastrostomy/post-esophagoenterostomy fistula. Dis Esophagus. 2007; 20:358–360. PMID: 17617887.

75. Eleftheriadis E, Kotzampassi K. Temporary stenting of acquired benign tracheoesophageal fistulas in critically ill ventilated patients. Surg Endosc. 2005; 19:811–815. PMID: 15868255.

76. Hünerbein M, Stroszczynski C, Moesta KT, Schlag PM. Treatment of thoracic anastomotic leaks after esophagectomy with self-expanding plastic stents. Ann Surg. 2004; 240:801–807. PMID: 15492561.

77. Gelbmann CM, Ratiu NL, Rath HC, et al. Use of self-expandable plastic stents for the treatment of esophageal perforations and symptomatic anastomotic leaks. Endoscopy. 2004; 36:695–699. PMID: 15280974.

78. Langer FB, Wenzl E, Prager G, et al. Management of postoperative esophageal leaks with the Polyflex self-expanding covered plastic stent. Ann Thorac Surg. 2005; 79:398–403. PMID: 15680802.

79. Schubert D, Scheidbach H, Kuhn R, et al. Endoscopic treatment of thoracic esophageal anastomotic leaks by using silicone-covered, self-expanding polyester stents. Gastrointest Endosc. 2005; 61:891–896. PMID: 15933696.

80. Ackroyd R, Watson DI, Devitt PG, Jamieson GG. Expandable metallic stents should not be used in the treatment of benign esophageal strictures. J Gastroenterol Hepatol. 2001; 16:484–487. PMID: 11354292.

81. Fiorini A, Fleischer D, Valero J, Israeli E, Wengrower D, Goldin E. Self-expandable metal coil stents in the treatment of benign esophageal strictures refractory to conventional therapy: a case series. Gastrointest Endosc. 2000; 52:259–262. PMID: 10922106.

82. Hramiec JE, O'Shea MA, Quinlan RM. Expandable metallic esophageal stents in benign disease: a cause for concern. Surg Laparosc Endosc. 1998; 8:40–43. PMID: 9488569.
83. Song HY, Park SI, Jung HY, et al. Benign and malignant esophageal strictures: treatment with a polyurethane-covered retrievable expandable metallic stent. Radiology. 1997; 203:747–752. PMID: 9169699.

84. Sandha GS, Marcon NE. Expandable metal stents for benign esophageal obstruction. Gastrointest Endosc Clin N Am. 1999; 9:437–446. PMID: 10388859.

85. Wadhwa RP, Kozarek RA, France RE, et al. Use of self-expandable metallic stents in benign GI diseases. Gastrointest Endosc. 2003; 58:207–212. PMID: 12872087.

86. Song HY, Park SI, Do YS, et al. Expandable metallic stent placement in patients with benign esophageal strictures: results of long-term follow-up. Radiology. 1997; 203:131–136. PMID: 9122381.

87. Tan BS, Kennedy C, Morgan R, Owen W, Adam A. Using uncovered metallic endoprostheses to treat recurrent benign esophageal strictures. AJR Am J Roentgenol. 1997; 169:1281–1284. PMID: 9353442.

88. Han HW, Lee IS, Park JM, et al. Self-expandable metallic stent therapy for a gastrointestinal benign stricture. Korean J Gastrointest Endosc. 2008; 37:1–6.
89. Cheng YS, Li MH, Chen WX, Chen NW, Zhuang QX, Shang KZ. Temporary partially-covered metal stent insertion in benign esophageal stricture. World J Gastroenterol. 2003; 9:2359–2361. PMID: 14562413.

90. Song HY, Jung HY, Park SI, et al. Covered retrievable expandable nitinol stents in patients with benign esophageal strictures: initial experience. Radiology. 2000; 217:551–557. PMID: 11058659.

91. Conio M, Blanchi S, Filiberti R, et al. A modified self-expanding Niti-S stent for the management of benign hypopharyngeal strictures. Gastrointest Endosc. 2007; 65:714–720. PMID: 17383472.

