Abstract
Although there is no survival advantage, inoperable hilar cholangiocarcinoma managed by palliative drainage may benefit from symptomatic improvement. In general, biliary drainage is divided into endoscopic or percutaneous approaches and surgical drainage. Plastic or metal stent is the most preferred device for palliative drainage in endoscopic approach. Considering cost-effectiveness, use of metallic stent is preferred than plastic stents in patients with more than 3 months of life expectancy with inoperable malignant biliary obstruction. In patients with unresectable malignant hilar obstruction, the endoscopic approach with biliary stent placement by experts has been considered as the treatment of choice. However, the endoscopic management of hilar obstruction is often more challenging and complex than distal malignant biliary obstructions. There is still a lack of clear consensus on the use of plastic versus metal stents and unilateral versus bilateral drainage since the decision should be made under many grounds such as the volume of liver drainage more than 50%, life expectancy, and expertise of the facility.
Hilar cholangiocarcinoma has a very poor prognosis, with less than 10% of patients surviving past 5 years. The vast majority of patients with hilar cholangiocarcinoma are not good candidates for curative surgery, but may benefit from palliative biliary drainage by stent placement, which is the treatment of choice for inoperable malignant hilar biliary strictures (HBS). As a palliative decompressive method, endoscopic drainage using metal or plastic stents has been proposed as an alternative to biliary-enteric bypass surgery and percutaneous drainage to palliate malignant HBSs.1-3 When appropriate endoscopic expertise is available, endoscopic palliation is considered the treatment of choice for nonresectable malignant HBS. Combined percutaneous and endoscopic procedures or percutaneous drainage alone are used in malignant HBS either after the failure of the endoscopic procedure or for further nonsurgical intervention where obstructive cholestasis fails to be resolved after the endoscopic procedure.1
However, the management of biliary decompression in malignant HBS is often more challenging and complex than in distal malignant biliary obstructions, and controversy exists regarding the use of one or multiple stents (unilateral versus bilateral), and plastic or metal stents for the optimum approach to endoscopic palliation. The clinical success rate of all biliary drainage procedures in HBS is less than that for distal biliary obstructions. Also, the strategy of palliative treatment differs according to the location or level of the malignant biliary stricture. In this section we reviewed the current strategy and technical issues for the endoscopic biliary stenting in inoperable malignant HBS.
Both plastic stents and metallic stents can be used for the palliation of malignant bile duct obstructions. Plastic stents have some advantages, including: less expense, technically easy insertion, and relatively easy removal and exchange when stent occlusion or malfunctions occur. However, plastic stents in hilar strictures have limited stent patency due to their narrow lumen and a higher chance of clogging because of the longer length of the stent. Stent occlusion frequently results in cholangitis, with rates as high as 20% to 40% reported for unilateral or bilateral plastic stents because of biofilm formation and sludge impaction secondary to the small diameter or bacterial contamination of the undrained bile ducts. Moreover, it is technically difficult to place more than two 10 Fr plastic stents initially, and they may be prone to distal migration due to elastic restoring force.1-4
Comparative trials have shown that plastic stent patency is significantly prolonged by the use of larger caliber stents (10 and 11.5 Fr) compared with smaller caliber stents (5, 7, and 8.5 Fr).4-6 However, in a retrospective study comparing the efficacy and complications of 10 Fr biliary stents with 11.5 Fr stents in the management of malignant and benign biliary tract diseases, there was no significant difference in success rates or complications.7 There was also no significant difference found according to stent design and materials in some studies.8-10 However, these studies were performed only in distal common bile duct (CBD) malignancy (nonhilar biliary obstruction).