92. Mayoral W, Fleischer D, Salcedo J, Roy P, Al-Kawas F, Benjamin S. Nonmalignant obstruction is a common problem with metal stents in the treatment of esophageal cancer. Gastrointest Endosc. 2000; 51:556–559. PMID: 10805841.

93. Kim JH, Song HY, Choi EK, Kim KR, Shin JH, Lim JO. Temporary metallic stent placement in the treatment of refractory benign esophageal strictures: results and factors associated with outcome in 55 patients. Eur Radiol. 2009; 19:384–390. PMID: 18726598.

94. Holm AN, de la Mora Levy JG, Gostout CJ, Topazian MD, Baron TH. Self-expanding plastic stents in treatment of benign esophageal conditions. Gastrointest Endosc. 2008; 67:20–25. PMID: 17945227.

95. Evrard S, Le Moine O, Lazaraki G, Dormann A, El Nakadi I, Deviere J. Self-expanding plastic stents for benign esophageal lesions. Gastrointest Endosc. 2004; 60:894–900. PMID: 15605003.

96. García-Cano J. Dilation of benign strictures in the esophagus and colon with the polyflex stent: a case series study. Dig Dis Sci. 2008; 53:341–346. PMID: 17565471.

97. Pennathur A, Chang AC, McGrath KM, et al. Polyflex expandable stents in the treatment of esophageal disease: initial experience. Ann Thorac Surg. 2008; 85:1968–1972. PMID: 18498804.

98. Barthel JS, Kelley ST, Klapman JB. Management of persistent gastroesophageal anastomotic strictures with removable self-expandable polyester silicon-covered (Polyflex) stents: an alternative to serial dilation. Gastrointest Endosc. 2008; 67:546–552. PMID: 18294520.

99. Repici A, Conio M, De Angelis C, et al. Temporary placement of an expandable polyester silicone-covered stent for treatment of refractory benign esophageal strictures. Gastrointest Endosc. 2004; 60:513–519. PMID: 15472671.

100. Dua KS, Vleggaar FP, Santharam R, Siersema PD. Removable self-expanding plastic esophageal stent as a continuous, non-permanent dilator in treating refractory benign esophageal strictures: a prospective two-center study. Am J Gastroenterol. 2008; 103:2988–2994. PMID: 18786110.

101. Broto J, Asensio M, Vernet JM. Results of a new technique in the treatment of severe esophageal stenosis in children: poliflex stents. J Pediatr Gastroenterol Nutr. 2003; 37:203–206. PMID: 12883312.

102. Triester SL, Fleischer DE, Sharma VK. Failure of self-expanding plastic stents in treatment of refractory benign esophageal strictures. Endoscopy. 2006; 38:533–537. PMID: 16767594.

103. Martin RC, Woodall C, Duvall R, Scoggins CR. The use of self-expanding silicone stents in esophagectomy strictures: less cost and more efficiency. Ann Thorac Surg. 2008; 86:436–440. PMID: 18640310.

104. Siersema PD. Treatment options for esophageal strictures. Nat Clin Pract Gastroenterol Hepatol. 2008; 5:142–152. PMID: 18250638.

105. Freeman ML. Bioabsorbable stents for gastrointestinal endoscopy. Tech Gastrointest Endosc. 2001; 3:120–125.

106. Saito Y, Tanaka T, Andoh A, et al. Novel biodegradable stents for benign esophageal strictures following endoscopic submucosal dissection. Dig Dis Sci. 2008; 53:330–333. PMID: 17713855.

107. Saito Y, Tanaka T, Andoh A, et al. Usefulness of biodegradable stents constructed of poly-l-lactic acid monofilaments in patients with benign esophageal stenosis. World J Gastroenterol. 2007; 13:3977–3980. PMID: 17663513.

108. Repici A, Vleggaar FP, Hassan C, et al. Efficacy and safety of biodegradable stents for refractory benign esophageal strictures: the BEST (Biodegradable Esophageal Stent) study. Gastrointest Endosc. 2010; 72:927–934. PMID: 21034894.

109. Tanaka T, Takahashi M, Nitta N, et al. Newly developed biodegradable stents for benign gastrointestinal tract stenoses: a preliminary clinical trial. Digestion. 2006; 74:199–205. PMID: 17341853.