Theoretically, a metal stent may result in better drainage than plastic stents in malignant HBSs. Metal stents have two advantages over the plastic stents. First, they do not occlude side branches because of the mesh, and since most malignant HBSs are firm and scirrhous, tumor ingrowth probably occurs less frequently. Second, metallic stents offer a longer but still limited stent patency due to a larger diameter of stent as up to 30 Fr or 10 mm, when deployed, using a relatively smaller delivery system of 7 to 8 Fr, facilitating easier passage across the biliary strictures. Self-expanding metal stents (SEMSs) have been used to delay stent occlusion and minimize the need for the reintervention that is common with plastic stents. More recently, covered SEMSs have been introduced with the goal of prolonging stent patency by inhibiting tumor in-growth through the interstices. The larger internal caliber relative to the plastic stents leads to prolonged stent patency (5 to 10 months).11-13 However, for malignant HBSs, only uncovered SEMSs are available. Since covered SEMSs can occlude intrahepatic side branches, their placement in advanced hilar malignancy is not commonly performed and only a few cases have been reported in the literature.
Regarding appropriate position of stents, generally the distal part of the SEMS should protrude about 1 cm into the duodenum to allow easy endoscopic access, in case it is needed for the restoration of patency of occluded stents. Placement of stents above an intact sphincter of Oddi might prevent migration of bacteria and deposition of organic material into the stent. In patients with malignant obstructive jaundice, prolongation of function time of the stent would be expected if it is placed above the sphincter of Oddi. However, there are few comparative results for the position of stents. A study using 10 Fr Teflon stent did not show a difference on stent function between stents placed above and across the sphincter of Oddi in malignant bile duct obstruction.14
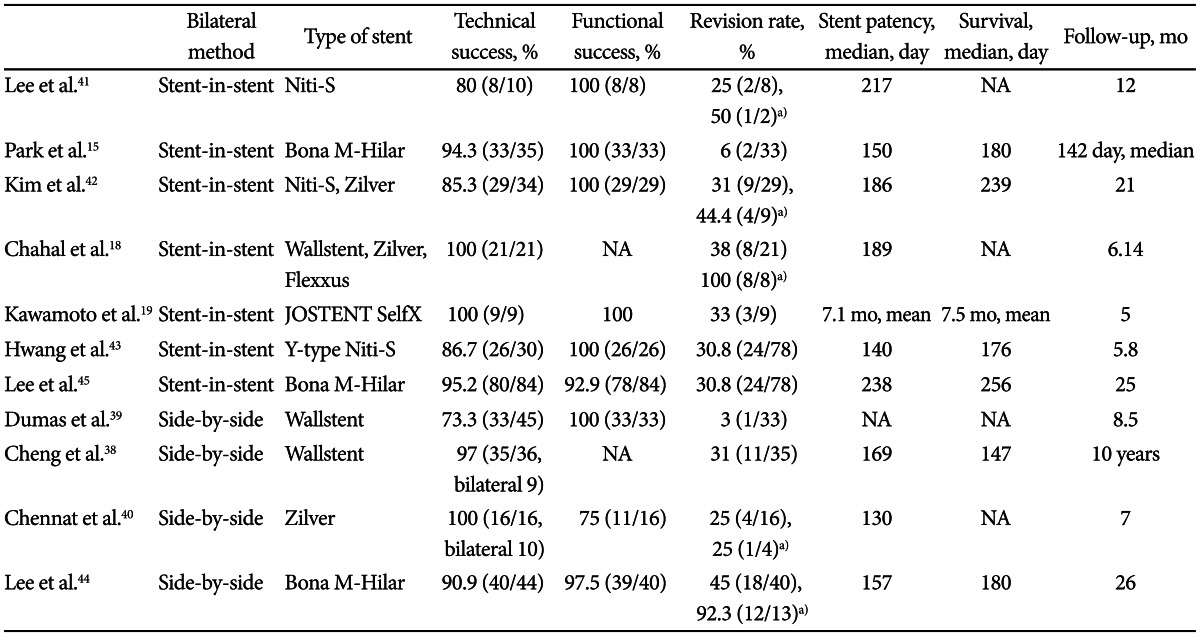
SEMSs are composed of either stainless steel or nickel shape-retaining titanium (Nitinol). Structurally, metal stents are divided into a closed-cell type (Wallstent, Boston Scientific Co., Natick, MA, USA; Niti-S, Taewoong Medical Inc., Seoul, Korea; Hanarostent, M.I. Tech Co., Seoul, Korea; Bonastent, Standard SciTech Inc., Seoul, Korea) and an open-cell type (Zilver stent, Wilson-Cook Medical Inc., Winston-Salem, NC, USA; and Niti-S Y-type, Taewoong Medical Inc.). Open-cell design stents are readily dilated by ballooning and then remain in the dilated state. These characteristics may be important factors in the success of primary placement of stents and secondary revisions, but stents placed in this manner may show weak patency in the central portion due to the large open-cell structures. In contrast, closed-cell design stents have been shown to increase patency rates and improve the palliation of CBD obstructions. However, a review of previous studies found no proven differences in patency or successful revision rates between closed-cell and open-cell design stents. Technical success rates of closed-cell and open-cell design stents ranged from 73.3% to 100%, depending on whether a stent-in-stent or side-by-side method was selected.15-20
The main causes of occlusion in SEMSs are tumor ingrowth, tumor overgrowth and the development of granulation tissue within the stent. A major limiting factor of SEMS is that once placed, SEMS may be difficult to remove and can only be removed surgically. Another disadvantage of SEMS is the greater cost relative to plastic stents. However, metal stent insertion not only offers higher patency rates compared to plastic stent insertion, but is also cost-effective since patients require fewer reinterventions. Metal stents may be considered as an initial intervention in patients with nonresectable malignant HBSs.2,21,22 With regard to cost-effectiveness, the use of metal stents should be restricted to those patients with nonresectable tumors who will, in all probability, live longer than three months, and in those patients who are planning to undergo chemotherapy or additional palliative therapy.23 However, there is not a good way to predict life expectancy. According to Asia-Pacific consensus recommendations in 2013, in Bismuth II-IV HBS patients with a predicted survival of longer than 3 months, metallic stent performance is superior to plastic stenting for palliation in terms of outcomes and cost-effectiveness.24
There is currently no consensus on the best option for an endoscopic method with regard to bilateral versus unilateral placement of stents in patients with nonresectable malignant HBSs. Single (unilateral) stents may be adequate for Bismuth type I hilar tumors, which have strictures of the main bile duct below the confluence. However, there is significant controversy as to whether single or multiple stents (unilateral versus bilateral) should be inserted for Bismuth type II or higher tumors. The decision on whether to place single or multiple biliary stents depends on the location and extent of the stricture in the biliary tract, as well as the degree of biliary contamination.1
A single biliary stent in one functional liver lobe for unilateral drainage can provide adequate palliation in the majority of patients with HBSs. It is well known that only 25% of the liver volume requires drainage for adequate palliation of obstructive cholestasis in order to see improvement in biochemical parameters.16 Approximately 55% to 60% of the liver volume is drained via the right hepatic duct, 30% to 35% by the left hepatic duct, and 10% from the caudate lobe. No significant difference was found in terms of successful drainage, complications, number of endoprosthesis changes and survival between patients with right duct drainage compared with those with left side drainage.25 De Palma et al.26,27 reported that unilateral metallic stent insertion is safe, feasible, and achieves adequate drainage in a great majority of patients with nonresectable hilar cholangiocarcinoma. Successful stent insertion was achieved in 59 of 61 (96.7%) patients. Stent malfunction occurred in only three of 61 (4.9%) cases. Successful drainage was achieved in 59 of 61 (96.7%) patients and complete resolution of jaundice occurred in 86% of cases. Compared with bilateral drainage, unilateral stents had a significantly higher rate of successful endoscopic stent insertion than bilateral stents (88.6% vs. 76.9%; p=0.041). Also, unilateral stents had a significantly lower rate of complications than bilateral stents (18.9% vs. 26.9%; p=0.026). They concluded that the insertion of more than one stent is not justified as a routine procedure in patients with biliary bifurcation tumors.26,27 Previous studies also suggested that more than one endoprosthesis would not be justified as a routine procedure in patients with malignant HBSs. Unilateral stent insertion with either a metal or plastic stent may have a significantly higher rate of technical success, lower complication rate, and higher rate of successful drainage compared with bilateral stent insertion.25-29 Iwano et al.29 showed that unilateral drainage is associated with a lower incidence of liver abscess, as well as a comparable outcome with regard to stent patency and complication-free survival compared with bilateral drainage. These findings are the result of inadvertent contrast injections into the undrained bile ducts. The results clearly show that failure to drain an opacified lobe leads to a significantly negative outcome, thus bilateral drainage is mandatory if both hepatic lobes are opacified. The incidence of cholangitis in patients with a hilar obstruction was significantly higher than those with a distal obstruction.30 An unsuccessful attempt at bilateral drainage can lead to increased incidence of post-procedure cholangitis and lower survival rates. Selectively targeted and planned endoscopic drainage guided by magnetic resonance cholangiography or computed tomography imaging has been introduced to reduce inadvertent contrast injections into atrophied and/or unintended multiple hepatic segments, which results in a lower incidence of postprocedure cholangitis.27,30-33