110. Fry SW, Fleischer DE. Management of a refractory benign esophageal stricture with a new biodegradable stent. Gastrointest Endosc. 1997; 45:179–182. PMID: 9041006.

111. Stivaros SM, Williams LR, Senger C, Wilbraham L, Laasch HU. Woven polydioxanone biodegradable stents: a new treatment option for benign and malignant oesophageal strictures. Eur Radiol. 2010; 20:1069–1072. PMID: 19921200.

112. Jeon SR, Eun SH, Shim CS, et al. Effect of drug-eluting metal stents in benign esophageal stricture: an in vivo animal study. Endoscopy. 2009; 41:449–456. PMID: 19418400.

113. Lopera JE, Brazzini A, Gonzales A, Castaneda-Zuniga WR. Gastroduodenal stent placement: current status. Radiographics. 2004; 24:1561–1573. PMID: 15537965.

114. Telford JJ, Carr-Locke DL, Baron TH, et al. Palliation of patients with malignant gastric outlet obstruction with the enteral Wallstent: outcomes from a multicenter study. Gastrointest Endosc. 2004; 60:916–920. PMID: 15605006.

115. Holt AP, Patel M, Ahmed MM. Palliation of patients with malignant gastroduodenal obstruction with self-expanding metallic stents: the treatment of choice? Gastrointest Endosc. 2004; 60:1010–1017. PMID: 15605026.

116. Kim JH, Song HY, Shin JH, et al. Metallic stent placement in the palliative treatment of malignant gastric outlet obstructions: primary gastric carcinoma versus pancreatic carcinoma. AJR Am J Roentgenol. 2009; 193:241–247. PMID: 19542420.

117. Cho YK, Kim SW, Hur WH, et al. Clinical outcomes of self-expandable metal stent and prognostic factors for stent patency in gastric outlet obstruction caused by gastric cancer. Dig Dis Sci. 2010; 55:668–674. PMID: 19333756.

118. Seo EH, Jung MK, Park MJ, et al. Covered expandable nitinol stents for malignant gastroduodenal obstructions. J Gastroenterol Hepatol. 2008; 23(7 Pt 1):1056–1062. PMID: 18086117.

119. Kim GH, Kang DH, Lee DH, et al. Which types of stent, uncovered or covered, should be used in gastric outlet obstructions? Scand J Gastroenterol. 2004; 39:1010–1014. PMID: 15513343.

120. Kim CG, Choi IJ, Lee JY, et al. Covered versus uncovered self-expandable metallic stents for palliation of malignant pyloric obstruction in gastric cancer patients: a randomized, prospective study. Gastrointest Endosc. 2010; 72:25–32. PMID: 20381802.

121. Boškoski I, Tringali A, Familiari P, Mutignani M, Costamagna G. Self-expandable metallic stents for malignant gastric outlet obstruction. Adv Ther. 2010; 27:691–703. PMID: 20737260.

122. Havemann MC, Adamsen S, Wøjdemann M. Malignant gastric outlet obstruction managed by endoscopic stenting: a prospective single-centre study. Scand J Gastroenterol. 2009; 44:248–251. PMID: 19016077.

123. Shimura T, Kataoka H, Sasaki M, et al. Feasibility of self-expandable metallic stent plus chemotherapy for metastatic gastric cancer with pyloric stenosis. J Gastroenterol Hepatol. 2009; 24:1358–1364. PMID: 19467141.

124. Kim TO, Kang DH, Kim GH, et al. Self-expandable metallic stents for palliation of patients with malignant gastric outlet obstruction caused by stomach cancer. World J Gastroenterol. 2007; 13:916–920. PMID: 17352023.

125. Im JP, Kang JM, Kim SG, Kim JS, Jung HC, Song IS. Clinical outcomes and patency of self-expanding metal stents in patients with malignant upper gastrointestinal obstruction. Dig Dis Sci. 2008; 53:938–945. PMID: 17805967.