Although bilateral biliary drainage may be controversial in the management of malignant HBSs, bilateral drainage remains a reasonable option in preserving the functional volume of the liver. In addition, an increased risk for cholangitis or septicemia has been associated with unilateral drainage. Bilateral biliary stents may be needed for palliative drainage of both hepatic lobes when both sides are contaminated, when a nondominant or atrophic lobe was inadvertently stented without efficacy, or if bilateral brachytherapy is scheduled. Accordingly, bilateral drainage may be more physiologically sound than unilateral drainage, and various bilateral drainage techniques and newly developed metallic stents are now available.34-36 Chang et al.34 found that the greatest survival rates in patients with bifurcation tumors were among those who underwent bilateral drainage, and the worst survival rates were among those with cholangiographic filling of both lobes, but drainage of only one. Naitoh et al.35 also showed a higher cumulative stent patency in the bilateral stent group.
Asia-Pacific consensus recommendations in 2013 suggest that the goal of palliative stenting of hilar cholangiocarcinoma is drainage of adequate liver volume (50% or more), irrespective of unilateral, bilateral, or multisegmental stenting. Draining more than 50% of liver volume frequently requires more than one stent, whether bilateral stenting or multisegmental stenting, which depends on the individual anatomy.24 In addition, atrophic segment and aberrant ductal anatomy need to be assessed by noninvasive imaging before attempting biliary drainage.37 If predicted survival is longer than 3 months, metallic stents are preferred. In Bismuth type II, if liver volume cannot be drained more than 50% by one stent, biliateral endoscopic drainage is more preferred; in Bismuth type III/IV, however, biliateral or multisegmental drainage by precutaneus approach is more preferred than endoscopic approach.24 However, when viewed from the perspective of the experienced endoscopists, bilateral drainage by metallic stents is technically feasible and was revealed to have higher technical and functional success rate in recent reported studies. So, if appropriate endoscopic expertise is available, endoscopic palliation can be suggested as the first treatment of choice even for high grade Bismuth type III or IV strictures.
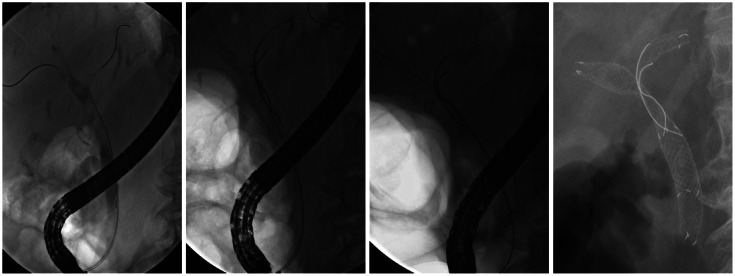
Bilateral biliary drainage using metallic stents for malignant HBSs can be performed with side-by-side or stent-in-stent method. After the initial stenting of the intrahepatic duct in one segment (or side), a second stent can be placed either using a "side-by-side" method (Fig. 1); parallel to the initial stent, or using "stent-in-stent" method (Fig. 2); or by crossing through the mesh within the initial stent.24 However, the technical challenges of metallic stent insertion for bilateral drainage may limit its use. Bilateral metallic stents placed by experienced endoscopists have an increased technical and functional success rate when compared with unilateral stents; however, bilateral stents do have an increased risk of complications when the placement fails. As a result, some endoscopists may hesitate to insert bilateral metal stents. The overall technical success rates for experts in stent-in-stent and side-by-side procedures range from 73.3% to 100% (Table 1).15,18,38-45
Bilateral side-by-side stent placement for HBS has frequently been performed using an endoscopic approach and parallel arrangement, as reported by Cheng et al.38 and Dumas et al.39 The issues surrounding this technique include the potential entanglement of the two guidewires, the difficulty of precise deployment to ensure adequate drainage, and endoscopic revision when the stents occluded.3 After deployment of the first SEMS, inserting the second delivery system may be difficult due to impaction or resistance of the second delivery catheter against the first deployed SEMS. Technically rapid insertion after preloading on guidewire may be helpful, and small diametered and good pushability delivery systems are needed. Both SEMS should be placed with their distal end in the duodenum or at the same level in the CBD to facilitate SEMS revision when stents occluded. For overcoming these difficulties, Chennat and Waxman40 introduced a thin, 6 Fr delivery system. It showed a higher rate of technical success and they concluded that this system was feasible and ideal for use in simultaneous side-by-side deployment. However, the authors noted that the handling of this side-by-side simultaneous system within the endoscopic working channel and biliary duct resulted in additional frictional forces that could be problematic and may increase the tendency of the stent delivery system to buckle in the distal duct. Furthermore, the duration of stent patency (130 days) was relatively short, due to the brevity of the follow-up period.
In bilateral stent-in-stent procedures, the use of a guidewire to cannulate to the desired contralateral duct through the preexisting SEMS may be difficult. Also, in endoscopic revisions for stent occlusions due to tumor ingrowth, the previously inserted wire mesh of the stent may preclude the insertion of revisionary stent. To facilitate second SEMS insertion, balloon dilation of contralateral hepatic duct immediately before the first stenting or dilation of first deployed SEMS by balloon before inserting the contralateral second SEMS can be useful.15,41 Large open-celled wire mesh stents can provide a high technical success rate in those cases; however, expanding radial forces may decrease in stricture sites and may have an inherent weakness to tumor ingrowth due to the large open mesh design. Also, full expansion of the second stent may be limited because of the space limitation though the large open mesh. Recently, cross-wired metallic stents for endoscopic bilateral stent-in-stent placement in malignant HBSs showed higher technical success and revision efficacy. This stent had the conventional hook and cross-wired structure on the proximal and distal portions. However, on the 25-mm-long central portion, this stent had only the cross-wired structure to facilitate placement of the contralateral stent across it. The primary technical success rate of endoscopic bilateral stent-in-stent placement of cross-wired metallic stents was 95.2% and median patency was 238 days. The technical and clinical success rates of planned bilateral endoscopic revision for occluded stents were 83.3% (20/24) and 79.2% (19/24), respectively.45 In general, the overall success rate of endoscopic revisions varied from 44.4% to 100%.18,19,38-45 These studies used various combinations of unilateral or bilateral stent placement, side-by-side or stent-in-stent insertion methods, without a comparative analysis because of the limited number of patients. The variations among these studies prohibit a direct comparison of the results. Nevertheless, newly developed or modified stents and devices recently did show a higher technical feasibility without increased complications. The results may encourage endoscopic retrograde cholangiopancreatography endoscopists to use these techniques and stents as soon as possible in order to overcome difficulties.
For the effective endoscopic biliary drainage, the selection of the appropriate stent according to the patient's condition and anatomical position is important. Also, acknowledgement and understanding of the advantages, disadvantages, and complications according to each type of stents are needed. Especially, endoscopic palliation of inoperable malignant HBSs is technically difficult and there is a lack of a clear consensus on the use of plastic versus metal stents and unilateral versus bilateral drainage. Recent Asia-Pacific consensus recommendations suggested that bilateral stent-in-stent or side-by-side endoscopic drainage is more preferred in Bismuth type II, but bilateral or multisegmental drainage by percutaneus approach is more preferred in Bismuth type III/IV. However, recently developed metal stents and devices have become commercially available and several studies have reported higher technical feasibility and successful clinical outcomes of these stents endoscopically in Bismuth type III/IV. Palliative therapeutic strategies should be made on an individual basis such as experienced endoscopists, patient condition, or surrounding medical curriculum, till more acceptable results are found in randomized, controlled trials further evaluating these therapeutic issues.
References
1. Kim JH. Endoscopic stent placement in the palliation of malignant biliary obstruction. Clin Endosc. 2011; 44:76–86. PMID: 22741117.