126. Kwon DS, Goh PG, Hwang SW, et al. The use of uncovered self-expandable metallic stents for palliation of gastric outlet obstruction caused by stomach cancer. Korean J Gastrointest Endosc. 2008; 36:336–340.
127. Park HY, Kang DH, Eum JS, et al. Uncovered self-expandable metal stents (SEMS) for gastric outlet obstruction caused by stomach cancer. Korean J Gastrointest Endosc. 2008; 36:57–63.
128. van Hooft JE, Uitdehaag MJ, Bruno MJ, et al. Efficacy and safety of the new WallFlex enteral stent in palliative treatment of malignant gastric outlet obstruction (DUOFLEX study): a prospective multicenter study. Gastrointest Endosc. 2009; 69:1059–1066. PMID: 19152912.

129. Lee SM, Kang DH, Kim GH, Park WI, Kim HW, Park JH. Self-expanding metallic stents for gastric outlet obstruction resulting from stomach cancer: a preliminary study with a newly designed double-layered pyloric stent. Gastrointest Endosc. 2007; 66:1206–1210. PMID: 18028923.

130. Lee SH, Kang DH, Bae YM, et al. Treatment of gastric outlet obstruction by stomach cancer with using double-layered pyloric stent. Korean J Gastrointest Endosc. 2007; 35:221–227.
131. Siddiqui A, Spechler SJ, Huerta S. Surgical bypass versus endoscopic stenting for malignant gastroduodenal obstruction: a decision analysis. Dig Dis Sci. 2007; 52:276–281. PMID: 17160470.

132. Hosono S, Ohtani H, Arimoto Y, Kanamiya Y. Endoscopic stenting versus surgical gastroenterostomy for palliation of malignant gastroduodenal obstruction: a meta-analysis. J Gastroenterol. 2007; 42:283–290. PMID: 17464457.

133. Jeurnink SM, van Eijck CH, Steyerberg EW, Kuipers EJ, Siersema PD. Stent versus gastrojejunostomy for the palliation of gastric outlet obstruction: a systematic review. BMC Gastroenterol. 2007; 7:18. PMID: 17559659.

134. Jeurnink SM, Steyerberg EW, van Hooft JE, et al. Surgical gastrojejunostomy or endoscopic stent placement for the palliation of malignant gastric outlet obstruction (SUSTENT study): a multicenter randomized trial. Gastrointest Endosc. 2010; 71:490–499. PMID: 20003966.

135. Kim ID, Kang DH, Choi CW, et al. Prevention of covered enteral stent migration in patients with malignant gastric outlet obstruction: a pilot study of anchoring with endoscopic clips. Scand J Gastroenterol. 2010; 45:100–105. PMID: 20030581.

136. Park SY, Park CH, Cho SB, et al. The usefulness of clip application in preventing migration of self-expandable metal stent in patients with malignant gastrointestinal obstruction. Korean J Gastroenterol. 2007; 49:4–9. PMID: 18167427.
137. Lee WH, Ko JH, Jung GS, Jeong KS, Kim KJ, Lee SH. Covered self-expandable metallic stent placement for a post-operative malignant anastomotic stricture secondary to recurrent gastric cancer. J Korean Radiol Soc. 2007; 57:253–259.

138. Jo SJ, Yoon KY, Choi KH, et al. A comparative study of stenting versus surgical bypass in gastric outlet obstruction caused by gastric cancer. J Korean Gastric Cancer Assoc. 2007; 7:82–87.

139. Cho YK, Kim SW, Nam KW, et al. Clinical outcomes of self-expandable metal stents in palliation of malignant anastomotic strictures caused by recurrent gastric cancer. World J Gastroenterol. 2009; 15:3523–3527. PMID: 19630108.

140. Bae JI, Shin JH, Song HY, Lee GH. Treatment of a benign anastomotic duodenojejunal stricture with a polytetrafluoroethylene-covered retrievable expandable nitinol stent. J Vasc Interv Radiol. 2004; 15:769–772. PMID: 15231893.

141. Joo MK, Park JJ, Lee BJ, et al. A case of stenotic change from gastric candidiasis managed with temporary stent insertion. Gut Liver. 2011; 5:238–241. PMID: 21814608.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download