2. Wagner HJ, Knyrim K, Vakil N, Klose KJ. Plastic endoprostheses versus metal stents in the palliative treatment of malignant hilar biliary obstruction. A prospective and randomized trial. Endoscopy. 1993; 25:213–218. PMID: 7686100.

3. Raijman I. Biliary and pancreatic stents. Gastrointest Endosc Clin N Am. 2003; 13:561–592. PMID: 14986787.

4. Maillot N, Aucher P, Robert S, et al. Polyethylene stent blockage: a porcine model. Gastrointest Endosc. 2000; 51:12–18. PMID: 10625788.

5. Speer AG, Cotton PB, MacRae KD. Endoscopic management of malignant biliary obstruction: stents of 10 French gauge are preferable to stents of 8 French gauge. Gastrointest Endosc. 1988; 34:412–417. PMID: 2460394.

6. Pedersen FM. Endoscopic management of malignant biliary obstruction. Is stent size of 10 French gauge better than 7 French gauge? Scand J Gastroenterol. 1993; 28:185–189. PMID: 8441913.

7. Kadakia SC, Starnes E. Comparison of 10 French gauge stent with 11.5 French gauge stent in patients with biliary tract diseases. Gastrointest Endosc. 1992; 38:454–459. PMID: 1511821.

8. van Berkel AM, Boland C, Redekop WK, et al. A prospective randomized trial of Teflon versus polyethylene stents for distal malignant biliary obstruction. Endoscopy. 1998; 30:681–686. PMID: 9865556.

9. England RE, Martin DF, Morris J, et al. A prospective randomised multicentre trial comparing 10 Fr Teflon Tannenbaum stents with 10 Fr polyethylene Cotton-Leung stents in patients with malignant common duct strictures. Gut. 2000; 46:395–400. PMID: 10673303.

10. Terruzzi V, Comin U, De Grazia F, et al. Prospective randomized trial comparing Tannenbaum Teflon and standard polyethylene stents in distal malignant biliary stenosis. Gastrointest Endosc. 2000; 51:23–27. PMID: 10625790.

11. Davids PH, Groen AK, Rauws EA, Tytgat GN, Huibregtse K. Randomised trial of self-expanding metal stents versus polyethylene stents for distal malignant biliary obstruction. Lancet. 1992; 340:1488–1492. PMID: 1281903.

12. Kaassis M, Boyer J, Dumas R, et al. Plastic or metal stents for malignant stricture of the common bile duct? Results of a randomized prospective study. Gastrointest Endosc. 2003; 57:178–182. PMID: 12556780.

13. Schmassmann A, von Gunten E, Knuchel J, Scheurer U, Fehr HF, Halter F. Wallstents versus plastic stents in malignant biliary obstruction: effects of stent patency of the first and second stent on patient compliance and survival. Am J Gastroenterol. 1996; 91:654–659. PMID: 8677925.
14. Pedersen FM, Lassen AT, Schaffalitzky de Muckadell OB. Randomized trial of stent placed above and across the sphincter of Oddi in malignant bile duct obstruction. Gastrointest Endosc. 1998; 48:574–579. PMID: 9852446.

15. Park do H, Lee SS, Moon JH, et al. Newly designed stent for endoscopic bilateral stent-in-stent placement of metallic stents in patients with malignant hilar biliary strictures: multicenter prospective feasibility study (with videos). Gastrointest Endosc. 2009; 69:1357–1360. PMID: 19481654.

16. Dowsett JF, Vaira D, Hatfield AR, et al. Endoscopic biliary therapy using the combined percutaneous and endoscopic technique. Gastroenterology. 1989; 96:1180–1186. PMID: 2925062.

17. Polydorou AA, Cairns SR, Dowsett JF, et al. Palliation of proximal malignant biliary obstruction by endoscopic endoprosthesis insertion. Gut. 1991; 32:685–689. PMID: 1711994.

18. Chahal P, Baron TH. Expandable metal stents for endoscopic bilateral stent-within-stent placement for malignant hilar biliary obstruction. Gastrointest Endosc. 2010; 71:195–199. PMID: 19945101.

19. Kawamoto H, Tsutsumi K, Fujii M, et al. Endoscopic 3-branched partial stent-in-stent deployment of metallic stents in high-grade malignant hilar biliary stricture (with videos). Gastrointest Endosc. 2007; 66:1030–1037. PMID: 17963891.
20. Jarnagin WR, Fong Y, DeMatteo RP, et al. Staging, resectability, and outcome in 225 patients with hilar cholangiocarcinoma. Ann Surg. 2001; 234:507–517. PMID: 11573044.

21. Perdue DG, Freeman ML, DiSario JA, et al. Plastic versus self-expanding metallic stents for malignant hilar biliary obstruction: a prospective multicenter observational cohort study. J Clin Gastroenterol. 2008; 42:1040–1046. PMID: 18719507.
22. Raju RP, Jaganmohan SR, Ross WA, et al. Optimum palliation of inoperable hilar cholangiocarcinoma: comparative assessment of the efficacy of plastic and self-expanding metal stents. Dig Dis Sci. 2011; 56:1557–1564. PMID: 21222156.

23. Stern N, Sturgess R. Endoscopic therapy in the management of malignant biliary obstruction. Eur J Surg Oncol. 2008; 34:313–317. PMID: 18276101.

24. Rerknimitr R, Angsuwatcharakon P, Ratanachu-Ek T, et al. Asia-Pacific consensus recommendations for endoscopic and interventional management of hilar cholangiocarcinoma. J Gastroenterol Hepatol. 2013; 28:593–607. PMID: 23350673.

25. Polydorou AA, Chisholm EM, Romanos AA, et al. A comparison of right versus left hepatic duct endoprosthesis insertion in malignant hilar biliary obstruction. Endoscopy. 1989; 21:266–271. PMID: 2482169.

26. De Palma GD, Galloro G, Siciliano S, Iovino P, Catanzano C. Unilateral versus bilateral endoscopic hepatic duct drainage in patients with malignant hilar biliary obstruction: results of a prospective, randomized, and controlled study. Gastrointest Endosc. 2001; 53:547–553. PMID: 11323577.

27. De Palma GD, Pezzullo A, Rega M, et al. Unilateral placement of metallic stents for malignant hilar obstruction: a prospective study. Gastrointest Endosc. 2003; 58:50–53. PMID: 12838220.

28. Sherman S. Endoscopic drainage of malignant hilar obstruction: is one biliary stent enough or should we work to place two? Gastrointest Endosc. 2001; 53:681–684. PMID: 11323609.

29. Iwano H, Ryozawa S, Ishigaki N, et al. Unilateral versus bilateral drainage using self-expandable metallic stent for unresectable hilar biliary obstruction. Dig Endosc. 2011; 23:43–48.

30. Nomura T, Shirai Y, Hatakeyama K. Cholangitis after endoscopic biliary drainage for hilar lesions. Hepatogastroenterology. 1997; 44:1267–1270. PMID: 9356838.
31. Freeman ML, Overby C. Selective MRCP and CT-targeted drainage of malignant hilar biliary obstruction with self-expanding metallic stents. Gastrointest Endosc. 2003; 58:41–49. PMID: 12838219.

32. Hintze RE, Abou-Rebyeh H, Adler A, Veltzke-Schlieker W, Felix R, Wiedenmann B. Magnetic resonance cholangiopancreatography-guided unilateral endoscopic stent placement for Klatskin tumors. Gastrointest Endosc. 2001; 53:40–46. PMID: 11154487.

33. Khan SA, Davidson BR, Goldin R, et al. Guidelines for the diagnosis and treatment of cholangiocarcinoma: consensus document. Gut. 2002; 51(Suppl 6):VI1–VI9. PMID: 12376491.

34. Chang WH, Kortan P, Haber GB. Outcome in patients with bifurcation tumors who undergo unilateral versus bilateral hepatic duct drainage. Gastrointest Endosc. 1998; 47:354–362. PMID: 9609426.

35. Naitoh I, Ohara H, Nakazawa T, et al. Unilateral versus bilateral endoscopic metal stenting for malignant hilar biliary obstruction. J Gastroenterol Hepatol. 2009; 24:552–557. PMID: 19220678.

36. Saleem A, Baron TH, Gostout CJ. Large-diameter therapeutic channel duodenoscope to facilitate simultaneous deployment of side-by-side self-expandable metal stents in hilar cholangiocarcinoma. Gastrointest Endosc. 2010; 72:628–631. PMID: 20579649.

37. Kwon AH, Uetsuji S, Ogura T, Kamiyama Y. Spiral computed tomography scanning after intravenous infusion cholangiography for biliary duct anomalies. Am J Surg. 1997; 174:396–401. PMID: 9337161.

38. Cheng JL, Bruno MJ, Bergman JJ, Rauws EA, Tytgat GN, Huibregtse K. Endoscopic palliation of patients with biliary obstruction caused by nonresectable hilar cholangiocarcinoma: efficacy of self-expandable metallic Wallstents. Gastrointest Endosc. 2002; 56:33–39. PMID: 12085032.

39. Dumas R, Demuth N, Buckley M, et al. Endoscopic bilateral metal stent placement for malignant hilar stenoses: identification of optimal technique. Gastrointest Endosc. 2000; 51:334–338. PMID: 10699784.

40. Chennat J, Waxman I. Initial performance profile of a new 6F self-expanding metal stent for palliation of malignant hilar biliary obstruction. Gastrointest Endosc. 2010; 72:632–636. PMID: 20579991.

41. Lee JH, Kang DH, Kim JY, et al. Endoscopic bilateral metal stent placement for advanced hilar cholangiocarcinoma: a pilot study of a newly designed Y stent. Gastrointest Endosc. 2007; 66:364–369. PMID: 17643714.
42. Kim JY, Kang DH, Kim HW, et al. Usefulness of slimmer and open-cell-design stents for endoscopic bilateral stenting and endoscopic revision in patients with hilar cholangiocarcinoma (with video). Gastrointest Endosc. 2009; 70:1109–1115. PMID: 19647244.

43. Hwang JC, Kim JH, Lim SG, Kim SS, Yoo BM, Cho SW. Y-shaped endoscopic bilateral metal stent placement for malignant hilar biliary obstruction: prospective long-term study. Scand J Gastroenterol. 2011; 46:326–332. PMID: 21082874.

44. Lee TH, Park do H, Lee SS, et al. Technical feasibility and revision efficacy of the sequential deployment of endoscopic bilateral side-by-side metal stents for malignant hilar biliary strictures: a multicenter prospective study. Dig Dis Sci. 2013; 58:547–555. PMID: 22886596.

45. Lee TH, Moon JH, Kim JH, et al. Primary and revision efficacy of cross-wired metallic stents for endoscopic bilateral stent-in-stent placement in malignant hilar biliary strictures. Endoscopy. 2013; 45:106–113. PMID: 23212727.

Fig. 1
Side-by-side deployment of metallic stents (Bonastent; Standard SciTech Inc.); sequential images of bilateral side-by-side stent placement in a patient with hilar cholangiocarcinoma (Bismuth type IIIA). The stricture was first negotiated with a guidewire inserted into the left hepatic duct, and the right hepatic duct was then accessed using the same method. Following the introduction of these two guidewires, the first stent (with a radiopaque X mark) was inserted in the left hepatic duct without removing the preloaded guidewire; the second stent was then deployed in the right hepatic duct using the same method.
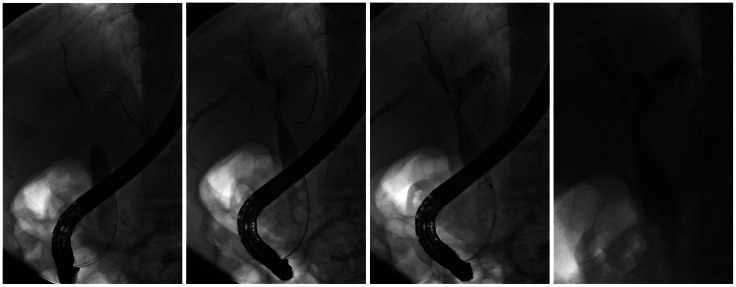
Fig. 2
Stent-in-stent deployment of metallic stents in Bismuth type IV (Bonastent; Standard SciTech Inc.); guidewires were initially introduced into both intrahepatic ducts bilaterally. The first stent with a radiopaque X mark was inserted into the left hepatic duct. After deployment of the first stent, the remaining guidewire was carefully withdrawn using an endoscopic retrograde cholangiopancreatography catheter, without pulling it back completely. The guidewire was then inserted into the right hepatic duct through the central portion of the first stent. Following deployment of the second stent, the bilateral metal stents were in a Y-configuration.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download